You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
High rates of opioid prescribing are a significant public health concern that have been linked to the growing opioid abuse epidemic in the United States.1-4 Regions with a higher number of dentists per capita are associated with increased opioid prescribing rates, as oral healthcare practitioners (OHCPs) are more likely to prescribe opioids than primary care physicians.5,6 In 2014 it was reported that dentists were responsible for 6.4% of all outpatient immediate-release opioid prescriptions in the United States,6,7 and while we have seen a general decrease in opioid prescription rates in dentistry since then, by 2019, 23% of all opioid prescriptions for children were still dental related.8,9 This is concerning as it has been more than 10 years since the publication of an article in the Journal of the American Dental Association identifying that "the appropriate use of opioids requires dentists to follow responsible and tailored prescribing practices to provide adequate pain control while limiting opportunities for abuse and diversion."10 Additional published reports have provided statistics highlighting these concerns, but very few have offered specific guidance to assist front-line OHCPs in choosing better analgesic alternatives for their patients.11-17
According to the Centers for Disease Control and Prevention (CDC), fatal opioid-related overdoses spiked in 2021, soaring from 56,064 the previous year to 75,673.18 For the first time ever, the total number of opioid-related deaths in the United States exceeded 100,000 in a continuous 12-month period ending in April 2021.18 The CDC found these 100,306 drug overdose deaths to represent an increase of 28.5% compared with the 78,056 deaths during the same period of previous year.18 Even more recently, a report published in The Lancet, by the Stanford-Lancet Commission on the North American Opioid Crisis, concluded that without urgent intervention, the United States will incur more than 1.2 million fatal opioid-related overdoses during the next 10 years.19
While an OHCP's instinctive reaction to the current state of the opioid abuse epidemic may be to discontinue prescribing opioids or replace the prescribing of opioids with another agent or treatment, this stance overlooks the legitimate necessity of these medications for certain patients. However, with the goal of reserving opioid-containing medications for only those cases where they are truly indicated, non-narcotic analgesic strategies should be utilized whenever possible. This article discusses examples of therapeutic strategies using synergistic drug combinations that can help limit the use of opioid-containing combination products, while also offering effective analgesia to dental patients.
Synergism
Synergism, or synergy, is most often defined in pharmacology as the effect of two or more agents working in combination that is greater than the expected additive effect of either drug alone.20Synergism allows the therapeutic effects of two or more medicines to be maximized while minimizing potential adverse effects.21,22 Historically, if a patient requires a larger effect of a medication, the prescriber would tend to give a higher dose of the drug. This is referred to as an additive effect and has also been referred to as noninteraction, and inertism:1 + 1 = 2.21The challenge in simply administering more and more of a medication, however, is that higher doses may increase the likelihood of adverse effects.
If two drugs act synergistically, especially if each drug works by a different mechanism of action, lower doses of each drug can be used and thus minimize the potential for adverse effects while still providing the desired outcome. This is referred to as a synergistic or potentiated effect (1 + 1 > 2), also called superadditivity or augmentation. The term coalism is also sometimes used to refer to synergy when neither drug, or none of the drugs in mixtures of more than two chemicals, is effective on its own.21
There are a number of examples of synergistic drug combinations with over-the-counter (OTC) medications as well as with prescription therapeutics. Common OTC examples include medications that contain aspirin, acetaminophen, and caffeine (Excedrin®, GlaxoSmithKline), or ibuprofen and diphenhydramine (Advil® PM, Wyeth Pharmaceuticals), acetaminophen and diphenhydramine (Tylenol® PM, Johnson & Johnson), and ibuprofen and pseudoephedrine (Advil® Cold & Sinus, Wyeth Pharmaceuticals), among others. In dentistry, an early example of synergy is the topical local anesthetic EMLA® (eutectic mixture of local anesthetics, APP Pharmaceuticals) approved by the US Food and Drug Administration (FDA) in 1992. This medication is a combination product containing 2.5% lidocaine and 2.5% prilocaine.23 When compared with the topical application of 20% benzocaine gel, EMLA been found to be both safer and more efficacious.23 Other combination products used in dentistry include postoperative analgesics as shown in Table 1; however, these are examples of pharmacologic synergism therapies that could contribute to the opioid abuse epidemic due to the narcotic moiety.24Another example of a synergistic drug combination in dentistry is the combination of the local anesthetic lidocaine with the vasoconstrictor epinephrine. Interestingly, lidocaine is clinically effective as a dental local anesthetic only when it is administered with epinephrine because the duration of anesthesia is influenced by the length of time that the local anesthetic remains in close proximity to neural fibers. Without epinephrine, the duration of local anesthesia is less than 10 minutes, which explains why lidocaine alone is no longer available in dental cartridges, having been removed from the market in 2011.25
Celecoxib and Tramadol
The American Association of Endodontists first developed a flexible analgesic strategy for the management of acute orofacial pain in 1995, which has been updated by different investigators in recent years (see "Acetaminophen Plus Ibuprofen" section, below).26-29 Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen have been shown to be more effective in reducing acute dental pain than opioid analgesics and are recommended as the preferred therapy for pain management.26 This should make intuitive sense, because orofacial pain is typically due to inflammation, and opioid analgesics are not anti-inflammatory agents like NSAIDs. In fact, regarding the use of opioids in the treatment of dental pain, the American Dental Association House of Delegates adopted the following statement: "Dentists should consider nonsteroidal anti-inflammatory analgesics as the first-line therapy for acute pain management."26 For situations in which NSAIDs alone are not effective, the combination of an NSAID with acetaminophen is recommended.30
Although medications such as acetaminophen and ibuprofen can also be given preoperatively to mitigate postoperative pain and meet analgesic medication requirements, a cyclooxygenase-2 (COX-2) selective NSAID, such as celecoxib, is ideally suited for this strategy. When compared with traditional nonselective NSAIDs, celecoxib can preemptively ameliorate the inflammatory response without causing increased bleeding or delayed wound healing postoperatively.31-33 A 400 mg dose of celecoxib administered orally 30 minutes prior to the dental procedure can maximize this potential benefit. For those patients who are currently taking an anticoagulant (eg, apixaban, betrixaban, edoxaban, dabigatran, rivaroxaban, or warfarin), a COX-2 inhibitor such as celecoxib could further be used to replace the postoperative ibuprofen prescription (ie, celecoxib 200 mg given every 12 hours for the initial 24-hour postoperative period).34
Tramadol is a synthetic analog of codeine and a centrally acting analgesic agent that has a relatively low affinity for opiate receptors.35Studies have been reported comparing tramadol with many analgesics for the treatment of pain associated with dental surgery, with tramadol repeatedly found to be more effective than codeine.36,37In a review of the literature, Moore concluded that tramadol may have limited utility for the management of acute pain in dentistry; however, this medication may have some therapeutic advantage if combined with a peripherally acting analgesic such as acetaminophen or an NSAID.38 Possible indications for use in dentistry may include cases where aspirin with codeine combinations are poorly tolerated or contraindicated, or where the potential for gastrointestinal adverse events contraindicate NSAIDs.39,40
In October 2021, the FDA approved a combination product of celecoxib and tramadol hydrochloride (Seglentis®, Esteve Pharmaceuticals) for acute pain management in individuals with pain severe enough to require an opioid analgesic and for which alternative treatments are inadequate.41Each tablet contains celecoxib 56 mg and tramadol hydrochloride 44 mg (equivalent to tramadol 39 mg), and the recommended dose is two tablets every 12 hours as needed for pain.41 Because of the risks of addiction, abuse, and misuse with opioids, even at recommended doses, Seglentis should be reserved for use in patients for whom alternative treatment options (eg, nonopioid analgesics alone) have not been tolerated or are not expected to be tolerated, or have not provided adequate analgesia or are not expected to provide adequate analgesia.41
Orphenadrine, Aspirin, and Caffeine
A combination of orphenadrine, aspirin, and caffeine, Orphangesic® Forte (Galt Pharmaceuticals) is a recently approved nonopioid pain medication for the treatment of mild to moderate pain.42 While orphenadrine alone is typically administered as 100-mg tablets every 12 hours for pain in otherwise healthy adults, this new combination product has been shown to be effective with just 50 mg of orphenadrine citrate, owing to the synergistic effect that occurs when the medication is combined with 770 mg of aspirin and 60 mg of caffeine.43
The exact mechanism of action of orphenadrine has not been clearly elucidated, but the drug appears to reduce skeletal muscle spasm, possibly through actions on cerebral motor centers or on the medulla. Orphenadrine does not have a direct skeletal muscle relaxant effect, but it does have analgesic activity, which may contribute to its skeletal muscle relaxant properties. Orphenadrine also possesses postganglionic anticholinergic effects and some antihistaminic and local anesthetic action. The antihistaminic activity is less than that of diphenhydramine, and in contrast to the sedative effect of diphenhydramine, orphenadrine produces a mild central nervous system stimulation.
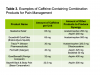
Caffeine is often combined with analgesic agents to provide a synergistic effect and a greater level of comfort than is achieved with higher doses of either drug alone (Table 2). In the dental model, Samieirad et al showed that when combining acetaminophen with caffeine versus codeine, the caffeine-containing analgesic resulted in significantly less swelling during the first 3 days postoperatively; the authors concluded that the use of caffeine-containing analgesics without the use of a narcotic is an acceptable and effective treatment for postoperative pain.44
While the clinical responses to caffeine are well known, the cellular mechanism of action is uncertain.45 At high concentrations, caffeine interferes with the uptake and storage of calcium by the sarcoplasmic reticulum of striated muscle (which would explain the effects of caffeine on skeletal muscle), but this does not appear to occur at clinically achievable concentrations. Currently, it is believed that xanthines such as caffeine act as adenosine-receptor antagonists. Adenosine acts as an autocoid, and virtually every cell in the human body contains adenosine receptors within the plasma membrane. Adenosine inhibits the release of neurotransmitters from presynaptic sites and works in concert with norepinephrine or angiotensin to augment their actions. Antagonism of adenosine receptors by caffeine would appear to promote neurotransmitter release, resulting in caffeine's analgesic properties.45
Acetaminophen and Ibuprofen
The mnemonic "2-4-24" is an easy way to help practitioners remember the near-ideal postoperative prescription involving acetaminophen and ibuprofen.46This memory aid stands for "2 drugs, in 4 doses, for 24 hours," referring to a combination of ibuprofen and acetaminophen to be administered every 6 hours for 24 hours. Depending on the doses selected, this strategy could address moderate to severe postoperative dental pain as described by the American Association of Endodontists' approach, as follows26,27:
For mild pain, administer 200 to 400 mg of ibuprofen as needed q4-6h.
For mild-to-moderate pain, administer 400 to 600 mg of ibuprofen fixed interval q6h for 24 hours, followed by 400 mg of ibuprofen as needed q4-6h.
For moderate-to-severe pain, administer 400 to 600 mg of ibuprofen plus 500 mg of acetaminophen fixed interval q6h for 24 hours, followed by 400 mg of ibuprofen plus 500 mg of acetaminophen as needed q6h.
For severe pain, administer 400 to 600 mg of ibuprofen plus 650 mg of acetaminophen with 10 mg of hydrocodone fixed interval q6h for 24 to 48 hours, followed by 400 to 600 mg of ibuprofen plus 500 mg of acetaminophen as needed q6h.
This combination is both effective and safe and should be recommended as first-line therapy in patients able to tolerate both medications.30 For the treatment of acute pain, the maximum recommended dose that should not be exceeded in otherwise healthy adults during a 24-hour period is 3,200 mg for ibuprofen47,48 and 4,000 mg for acetaminophen.26,48,49The combination of a nonsteroidal anti-inflammatory drug (NSAID), such as ibuprofen, and acetaminophen administered every 6 hours for at least 24 hours has been recognized and validated by both individual studies and meta-analyses as the postoperative prescription of choice for acute nociceptive orofacial pain.46,50-52
In some cases, if the over-the counter (OTC) forms of these two medications are prescribed, the overall pill burden to the patient may seem excessive: eight tablets of acetaminophen 325 mg and 12 tablets of ibuprofen 200 mg every 24 hours.26 One solution to this problem is the prescribing of a new OTC combination product, Advil® Dual Action (GlaxoSmithKline), the first and only nonprescription FDA-approved pain relief medication to combine acetaminophen and ibuprofen.53 Each tablet contains acetaminophen 250 mg and ibuprofen 125 mg, with the recommendation for adults to take two capsules every 8 hours while symptoms persist, and to not exceed more than six tablets in a 24-hour period, or acetaminophen 1,500 mg and ibuprofen 750 mg.53
While Advil Dual Action may seem like a perfect postoperative analgesia strategy for improving patient compliance, as it minimizes the potential pill burden to the patient, this combination product may have shortcomings. Most importantly, the daily doses of the active ingredients (acetaminophen 250 mg and ibuprofen 125 mg per dose) when compared to the target doses of the "2-4-24" strategy (acetaminophen 650 mg and ibuprofen 600 mg per dose) are impossible to achieve. Secondly, if patients attempt to match the optimal analgesic dose of ibuprofen 600 mg using Advil Dual Action tablets, they will greatly exceed the recommended maximum dose of acetaminophen, which is known to have serious health implications including potential liver toxicity and mortality.54
Conclusions
The opioid epidemic continues to plague our society. Recent reports conclude that without urgent intervention, the United States will incur more than 1.2 million fatal opioid-related overdoses during the next 10 years. Oral healthcare professionals continue to have higher rates of opioid prescribing than primary care physicians, and therefore dentists have been identified as having an important role in opioid abuse prevention efforts. While the knee-jerk reaction to our historical prescribing practices might easily be to simply discontinue prescribing opioids for postoperative dental analgesia, there will always be cases for which opioid-containing analgesics are clinically indicated and necessary, and clinicians should always attempt to match the right drug or drugs to the clinical situation. However, in almost all cases of acute dental pain, non-narcotic analgesic regimens that potentially leverage pharmacologic synergy, specifically combination therapy with acetaminophen and ibuprofen, should be prescribed as first-line therapy.
About the Authors
Mark Donaldson, BSP, ACPR, PharmD, FASHP, FACHE
Associate Principal
Vizient Pharmacy Advisory Solutions
Irving, Texas
Clinical Professor
School of Pharmacy
University of Montana
Missoula, Montana
Clinical Assistant Professor
School of Dentistry
Oregon Health & Sciences University
Portland, Oregon
Adjunct Professor
Faculty of Dentistry
University of British Columbia
Vancouver, British Columbia
Jason H. Goodchild, DMD
Vice President of Clinical Affairs
Premier Dental Products Company
Plymouth Meeting, PA
Associate Clinical Professor
Department of Oral and Maxillofacial Surgery
Creighton University School of Dentistry
Omaha, Nebraska
Adjunct Assistant Professor
Division of Oral Diagnosis
Department of Diagnostic Sciences
Rutgers School of Dental Medicine
Newark, New Jersey
References
1. U.S. Department of Health and Human Services. What is the U.S. opioid epidemic? https://www.hhs.gov/opioids/about-the-epidemic/index.html. Accessed February 4, 2022.
2. Volkow ND. America's addiction to opioids: heroin and prescription drug abuse. National Institute on Drug Abuse website. https://www.drugabuse.gov/about-nida/legislativeactivities/testimony-to-congress/2016/americas-addiction-to-opioids-heroin-prescriptiondrug-abuse. Published May 14, 2014. Accessed February 4, 2022.
3. Kolodny A, Courtwright DT, Hwang CS, et al. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health. 2015;36:559-574.
4. U.S. Department of Health and Human Services. HHS acting secretary declares public health emergency to address national opioid crisis. October 26, 2017. Available at: https://www.hhs.gov/about/news/2017/10/26/hhs-actingsecretary-declares-public-health-emergency-address-national-opioid-crisis.html. Accessed February 4, 2022.
5. The Centers for Disease Control and Prevention. Drug overdose deaths in the U.S. top 100,000 annually. https://www.cdc.gov/nchs/pressroom/nchs_press_releases/ 2021/20211117.htm. Published November 17, 2021. Accessed February 4, 2022.
6. Ringwalt C, Gugelmann H, Garrettson M, et al. Differential prescribing of opioid analgesics according to physician specialty for Medicaid patients with chronic noncancer pain diagnoses. Pain Res Manag. 2014;19(4):179-185.
7. Levy B, Paulozzi L, Mack KA, Jones CM. Trends in opioid analgesic-prescribing rates by specialty, U.S., 2007-2012. Am J Prev Med. 2015;49(3):409-413.
8. Yan CH, Lee TA, Sharp LK, et al. Trends in opioid prescribing by general dentists and dental specialists in the U.S., 2012-2019 [published online ahead of print February 26, 2022]. Am J Prev Med. S0749-3797(22)00068-X. doi: 10.1016/j.amepre.2022.01.009.
9. Okunev I, Frantsve-Hawley J, Tranby E. Trends in national opioid prescribing for dental procedures among patients enrolled in Medicaid. J Am Dent Assoc. 2021;152(8):622-630.
10. Denisco RC, Kenna GA, O'Neil MG, et al. Prevention of prescription opioid abuse: the role of the dentist. J Am Dent Assoc. 2011;142(7):800-810.
11. Koppen L, Suda KJ, Rowan S, McGregor J, Evans CT. Dentists' prescribing of antibiotics and opioids to Medicare Part D beneficiaries: medications of high impact to public health. J Am Dent Assoc. 2018;149(8):721-730.
12. Moore PA, Dionne RA, Cooper SA, Hersh EV. Why do we prescribe Vicodin? J Am Dent Assoc. 2016;147(7):530-533.
13. Moore PA, Ziegler KM, Lipman RD, Aminoshariae A, Carrasco-Labra A, Mariotti A. Benefits and harms associated with analgesic medications used in the management of acute dental pain: an overview of systematic reviews. J Am Dent Assoc. 2018;149(4):256-268.
14. Lutfiyya MN, Gross AJ, Schvaneveldt N, Woo A, Lipsky MS. A scoping review exploring the opioid prescribing practices of US dental professionals. J Am Dent Assoc. 2018;149(12):1011-1023.
15. McCauley JL, Hyer JM, Ramakrishnan VR, et al. Dental opioid prescribing and multiple opioid prescriptions among dental patients: administrative data from the South Carolina prescription drug monitoring program. J Am Dent Assoc. 2016;147(7):537-544.
16. Gupta N, Vujicic M, Blatz A. Opioid prescribing practices from 2010 through 2015 among dentists in the United States: what do claims data tell us? J Am Dent Assoc. 2018;149(4):237-245.
17. Gupta N, Vujicic M, Blatz A. Multiple opioid prescriptions among privately insured dental patients in the United States: evidence from claims data. J Am Dent Assoc. 2018;149(7):619-627.
18. Guy GP Jr, Zhang K, Bohm MK, et al. Vital signs: changes in opioid prescribing in the United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 2017;66(26):697-704.
19. Humphreys K, Shover CL, Andrews CM, et al. Responding to the opioid crisis in North America and beyond: recommendations of the Stanford-Lancet Commission. Lancet. 2022; 399(10324):555-604.
20. Roell KR, Reif DM, Motsinger-Reif AA. An introduction to terminology and methodology of chemical synergy-perspectives from across disciplines. Front Pharmacol. 2017;8:158.
21. Greco WR, Bravo G, Parsons JC. The search for synergy: a critical review from a response surface perspective. Pharmacol Rev. 1995;47(2):331-385.
22. Foucquier J, Guedj M. Analysis of drug combinations: current methodological landscape. Pharmacol Res Perspect. 2015;3(3):e00149.
23. Al-Melh MA, Andersson L. Comparison of topical anesthetics (EMLA/Oraqix vs. benzocaine) on pain experienced during palatal needle injection. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.2007;103(5):e16-e20.
24. Donaldson M, Goodchild JH. Could the prescription you write put you in legal jeopardy? Gen Dent. 2018;66(1):9-12.
25. Becker DE, Reed KL. Local anesthetics: review of pharmacological considerations. Anesth Prog. 2012;59(2):90-101.
26. American Dental Association. Oral analgesics for acute dental pain. https://www.ada.org/en/member-center/oral-health-topics/oral-analgesics-for-acute-dental-pain. Updated September 15, 2020. Accessed February 28, 2022.
27. Moore PA, Hersh EV. Combining ibuprofen and acetaminophen for acute pain management after third-molar extractions: translating clinical research to dental practice. J Am Dent Assoc. 2013;144(8):898-908.
28. American Association of Endodontists. Management of acute pain. Endodontics: Colleagues for Excellence. Newsletter. Spring/Summer 1995:1-4.
29. Moore PA, Hersh EV. Combining ibuprofen and acetaminophen for acute pain management after third-molar extractions: translating clinical research to dental practice. J Am Dent Assoc. 2013; 144(8):898-908.
30. Aminoshariae A, Kulild JC, Donaldson M, Hersh EV. Evidence-based recommendations for analgesic efficacy to treat pain of endodontic origin: a systematic review of randomized controlled trials. J Am Dent Assoc. 2016;147(10):826-839.
31. Munteanu AM, Cionac Florescu S, Anastase DM, Stoica CI. Is there any analgesic benefit from preoperative vs. postoperative administration of etoricoxib in total knee arthroplasty under spinal anaesthesia?: A randomised double-blind placebo-controlled trial. Eur J Anaesthesiol. 2016; 33(11):840-845.
32. Al-Sukhun J, Al-Sukhun S, Penttilä H, Ashammakhi N, Al-Sukhun R. Preemptive analgesic effect of low doses of celecoxib is superior to low doses of traditional nonsteroidal anti-inflammatory drugs. J Craniofac Surg. 2012;23(2):526-529.
33. Boonriong T, Tangtrakulwanich B, Glabglay P, Nimmaanrat S. Comparing etoricoxib and celecoxib for preemptive analgesia for acute postoperative pain in patients undergoing arthroscopic anterior cruciate ligament reconstruction: a randomized controlled trial. BMC Musculoskelet Disord.2010; 11:246.
34. Isiordia-Espinoza MA, Franco-González MA, Alonso-Castro ÁJ, Franco-de la Torre L. Analgesic effectiveness and safety of celecoxib versus non-opioid active controls after third molar surgery: a meta-analytical evaluation [published online ahead of print June 27, 2021]. J Stomatol Oral Maxillofac Surg. S2468-7855(21)00141-5. doi: 10.1016/j.jormas.2021.06.015.
35. Physicians' Desk Reference. 50th ed. Medical Economics Company; 1996.
36. Moore PA, Crout RJ, Jackson DL, Schnieder LG, Graves RW, Bakos L. Tramadol hydrocholoride: analgesic efficacy compared with codeine, aspirin with codeine, and placebo after dental extraction. J Clin Pharmacol. 1998;38(6):554-560.
37. Mehlisch DR, Minn F, Brown P. Tramadol hydrochloride: efficacy compared to codeine sulfate, acetaminophen with dextropropoxyphene, and placebo in dental extraction pain [Abstract PIII-34]. Clin Pharmacol Ther. 1990;47(2):187.
38. Moore PA. Pain management in dental practice: tramadol vs. codeine combinations. J Am Dent Assoc. 1999;130(7):1075-1079.
39. Donaldson M, Goodchild JH. Tramadol: what have we learned in the last 25 years? Gen Dent. 2021;69(4):14-18.
40. Sadeghein A, Shahidi N, Dehpour AR. A comparison of ketorolac tromethamine and acetaminophen codeine in the management of acute apical periodontitis. J Endod. 1999;25(4):257-259.
41. Seglentis [prescribing information]. Esteve Pharmaceuticals; October 2021. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/213426s000lbl.pdf. Accessed March 3, 2022.
42. Orphangesic Forte [prescribing information]. Atlanta, GA: Galt Pharmaceuticals; April 2021. Available at: https://orphengesicforte.com/assets/documents/Orphengesic-Forte-500523-2021-04-05-clean.pdf. Accessed March 23, 2022
43. Orphengesic Forte - an old analgesic combination returns. Med Lett Drugs Ther. 2020; 62(1611):180-181.
44. Samieirad S, Afrasiabi H, Tohidi E, et al. Evaluation of caffeine versus codeine for pain and swelling management after implant surgeries: a triple blind clinical trial. J Craniomaxillofac Surg. 2017;45(10):1614-1621.
45. Derry CJ, Derry S, Moore RA. Caffeine as an analgesic adjuvant for acute pain in adults. Cochrane Database Syst Rev. 2014;12:CD009281.
46. Donaldson M, Goodchild JH. Appropriate analgesic prescribing for the general dentist. Gen Dent. 2010;58(4):291-297.
47. Motrin Ibuprofen Tablets, USP [package insert]. New York, NY: Pfizer; 2007. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2007/017463s105lbl.pdf. Accessed March 30, 2022.
48. Queremel Milani DA, Davis DD. Pain management medications. Stat Pearls [internet]. Treasure Island, Fl: StatPearls Publishing; 2022. Available at: https://www.ncbi.nlm.nih.gov/books/NBK560692/. Updated August 19, 2021. Accessed April 4, 2022.
49. Acetaminophen Injection, for intravenous use [prescribing information]. Lake Zurich, IL: Fresenisu Kabi; 2015. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/204767s000lbl.pdf. Accessed April 4, 2022.
50. Aminoshariae A, Kulild JC, Donaldson M. Short-term use of nonsteroidal anti-inflammatory drugs and adverse effects: an updated systematic review. J Am Dent Assoc. 2016;147(2):98-110.
51. Christensen GJ. Pain meds: what works? Clinicians Report. 2015 ;8(2).
52. Becker DE. Pain management: part 1: managing acute and postoperative dental pain. Anesth Prog. 2010;57(2):67-79.
53. Searle S, Muse D, Paluch E, et al. Efficacy and safety of single and multiple doses of a fixed-dose combination of ibuprofen and acetaminophen in the treatment of postsurgical dental pain: results from 2 phase 3, randomized, parallel-group, double-blind, placebo-controlled studies. Clin J Pain.2020;36(7):495-504.
54. Donaldson M, Goodchild JH. Acetaminophen: how safe is it? Gen Dent. 2022;70(2):9-13.