You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The maxillary canine is a critically important tooth because of its morphology, arch position, protective function through canine guidance, and role in smile esthetics.1 Proper final position of the canine in the arch is considered a key to long-term stability.2
An impacted tooth is one that has not erupted as a consequence of a blockage due to a physical barrier such as another tooth, an enlarged cyst, bone, soft tissues, a supernumerary tooth, an odontoma, or a tumor.2 Mandibular third molars are the most common impacted teeth, followed by maxillary permanent canines. In order to erupt, the maxillary canines must travel a long distance from the lower border of the orbit into the arch, and they are also the last anterior teeth to erupt.3 The prevalence of impacted maxillary cuspids is around 2%.3 Females present with impacted cuspids two to three times more often than males. About two-thirds of impactions are palatal and one-third are buccal, with bilateral impactions having a prevalence of 8%.3,4 Latin America has a prevalence similar to Europe or the United States, with reports coming from Colombia,5 Mexico,2 and Brazil,6 among other countries. Some countries, such as Greece and Turkey, however, show a higher prevalence of close to 4%.7
Impaction can displace a tooth as a result of physical pressure, the presence of a cyst, root resorption (which is more common in maxillary lateral incisors that present conical roots palatally oriented, but also can be seen in maxillary central incisors), local and referred pain, and inflammatory disorders.4-8 Clinicians must be aware that there may be a difference of up to 6 months between chronologic and eruption age for the maxillary canine to rule out agenesis or impactions.9 To only observe an impacted canine without intervention after age 12 will most likely not resolve the situation.10 Early diagnosis and intervention helps ensure easier occlusal management later.11 If early interventions are unsuccessful, an interdisciplinary surgical orthodontic solution will be needed.9
Causes of Impaction
Potential causes of impacted teeth as proposed by Becker and Chaushu et al include: an enlarged dental follicle, odontoma, unerupted tooth on the pathway, contact with the adjacent tooth, periapical pathology on the pathway, delayed eruption of the adjacent tooth, and the absence or presence of a peg lateral.4,12 Three sets of criteria should be considered for the proper assessment of impacted canines: diagnostic principles, treatment planning, and biomechanics principles. The former encompasses all of the diagnostic measures (both clinical and imaging) needed to facilitate a sufficient assessment of the problem. Treatment planning refers to the communication between the orthodontist and oral surgeon to attain adequate exposure. Biomechanics involves the efficient planning of orthodontic force vectors for correct clinical management.
Bishara divided causes of impaction into general and local categories.13 Among the general causes are alterations within the thyroid gland, hypovitaminosis A and D, febrile and infectious diseases, radiation, and syndromes such as Crouzon and Down. Local mechanical conditions commonly considered as causes of impaction are supernumerary teeth, odontomas, traumas at an early age, cleft lip, and cleft palate.4-8 Other suggested causes include anomalies in morphology or position of the tooth germ, alterations in the pathway of the canine, periodontal ligament (PDL) ankylosis, prolonged retention or early loss of primary canines, iatrogenesis, root dilaceration, and idiopathic factors.13
It is generally agreed that a particularly specific reason for buccally impacted maxillary canines is lack of space or an arch length deficiency.8-14 Tomographic studies have shown a relationship between narrow maxillary arches and buccal impactions. Such a relationship has not been reported for palatal impactions in the permanent dentition.14,15 Jacobs reported a tooth size discrepancy for impacted buccal canines.16 The canines are more apt to be impacted because of their relatively long path to eruption.
Becker proposed that palatally impacted canines are a result of a lack of guidance of the lateral incisor root, in cases of either missing or morphologically deformed lateral incisors.4 Other authors, on the other hand, proposed a common genetic cause between palatal impacted canines and other dental anomalies, such as missing or microdontic maxillary lateral incisors, enamel hypoplasia, infraerupted temporary molars, or a mandibular second bicuspid with a distally altered eruption pattern.3,17-20 Peck et al stated that palatal impaction should be seen as part of a broader view of chromosomic alterations.3
Surgical/Orthodontic Decision Tree
To assist clinicians in determining the optimal treatment of an impacted maxillary canine, a surgical/orthodontic decision tree is presented in Figure 1.
Diagnosis of Canine Impaction
The diagnostic process must follow a logical sequence and should incorporate a thorough patient account of family history of dental anomalies17,18 combined with a comprehensive clinical examination. The examination should include palpation complemented with basic radiologic initial screening x-rays such as panoramic,2 lateral cephalic,21 and upper occlusal. These x-rays should be supplemented with periapical projections using the Clark technique22 even though the panoramic x-ray is a more cost-effective initial screening tool.23
To obtain more information with greater detail, a volumetric study such as a cone-beam computed tomography (CBCT) is often indicated. This advanced imaging technology may be used for the assessment of root resorption in adjacent teeth,24,25 possible transpositioning between the maxillary lateral incisor and canine or in maxillary canines erupting just above the apexes of the lateral incisors,26,27 root dilacerations, and ankylosis.8 Regarding root resorption, Ericson and Kurol reported that, based on tomography, 38% of maxillary lateral incisors and 9% of maxillary central incisors presented important root resorption in relation to impacted canines (Figure 2 and Figure 3).24
CBCT Technology and Impacted Canines
A valuable radiological diagnostic tool, CBCT imaging is indicated depending on information obtained from clinical examination and must be justified based on the individual patient needs.28 This means that CBCT should not be the first method of imaging used in cases where there is no clinical suspicion of an impacted canine. Localized CBCT imaging is justified only after a clinical assessment is performed and when other radiological imaging is inconclusive.
Although intuitively one might think that CBCT imaging is better than 2-dimensional (2D) imaging in cases involving impacted canines, this assumption has not been fully tested. Systematic reviews that have compared diagnostic performances to determine impacted canines using CBCT versus conventional imaging have shown that although CBCT imaging facilitates more consistency in diagnoses and initial management decisions, clinician opinions still vary. In other words, this mode of imaging does not eliminate differences in personal management preferences. In this regard, panoramic radiography may suffice in many cases.29 A relatively similar conclusion was proposed when comparisons were made for impacted canine angulation and position; although the study concluded that CBCTs provide more precise positions and fewer agreement inconsistencies and enable a greater variety of treatment plans, lack of evidence was noted in regard to actual impact on patient-oriented outcomes (eg, treatment time, pain levels, etc).30 In summary, there is no robust evidence stating that CBCT should be the first-line imaging method for impacted canines, although it may well be indicated when 2D imaging is inconclusive.
Open or Closed Surgical Technique?
In a systematic literature review analyzing impacted cuspids that were high in the palate, Parkin et al concluded there was no significant evidence to favor either open surgical or closed eruption.31 Neither technique provided strong evidence of better outcomes regarding gingival esthetics, oral health, and patient comfort. They recommended further randomized clinical trials.
Sampaziotis et al, in another systematic literature review comparing both surgical techniques for palatal impacted cuspids, concluded there was no difference in periodontal outcome or esthetic appearance.32 Post-surgical pain was similar. The procedure with the open surgical exposure technique was reported to be shorter, however the authors' conclusions were drawn based on only two studies that met their inclusion criteria.
In a systematic review with a meta-analysis comparing both techniques, Cassina et al concluded the open exposure technique had a lower risk of ankylosis and shorter traction time.33 Again, this review included only a small number of clinical trials. The researchers also recommended that a larger number of randomized clinical trials was needed in order to make clinical recommendations.
A disadvantage of the closed eruption technique is that if the orthodontic attachment becomes loose, more surgery is required. Because the tooth is inside the tissue, the vector of force is harder to control,34 and traction is a blind movement.35 There is also an increased risk of ankylosis reported with the closed eruption technique.34,35 For these reasons, some authors prefer the open surgical approach.34-36 In summary, however, presently there is no clear consensus on which surgical approach is indicated.
Space Considerations in Early Management of Impacted Canine
Extraction of a primary canine is a simple measure for prevention and early management of canine impaction.37 It can be used alone or in conjunction with space maintenance appliances, such as Nance buttons or transpalatal arches,16,38 or space gaining appliances. Jacobs described the importance of correcting space deficiencies in the maxillary arch.16 Baccetti et al noted the importance of early palatal expansion in the mixed dentition as a preventive method for palatal impacted canines.38 Palatal expansion is a reproducible, cost-effective method for augmenting arch width and avoiding further problems.8
Pediatric dentists should indicate a panoramic x-ray for patients between 7 and 11 years old.26 This basic practice is helpful in determining the proximity of the crown of the canines in relation to the roots of lateral and central incisors.39 Many situations improve with the extraction of the primary canine, even in cases of incipient lateral incisor resorption. However, early extraction of deciduous canines with or without arch increase measurements does not work all the time. A recent important randomized controlled trial by Naoumova and Kjellberg provided timely guidance as to when to extract deciduous canines.40 When the potentially impacted canine is in sector 2 (distal aspect of lateral incisor to midline of lateral incisor) or sector 3 (midline of lateral incisor to distal aspect of central incisor),37 and its relative inclination to a fictitious vertical plane is between 20 and 30 degrees, then the early extraction of the deciduous tooth is indicated. In cases where the inclination is less than 20 degrees or more than 30 degrees, the early extraction of the deciduous cuspid will not significantly affect the permanent canine impaction. The same applies to impacted canines in sectors 1 (deciduous canine), 4 (distal aspect of central incisor to midline of central incisor), or 5 (midline of central incisor to midline of maxillary arch).40
It is necessary to surgically expose the canine and direct it away from nearby roots. Moving the canine first palatally or buccally, depending on the case, and then distally has been suggested.26 Another recommendation in patients with severe crowding is to verify that the impacted canine responds to traction before a decision is made on whether to extract a premolar.26,34
Anchorage Considerations in Impacted Teeth
For the traction of impacted teeth it is important to have either a rectangular base stainless steel archwire or thick transpalatal bar with adequate rigidity. This is especially critical in palatally impacted canines. Avoiding the use of flexible archwires can allow for better control of adverse effects on adjacent teeth during traction.34,35 Sufficient intra-arch anchorage can be obtained, working up the sequence to .019 x .025 wires in a .022 slot. This prevents deformed archwires, bite opening from traction, intrusion to adjacent teeth, and other related adverse effects.34,35
Various external elements, such as swinging gates, transpalatal arches, Hass expanders, quad helixes, Hyrax expanders, and temporary anchorage devices (TADs), have been used as alternative anchorage apparatuses. In the case of a transpalatal bar, the objective is to use cantilever extension arms to traction the impacted canine into the palate. This is followed by traction of the canine into its final position using positioning springs or other methods to bring the impacted tooth into the dental arch (Figure 4 and Figure 5).
Considerations During Activation of Impacted Canines
Vectors of force must be applied that allow the canine to be moved away from the root of adjacent teeth, especially in cases where there is a close relationship between the canine and lateral incisor.26,35 Very deeply impacted palatally displaced canines should be activated first occlusally, and in many instances distally, before being moved to the desired position in the arch.9,27 Auxiliaries such as power chains, elastic thread, nickel titanium coils, auxiliary extrusion springs, ballista springs, cantilever arms, and TADs can be used.26,41
When ankylosis is suspected, traction force should be reduced, and the patient should be referred to a periodontist. In such instances, a simple periapical (PA) x-ray is recommended to determine the presence of osteoid tissue to ensure that the periodontal tissue is following the tooth in its movement.34,35
Treatment Time With Impacted Canines
In an evaluation of duration of orthodontic treatment, Fink and Smith analyzed six private orthodontic practices with 118 patients and concluded the average orthodontic treatment time was 23.1 months with a range from 19.4 to 27.9 months in patients without impacted canines.42 Another study measured treatment time in cases of adolescents with palatal impacted canines managed with closed eruption. For unilateral cases, average treatment time was 25.8 months, while for bilateral cases, it was 32.3 months.43 A similar study was done with adults with palatal impactions managed with the closed eruption technique. It concluded that although the treatment did not last long, it required more visits. Adult cases had a success rate of 69.5% compared to 100% successfully resolved cases in adolescent patients. Another interesting finding was that all the cases where the canine was unsuccessfully positioned in the arch involved patients older than 30 years of age.44
The orthodontist is often faced with an impacted canine and the need to create adequate space to facilitate movement prior to surgical exposure. This requires full-sized arches to be engaged in brackets before the tooth is exposed and may take 2 to 4 months.27
Periodontists or oral surgeons are often consulted to evaluate and surgically expose the impacted canine. A clinical and radiographic examination is performed to identify the location of the tooth, which can be verified by three different methods:palpation, radiography, and transgingival probing.45 Palpating the unerupted canine prominence allows the clinician to feel a hard, well-circumscribed area; this will be the location of the impacted tooth.45 If this bulge cannot be detected, radiographic evaluation may be needed.13,46 Lateral, occlusal, panoramic, or PA images have been utilized to determine impacted tooth location.37 The SLOB rule (same-lingual, opposite-buccal) is used with two different radiographs by changing the horizontal angle of the tube head while maintaining the film position of the impacted canine.47 CBCT is also considered a highly accurate imaging technique for determining the canine position.37
Facially Impacted Canine Surgical Techniques
One-third of impacted canines are in a facial relationship.4,8 Two techniques may be used for the management of facially impacted canines.45,48
Gingivectomy-Gingivectomy is the excisional removal of gingival tissue.45 The tip of the canine should be at or below the mucogingival junction (MGJ).48 This procedure is indicated if there is a wide zone of keratinized gingival tissue. The procedure is performed with either a Kirkland knife or 15 blade with an external bevel.27,45,48If the tip of the canine is located coronal to the cementoenamel junction (CEJ) of the lateral incisor, then gingivectomy can be performed.27 Upon completion of the procedure, at least 3 mm of keratinized gingival tissue should be apical to the CEJ.27,48At least two-thirds of the clinical crown should be exposed to permit placement of the bracket.27 A disadvantage of this technique is the need to repeat the procedure if the gingival tissue regrows, and it cannot be performed if there is an inadequate zone of keratinized gingiva.48
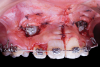
Apically repositioned flap-This technique is an option when there is not enough keratinized gingival tissue, and it is the preferred surgical procedure when the impacted canine is mesial to the lateral incisor.27,48 The flap must be secured and adapted to the tooth. Contraindication for this technique is risk of gingival recession and uneven gingival margin and the need for extensive osseous surgery.48 The flap is made by an incision with a 15 or 15c blade on the ridge to obtain the maximum amount of keratinized gingival tissue.27,45,48 Vertical incisions are performed, and the flap is moved in a lateral or apical direction.8 A flap design is recommended in which the base and the coronal zone are either the same width or narrower at the base, with a thickness of 4 mm to 5 mm, so the flap can be wide enough mesiodistally, extending 1.5 mm beyond the angle of the tooth (Figure 6 and Figure 7).8,35,36 Any bony shell covering the tooth should be removed with a curette or diamond bur to expose the coronal portion of the crown.8 The flap is then positioned at the CEJ and secured with periosteal sutures to obtain greater stability. Depending on the degree of canine impaction, a periodontal dressing can be placed so the tissue does not close.8,35,36 The bracket is placed either at the time of the procedure or 10 days after.35 If the impacted canine is too apical, the closed technique is performed.26,35 Generally, orthodontic movement begins 4 to 6 weeks after the surgical exposure.26 When a wide follicle surrounds the canine, the flap incision should be made wider than the follicle to permit optimum adaptation of the flap to the crown and bone. To determine if the flap is well adapted, when the lip moves the flap should remain stationary.8,35,36
Palatally Impacted Canine Surgical Techniques
Two surgical techniques can be utilized to achieve palatine canine exposure: open exposure with a trapezoidal or semilunar flap, or closed exposure.27,49
Open exposure-A semilunar internal bevel incision is made with a 15 or 15c blade along the mesio-palatal portion of the tooth, continuing to the disto-palatal area. A bevel incision should be performed toward the bone.49 A full-thickness flap is elevated with periosteal elevators. The removal of the bony crypt is completed with curettes and rotary instruments. The follicle is carefully removed with curettes, and the canine is exposed.45 The bony crypt is sufficiently exposed to permit proper positioning of the bracket. The bracket is placed, and a wire is tied to it. Bleeding in the area is controlled with the use of local anesthesia, bone wax, or gauze impregnated with 1:50,000 anesthesia.45 A new 15c blade is used to fenestrate the gingival tissue at the bracket location and create a trap door exposing the bracket through the flap, which is secured with sutures.49 The use of a periodontal dressing in the area is optional.8,45,48,49 Orthodontic forces are applied 2 weeks later in cases where direct traction is desired.27 It has been suggested to allow spontaneous eruption to the occlusal plane after the open exposure, and then direct the canine bucally (Figure 8 and Figure 9).9,26,27
Closed exposure-In this procedure, an intrasulcular or crestal incision is performed with a 15 or 15c blade from the bicuspid to the midline.27 A full-thickness flap is elevated with a periosteal elevator to expose the impacted canine. Any remnant tissue and the bony crypt is gently removed with hand and rotary instruments.26 A bracket is placed, a wire is tied in, and the flap is repositioned back and sutured.26,27 A suggested advantage of this approach is gingival esthetics. A disadvantage is possible bracket detachment due to the lack of a dry field at the time of bracket placement and, thus, the need for surgical re-exposure.2,48
Complications in Surgical/Orthodontic Impacted Teeth
Complications that orthodontists may encounter in the treatment of impacted teeth include devitalizations, second exposures, ankylosis, damage to adjacent teeth, and external radicular root resorption.35 An adequate treatment protocol allows for the preservation of the periodontal attachment.35
To date, there are no studies that explain the difference in response between adolescents and adults. It has been suggested that the PDL around the unerupted canine atrophies in older patients making movement slower and less predictable.26 Use of CBCT allows for the evaluation of the PDL and root morphology.8 In cases of absence of ligament space or presence of an apex in the form of a hook, further analysis is required to rule out spot (partial) or total ankylosis.35 The incidence of ankylosis increases with age and worsens the prognosis of the impacted canine solution.34,35 Patients should be informed of the risks and benefits of treatment of ankylosed canines so they can be able to decide whether the best course of action is to attempt luxation and traction or consider other possibilities such as extraction and placement of a future implant.26
Unfavorable Periodontal Reactions
An appropriate surgical technique is critical for the management of soft tissues and periodontal response.50,51 Rapid movement, heavy forces, and poor oral hygiene all play a role in poor responses.8 Marginal bone loss, gingival recession, and sensibility are complications of prolonged treatment.34,35 While some clinicians propose the use of perforations and tunnels for shorter treatment time,52 others consider this periodontally unacceptable. This is because if, for some reason, the canine cannot be placed in the arch, the patient will likely be left with a periodontal defect, which could require grafting and other procedures if the canine is to be substituted with an implant.35
Root Resorption of the Impacted Canine and/or Adjacent Teeth
In normal orthodontic treatment without impacted canines, a factor associated with root resorption is prolonged orthodontic treatment.53,54 Maxillary and mandibular anterior teeth are more commonly prone to develop root resorption than other teeth. Other factors related to root resorption are anterior retraction, extraction of teeth, heavy orthodontic forces, and altered apex root forms.41
Remington et al observed a large group of patients without impactions 10 years out of treatment. They concluded that once treatment stops, root resorption does not progress if it was related to tooth movement.55 Ericson et al reported that the chance of root resorption on maxillary laterals in females was three to four times greater compared to males in cases of impacted cuspids.24,56 The diagnosis of root resorption with CBCT is more accurate in these patients. An increase in the detection of root resorption was reported in more than 50% of CBCTs compared to 2D images.24
The mechanism of root resorption in adjacent lateral and central incisors is not totally established. The involvement of the cuspid follicle in root resorption is more controversial.57 Researchers have suggested that the pressure produced by the erupting canine and/or changes induced by the active and enlarged cuspid dental follicles are possible causes.56,57 Yan et al, in a tomographic study, reported physical proximity of less than 1 mm between the impacted canine and the roots of adjacent teeth to have a strong correlation with root resorption.58 Dağsuyu et al did not find an association between follicle size and lateral incisor resorption.57 Still, they reported more asymmetric and larger follicles in impacted canines close to resorbed laterals. Chaushu et al, on the other hand, reported root resorption in adjacent teeth of canines with follicles larger than 2 mm.12
When root resorption (even without half of the root of the canine formed) is present in the lateral incisors in patients between 9 and 10 years old, it is recommended that canine exposure be performed and the canine removed from the proximity of the root of the lateral incisor. Once the canine is in a distant and safe place from the lateral incisor, the orthodontic force on it should be stopped to allow the tooth to complete its root formation.35 Removing the impacted canine from the area of resorption on the lateral incisor has been shown to permit the deposit of secondary cement over the exposed dentin. This may produce a form of tooth repair.24
The presence of pre-existing root resorptions in the buccal or palatal aspects of lateral incisors should be documented before treatment is started to establish that the pre-existing condition is not a consequence of treatment, even though, in cases with significant root resorption, it is rare to lose a lateral and/or central incisor.26 Vermette et al found shorter roots post-treatment in cases with impacted canines that were brought to the arch.54 The cases that present the most root resorption are those of canines impacted in the middle of the ridge; yet, in many cases, the lateral incisor root moves away from the canine, and root resorption is avoided.26
Summary
Although maxillary impacted canines are a relatively uncommon problem in the general population, the frequency is perceived as high. Maxillary impacted canines require a complete set of clinical and imaging diagnoses to improve efficiencies during treatment planning. Early intervention through deciduous canine extractions and space gaining mechanics can intercept some cases that may otherwise lead to impactions, depending on the canine location relative to the ipsilateral anterior teeth. If early management is not successful, surgical orthodontic treatment will be required to bring the canine into the arch.
Orthodontic and surgical protocols have been described for buccal and palatal impacted canines. Clinicians should decide on the best approach for the management of impacted canines based on the available evidence. For buccal impacted canines, the position relative to the MGJ is critical for deciding on which surgical procedure to use. In these instances, three techniques can be used, depending on the tooth position: gingivectomy, apically positioned flap, or closed eruption. For palatal impacted canines, the open approach has several advantages relative to the closed eruption technique. However, the closed technique has clear indications.
Use of proper orthodontic mechanics, along with adherence to basic biomechanics principles, likely reduces the risks of treatment complications. Three critical factors are preparation of efficient anchorage on the maxillary arch, use of an effective bonding technique for the orthodontic attachment, and application of appropriate force vectors to traction the canine into the arch. Possible treatment complications of impacted canines include ankylosis of the tooth, root resorption of the tooth or adjacent teeth, gingival esthetic shortcomings in the treated canine relative to the contralateral canine, and extended treatment times.
About the Authors
Miguel Hirschhaut, DDS'
Private Practice limited to Orthodontics, Caracas, Venezuela; Adjunct Professor of Orthodontics, Universidad Central de Venezuela, Caracas, Venezuela
Nelson Leon, DDS
Private Practice limited to Oral and Maxillofacial Surgery, Caracas, Venezuela
Howard Gross, DDS, MS
Private Practice limited to Periodontics and Implant Dentistry, Lansdale, Pennsylvania
Carlos Flores-Mir, DDS, DSc
Professor, Division of Orthodontics, Department of Dentistry, University of Alberta, Edmonton, Alberta, Canada; Part-time Private Practice limited to Orthodontics, Edmonton, Alberta, Canada
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Bjerklin K. Orthodontic management of impacted maxillary canines. APOS Trends Orthod. 2020;10(2):64-71.
2. Ugalde MFJ, Gonzalez LR. Prevalencia de retenciones de caninos en pacientes tratados en la clínica de ortodoncia de UNITEC. Revista ADM. 1999;56(2):49-58.
3. Peck S, Peck L, Kataja M. Concomitant occurrence of canine malposition and tooth agenesis: evidence of orofacial genetic fields. Am J Orthod Dentofacial Orthop. 2002;122(6):657-660.
4. Becker A. Palatally impacted canines. In: The Orthodontic Treatment of Impacted Teeth. 3rd ed. West Sussex, United Kingdom: Wiley-Blackwell; 2012:110-172.
5. Castañeda Peláez DA, Briceño Avellaneda CR, Sánchez Pavón ÁE, et al. Prevalence of included, retained and impacted teeth, in panoramic radiographs of population from Bogotá, Colombia. Universitas Odontologica. 2015;34(73):149-158.
6. Pedro FL, Bandéca MC, Volpato LE, et al. Prevalence of impacted teeth in a Brazilian subpopulation. J Contemp Dent Pract. 2014;15(2):209-213.
7. Allareddy V, Caplin J, Markiewicz MR, Meara DJ. Orthodontic and surgical considerations for treating impacted teeth. Oral Maxillofac Surg Clin North Am. 2020;32(1):15-26.
8. Evans M, Tanna N, Chung CH. Management of impacted maxillary canines. In: Eliades T, Katsaros C, eds. The Ortho-Perio Patient: Clinical Evidence & Therapeutic Guidelines. Batavia, IL: Quintessence Publishing; 2019:121-160.
9. Kokich VG. Surgical and orthodontic management of impacted maxillary canines. Am J Orthod Dentofacial Orthop. 2004;126(3):278-283.
10. Sajnani AK. Permanent maxillary canines - review of eruption pattern and local etiological factors leading to impaction. J Investig Clin Dent. 2015;6(1):1-7.
11. Kurol J. Early treatment of tooth-eruption disturbances. Am J Orthod Dentofacial Orthop. 2002;121(6):588-591.
12. Chaushu S, Kaczor-Urbanowicz K, Zadurska M, Becker A. Predisposing factors for severe incisor root resorption associated with impacted maxillary canines. Am J Orthod Dentofacial Orthop. 2015;147(1):52-60.
13. Bishara SE. Impacted maxillary canines: a review. Am J Orthod Dentofacial Orthop. 1992;101(2):159-171.
14. Yan B, Sun Z, Fields H, et al. Etiologic factors for buccal and palatal maxillary canine impaction: a perspective based on cone-beam computed tomography analyses. Am J Orthod Dentofacial Orthop. 2013;143(4):527-534.
15. Al-Nimri K, Gharaibeh T. Space conditions and dental and occlusal features in patients with palatally impacted maxillary canines: an aetiological study. Eur J Orthod. 2005;27(5):461-465.
16. Jacobs SG. The impacted maxillary canine. Further observations on aetiology, radiographic localization, prevention/interception of impaction, and when to suspect impaction. Aust Dent J. 1996;41(5):310-316.
17. Garib DG, Alencar BM, Lauris JR, Baccetti T. Agenesis of maxillary lateral incisors and associated dental anomalies. Am J Orthod Dentofacial Orthop. 2010;137(6):732.e1-e6.
18. Garib DG, Alencar BM, Ferreira FV, Ozawa TO. Associated dental anomalies: the orthodontist decoding the genetics which regulates the dental development disturbances. Dental Press J Orthod. 2010;15(2):138-157.
19. Baccetti T. A controlled study of associated dental anomalies. Angle Orthod. 1998;68(3):267-274.
20. Peck S. Misleading article on palatally displaced canines. Am J Orthod Dentofacial Orthop. 2016;149(2):149-150.
21. Orton HS, Garvey MT, Pearson MH. Extrusion of the ectopic maxillary canine using a lower removable appliance. Am J Orthod Dentofacial Orthop. 1995;107(4):349-359.
22. Clark CA. A method of ascertaining the relative position of unerupted teeth by means of film radiographs. Proc R Soc Med. 1910;3(Odontol Sect):87-90.
23. Ericson S, Kurol J. Radiographic examination of ectopically erupting maxillary canines. Am J Orthod Dentofacial Orthop. 1987;91(6):483-492.
24. Ericson S, Kurol PJ. Resorption of incisors after ectopic eruption of maxillary canines: a CT study. Angle Orthod. 2000;70(6):415-423.
25. Kim Y, Hyun HK, Jang KT. The position of maxillary canine impactions and the influenced factors to adjacent root resorption in the Korean population. Eur J Orthod. 2012;34(3):302-306.
26. Kokich VG, Mathews DP. Labially impacted maxillary canines. In: Orthodontic and Surgical Management of Impacted Teeth. Hanover Park, IL: Quintessense Publishing; 2014:27-103.
27. Kokich VG, Mathews DP. Surgical and orthodontic management of impacted teeth. Dent Clin North Am. 1993;37(2):181-204.
28. American Academy of Oral and Maxillofacial Radiology. Clinical recommendations regarding use of cone beam computed tomography in orthodontics [corrected]. Position statement by the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116(2):238-257.
29. Eslami E, Barkhordar H, Abramovitch K, et al. Cone-beam computed tomography vs conventional radiography in visualization of maxillary impacted-canine localization: a systematic review of comparative studies. Am J Orthod Dentofacial Orthop. 2017;151(2):248-258.
30. Björksved M, Magnuson A, Bazargani SM, et al. Are panoramic radiographs good enough to render correct angle and sector position in palatally displaced canines? Am J Orthod Dentofacial Orthop. 2019;155(3):380-387.
31. Parkin N, Benson PE, Thind B, et al. Open versus closed surgical exposure of canine teeth that are displaced in the roof of the mouth. Cochrane Database Syst Rev.2017;8(8):CD006966.
32. Sampaziotis D, Tsolakis IA, Bitsanis E, Tsolakis AI. Open versus closed surgical exposure of palatally impacted maxillary canines: comparison of the different treatment outcomes - a systematic review. Eur J Orthod. 2018;40(1):11-22.
33. Cassina C, Papageorgiou SN, Eliades T. Open versus closed surgical exposure for permanent impacted canines: a systematic review and meta-analyses. Eur J Orthod. 2018;40(1):1-10.
34. Vanarsdall RL, Secchi AG. Periodontal-orthodontic interrelationships. In: Graber LW, Vanarsdall RL, Vig KWL, eds. Orthodontics: Current Principles and Techniques. 5th ed. St. Louis, MO: Elsevier Inc; 2011:647-659.
35. Vanarsdall RL. Orthodontics/periodontics. In: Graber TM, Graber LW, Vanarsdall RL, Vig KWL, eds. Orthodontics: Current Principles and Techniques. 3rd ed: St. Louis, MO: Mosby; 2000;822-836.
36. Vanarsdall RL Jr. Efficient management of unerupted teeth: a time-tested treatment modality. Semin Orthod. 2010;16(3):212-221.
37. Ericson S, Kurol J. Early treatment of palatally erupting maxillary canines by extraction of the primary canines. Eur J Orthod. 1988;10(4):283-295.
38. Baccetti T, Mucedero M, Leonardi M, Cozza P. Interceptive treatment of palatal impaction of maxillary canines with rapid maxillary expansion: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 2009;136(5):657-661.
39. Garib DG, Janson G, de Oliveira Baldo T, dos Santos PB. Complications of misdiagnosis of maxillary canine ectopic eruption. Am J Orthod Dentofacial Orthop. 2012;142(2):256-263.
40. Naoumova J, Kjellberg H. The use of panoramic radiographs to decide when interceptive extraction is beneficial in children with palatally displaced canines based on a randomized clinical trial. Eur J Orthod. 2018;40(6):565-574.
41. Maués CP, do Nascimento RR, de Vasconcellos Vilella O. Severe root resorption resulting from orthodontic treatment: prevalence and risk factors. Dental Press J Orthod. 2015;20(1):52-58.
42. Fink DF, Smith RJ. The duration of orthodontic treatment. Am J Orthod Dentofacial Orthop. 1992;102(1):45-51.
43. Stewart JA, Heo G, Glover KE, et al. Factors that relate to treatment duration for patients with palatally impacted maxillary canines. Am J Orthod Dentofacial Orthop. 2001;119(3):216-225.
44. Becker A, Chaushu S. Success rate and duration of orthodontic treatment for adult patients with palatally impacted maxillary canines. Am J Orthod Dentofacial Orthop. 2003;124(5):509-514.
45. Cohen ES. Atlas of Cosmetic and Reconstructive Periodontal Surgery. 3rd ed. Boston, MA: BC Decker; 2007.
46. Ngan P, Hornbrook R, Weaver B. Early timely management of ectopically erupting maxillary canines. Semin Orthod. 2005;11(3):152-163.
47. Clark D. The management of impacted canines: free physiologic eruption. J Am Dent Assoc. 1971;82(4):836-840.
48. Cooke J, Wang HL. Canine impactions: incidence and management. Int J Periodontics Restorative Dent. 2006;26(5):483-491.
49. Smukler H, Castellucci G, Goldman HM. Surgical management of palatally impacted cuspids. Compendium. 1987;8(1):10-17.
50. Incerti-Parenti S, Checchi V, Ippolito DR, et al. Periodontal status after surgical-orthodontic treatment of labially impacted canines with different surgical techniques: a systematic review. Am J Orthod Dentofacial Orthop. 2016;149(4):463-472.
51. Woloshyn H, Artun J, Kennedy DB, Joondeph DR. Pulpal and periodontal reactions to orthodontic alignment of palatally impacted canines. Angle Orthod. 1994;64(4):257-264.
52. Bariani RC, Milani R, Guimaraes Junior CH, et al. Orthodontic traction of impacted upper canines using the VISTA technique. J Clin Orthod. 2017;51(2):76-85.
53. Chapokas AR, Almas K, Schincaglia GP. The impacted maxillary canine: a proposed classification for surgical exposure. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113(2):222-228.
54. Vermette ME, Kokich VG, Kennedy DB. Uncovering labially impacted teeth: apically positioned flap and closed-eruption techniques. Angle Orthod. 1995;65(1):23-32.
55. Remington DN, Joondeph DR, Artun J, et al. Long-term evaluation of root resorption occurring during orthodontic treatment. Am J Orthod Dentofacial Orthop. 1989;96(1):43-46.
56. Ericson S, Bjerklin K, Falahat B. Does the canine dental follicle cause resorption of permanent incisor roots? A computed tomographic study of erupting maxillary canines. Angle Orthod. 2002;72(2):95-104.
57. Dağsuyu İM, Okşayan R, Kahraman F, et al. The relationship between dental follicle width and maxillary impacted canines' descriptive and resorptive features using cone-beam computed tomography. Biomed Res Int. 2017;2017:2938691.
58. Yan B, Sun Z, Fields H, Wang L. Maxillary canine impaction increases root resorption risk of adjacent teeth: a problem of physical proximity. Am J Orthod Dentofacial Orthop. 2012;142(6):750-757.