You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
INTRODUCTION
Pain control is the cornerstone of modern dental practice, with patients demanding better and more painless dental procedures through various anesthesia techniques. Local anesthesia was introduced to the dental profession in 1884 and today's options for anesthetizing specific sites in the mouth have become more varied, with dental professionals having many more options to ensure the comfort and safety of their patients during any dental procedure. Most of today's local anesthetics employ a cartridge, needle, and syringe. The syringe is reusable, while the cartridge and needle are single use and disposable. Because an estimated 300 million anesthetic cartridges are used each year, it is critical to have a broad knowledge of the wide variety of products available, correct techniques for using them, and how to manage reactions or emergency situations, should they arise.
Allied dental staff plays an important role in assuring the comfort and safety of dental patients before, during, and after administration of local anesthesia to patients within a dental practice. This course is intended to provide dental professionals with basic knowledge on local anesthesia used in practice today.
HISTORY OF PAIN CONTROL
The history of pain control can be traced back to early times in Sumaria with the use of opium ca. 4000 BCE. Through the centuries, progress was made and we are where we are today with a variety of anesthesia techniques available to the dental patient. Science, medicine, and dentistry were weaved throughout history, and experimentation was built on preceding techniques. Understanding the history of pain can help practitioners and researchers grasp the nature of pain, and demonstrate how the pain management specialty grew to include the current range of treatment options.
There was the mechanical school of thought made up of individuals who wanted to return to the belief that the human body functions as a simple machine. This school of thought was popular up until the middle of the 18th century. Toward the end of the 18th century, there was the vitalist school of thinking, which was the more dominant line of thought. Those thought leaders adopted the concept of sensitivity, which included the simultaneous concepts of physiology and psychology. The minority school of thought (animism) felt that nature was more passive. Those believers accepted mechanical explanations and considered the soul to be directly responsible for all organic functions. Further, they believed it made pain an important sign in illness as a result of internal strife.
Various plants, herbs, and drugs were used in different combinations throughout time. Efforts to minimize pain were not confined to the inhalation drugs in the early days of anesthesia. Application of continual pressure on blood vessels, local applications of ice water, ethyl chloride spray, and sometimes a crack on the head with a mallet were among the methods used to reduce pain during a procedure. Prior to the introduction of ether by Morton in 1842 and nitrous oxide by Wells in 1844, little could be done to reduce the discomfort associated with the performance of dental and other oral procedures. These chemicals were used mostly for analgesia or anesthesia during extractions and other surgical procedures, and most patients did not experience anesthesia for other types of routine dental procedures until after the introduction of conduction anesthesia in the late 1800s.1 The timeline in Appendix 1 shows creativity as well as experimentation until these techniques were perfected with elapsed time.
HISTORY OF LOCAL ANESTHESIA
Local anesthetics have been used for dental procedures for over 100 years. Although dentists first introduced anesthesia to the world, it was a physician who used the first local anesthetic for a dental procedure. Local anesthesia has been making life more comfortable for dental patients since 1884, when Carl Koller discovered the analgesic properties of cocaine. That same year, William S. Halsted introduced conduction anesthesia by using cocaine to block the inferior alveolar nerve. Although cocaine was effective for achieving profound anesthesia, it was found to be highly addictive. Today, dental schools across the country teach a variation of Dr. Halsted's mandibular nerve block.
The most successful local anesthetic used in dentistry, procaine, was introduced in 1904 by Alfred Einhorn. The drug's brand name, Novocaine® or Novocain®, was once recognized by everyone. Procaine (Novocaine®) was widely used by physicians and dentists into the 1950s, and Novocaine® is still the name that many patients usually relate with local anesthetics. When mixed with a very small proportion of epinephrine, procaine was found to be highly successful and safe as a local anesthetic choice for most patients. By the 1950s, lidocaine (Xylocaine®) became widely accepted. Although many other local anesthetic agents are currently in use and nitrous oxide is often used for its analgesic effect, lidocaine is still one of the principal anesthetics in use today.
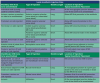
Today's dental professionals have many options of local anesthetics from which to choose (see Table 1). During World War I, Dr. Harvey Cook, who had observed brass munitions cartridges, created the first anesthetic cartridge for dentistry using brass cartridges and pencil erasers as stoppers. About 40 years after the introduction of procaine, Dr. Niels Jorgensen developed a procedure now known as intravenous conscious sedation. Dr. Jorgensen used intravenous injection, which he called "intravenous premedication," to administer a combination of pentobarbital, meperidine, and scopolamine. Since 1955, his technique has been accepted as an adjunct to local anesthesia, taught as early as 1945 in the Loma Linda Dental School in California. In 1948, a new local anesthetic, lidocaine, was introduced by Nils Lofgren of Astra Pharmaceuticals. This has become the "gold standard" for local anesthetics in dentistry.2
Beginning in 1972, the American Dental Association's (ADA) Council on Dental Education published "Guidelines for Teaching the Comprehensive Control of Pain and Anxiety in Dentistry." These guidelines were first published in the Journal of Dental Education and are continually updated as needed by the ADA House of Delegates.3
PURPOSE AND TYPES OF LOCAL ANESTHESIA
Reduced pain and anxiety is the purpose of using local anesthesia during dental procedures. Local anesthesia is produced by the application or injection of a pharmacologic agent to eliminate pain or sensation in a specific area in the mouth for a short period of time. These agents are commonly used for most dental procedures to ensure patient comfort and safety, based on the professional judgment of the dentist.
Properties of an ideal local anesthetic include the following:
• Potent local anesthesia
• Reversible local anesthesia
• Absence of local reactions
• Absence of systemic reactions
• Absence of allergic reactions
• Rapid onset
• Satisfactory duration
• Adequate tissue penetration
• Low cost
• Stability in solution (long shelf-life)
• Sterilization by autoclave
• Ease of metabolism and excretion
Cocaine, which comes from the coca bush, is the only naturally occurring anesthetic agent, but has not been used in dentistry since the early 1900s. All local anesthetics currently in use are synthetic.4 Local anesthetics normally contain the active ingredient and a vasoconstrictor, such as epinephrine. There are other vasoconstrictors available such as Levonordefrin® when reduced dosages of epinephrine are recommended for use on a patient for medical reasons.
Commonly Used Local Anesthetics
For anesthetic cartridges, colored bands can provide an added check on the type of anesthetic being used. The following color code format for banding of cartridges is used for various local anesthetics with varying amounts of epinephrine. Many dental professionals may use more than one type of anesthetic when working on different areas of the mouth. It is important for the dental professional to be aware of the color bands on anesthetics as a check on the product that is being requested in the syringe.
• The color code shall consist of a band 3.0±0.5 mm wide at a distance of 15±5 mm from the stopper end of the cartridge.
• The end cap of the cartridge may be either color-coded to match the ADA Color-Coding System or given a neutral color. (Figure 1, Figure 1A, Table 2)
• The stopper will not be color-coded and should not be indicative of the drug or color code.
• Lettering on the cartridge shall be black and font size should follow FDA labeling guidelines (headings at least 8 point type and text at least 6 point type).
• Lettering shall be in durable print that will not be removed by normal office handling.
ANESTHETIC CARTRIDGES, SYRINGES,AND NEEDLES
In order to deliver local anesthesia, it is necessary to use anesthetic cartridges, syringes, and needles. There are several styles of syringes available, as well as a number of needles in various gauges.
Anesthetic Cartridges
Local anesthetic solutions are supplied in glass cylinders called cartridges or carpules. One end of the cartridge has a rubber or silicone stopper (which is slightly indented from the edge of the glass) and the other end has an aluminum cap with a rubber diaphragm in the center. (Figure 9) The cartridge itself is covered with a plastic label that contains pertinent information: the name of the anesthetic solution and its concentration, the ratio of vasoconstrictor (if it contains one), the volume (1.7 ml), the lot number, the expiration date, and the manufacturer. The label on the cartridge should always be checked before it is used. It is imperative to note that the correct solution is being used, and whether or not it contains a vasoconstrictor. Also, the cartridge should not be used past the expiration date.
In addition to checking the label of the cartridge, the dental assistant should check to be sure that the cartridge is not broken or chipped, that the rubber stopper is not extruded (extending beyond the edge of the glass), and that there are no bubbles in the solution (these signs could mean the solution may have been frozen), that the metal cap is not rusted or corroded, and that the solution is not discolored or cloudy. If any of these conditions exist, the cartridge should be discarded. Anesthetic cartridges are stored at room temperature, in a dark place, and in their original containers. Some dentists prefer that the diaphragm be disinfected with an alcohol wipe just prior to use. Once a cartridge has been placed into a syringe, it must either be used or discarded; never save it for reuse.6
Syringes
Anesthetic syringes vary in design and can be either stainless steel, which are autoclavable; or plastic, which are autoclavable or disposable. The most common type of syringe used in dentistry is the aspirating syringe. The parts of the syringe are shown in Figure 7, and their functions are discussed in Table 3. The aspirating syringe is recommended by the ADA.7 It protects the patient by allowing the clinician to check for proper placement of the needle before actually injecting the anesthetic solution. Anesthetic solutions must not be injected into the bloodstream because they can be toxic. The aspirating syringe prevents the injection of the solution into a blood vessel. The clinician will place the needle in the tissue and then apply negative (back) pressure on the thumb ring. If the needle is placed in a blood vessel, blood will be aspirated (or drawn back into) the cartridge. The clinician then knows that they must withdraw the needle and reposition it so that the solution will not be injected into a blood vessel.
Needles
Needles used for dental injections are disposable and are never reused. They are supplied in a sterile plastic cover. The plastic cover consists of two sections, which are safety sealed. Under one of the plastic covers (usually the clear portion) is the syringe end of the needle. This is the shorter end of the needle and it will penetrate the diaphragm of the anesthetic cartridge. This is also where it will be screwed onto the syringe; this part of the needle is called the hub. (Figure 8) Under the other plastic cover is the shank of the needle. At the penetrating end of the needle is the bevel. The bevel is the slanted tip of the needle. The needle is hollow in the center, and this center portion through which the anesthetic solution flows is called the lumen. There are two lengths of anesthetic needles available: short (1") and long (15/8"). The length depends on the area to be anesthetized, and on the clinician's preference. Generally, the short needle is used for infiltration and field block injections. The long needle is commonly used for nerve block injections. (Figure 10)
Anesthetic needles are also available in varying diameters, or gauges. This refers to the thickness of the needle. There are three gauges commonly used in dentistry: 25, 27, and 30. The larger the gauge number, the smaller the diameter of the needle (the thinner the needle). For example, a 30 gauge needle is thinner than a 25 gauge needle. For infiltration and field block anesthesia, a smaller gauge needle (30) is often used, while a higher gauge needle (27, or 25) is used for nerve block anesthesia. Generally, when using a longer needle, a higher gauge is used because it allows the needle to be stronger. Figure 3 illustrates a disposable needle.
Assembly of the Syringe
In order to properly assemble the syringe with the anesthetic cartridge and the needle, the assistant must be certain that they have assembled the correct items. Selection of the proper anesthetic solution is critical. The assistant should check the patient's record to determine the type of anesthesia to be used. The assistant must also know what area of the oral cavity will be anesthetized in order to determine the proper needle length and gauge. The dental provider should be consulted regarding both the type of anesthesia and the type of needle before the syringe is assembled.8 When the appropriate anesthetic cartridge has been chosen, it should be inspected, as described in the previous section on anesthetic cartridges. The assistant should also double-check that they have chosen the correct type of anesthesia. The syringe can then be removed from its protective wrapping, and inspected to be sure it is safe and ready for use.
The following steps are then taken to complete the assembly of the syringe.
1. Hold the syringe in one hand, pulling back on the thumb ring to retract the piston.
2. Place the rubber stopper end of the cartridge in the barrel of the syringe first, with the stopper facing the thumb ring and the metal cap facing the needle end of the syringe.
3. Gently release the thumb ring, and with moderate pressure push the piston rod into the rubber stopper to engage the harpoon. Do not place a hand over the cartridge while engaging the harpoon. Gently pull back on the thumb ring to check that harpoon is engaged.
4. Break the safety seal on the needle cover and remove the clear plastic cover from the syringe end of the needle. If a needle is found to have a previously broken seal, it should be discarded in the sharps container, and a new one obtained. Do not remove the needle guard (the other plastic cover) from the injection end of the needle.
5. Screw the needle onto the syringe, being certain that it is on straight and firmly.
6. Loosen, but do not remove, the needle guard from the needle. Place the syringe on the tray out of the sight of the patient.
The syringe may also be assembled by placing the needle on the syringe first and then placing the cartridge into the barrel of the syringe. To prevent accidental needle-sticks from a contaminated needle, it is best that once the needle has been contaminated (used for an injection), the syringe should not be transferred from assistant to dentist. The dentist should retrieve the syringe for additional injections. The needle should also be recapped using a one-handed scoop technique. This is accomplished by sliding the needle into the needle guard, using only one hand. Needle recapping devices may also be used. In the event that a second injection is necessary, the assistant should be sure the needle guard is in place, and place a new cartridge in the syringe. The syringe is then placed on the tray for the dentist to retrieve. Once the treatment is complete, the needle should be carefully removed from the syringe with the needle guard in place, and then discarded in a sharps container. Before discarding the needle in the sharps container, check to be sure that the hub end of the syringe did not come off with the needle. The anesthetic cartridge is then removed from the syringe, and it too can be placed in the sharps container (check with local laws regarding disposal of anesthetic cartridges). The syringe must be cleaned and sterilized appropriately.
Topical Anesthetics
The goal for using topical anesthetics is to reduce discomfort associated with an injection. A topical anesthetic is applied to numb the surface of the gingiva in preparation for injecting a local anesthetic at that site (Figure 4A). Unlike injectable anesthesia, topical anesthetics anesthetize only the top portion of the mucous membrane or tissue and do not provide anesthesia for the teeth or bony structures. They are used to anesthetize the surface of an injection site. Most topical anesthetics require up to 1 minute to anesthetize the area, therefore, always check the manufacturer's directions for use. Whenever possible, use topical anesthetics to minimize the patient's discomfort associated with injections. For example, after the tissue is dried, a topical anesthetic can be applied to a sterile cotton swab and placed at the injection site prior to the actual injection. It is important to use a topical anesthetic for maxillary lingual injections, just medial to the first molar, because these can be among the most painful sites for injection.
The concentration of the topical anesthetics used for topical application is high to facilitate diffusion of the drug through the mucous membranes; about 2-3 mm. Care should be taken that only a small amount is applied to limited areas to avoid toxicity. Topical anesthetics are available in creams, ointments, aerosols, sprays, lotions, and jellies. A variety of topical anesthesia agents are available in either ester or amide formulations, and include benzocaine (an ester), butamben, dibucaine, lidocaine (an amide), oxybuprocaine, pramoxine, proparacaine, proxymetacaine, and tetracaine (an ester). The most common form of topical anesthetic in most dental offices is benzocaine gel in a 20% concentration. Some dental practices have a topical spray on hand for use with patients that have difficulty with dental radiographs. Topical sprays deliver a continuous stream when activated until the spray is deactivated, potentially delivering a very high dose of anesthetic agent. There are sprays that do deliver a measured dose and limit the amount that can be expelled, therefore making the use of these dose-limiting sprays safer to the patient.
In recent years, oral cavity patches have been developed that adhere to the gingiva and deliver targeted, consistent release of topical anesthesia. These have been found to provide more effective pain relief than topical applied with a swab, when using large needles that are inserted to the bone. (Figure 4A)
Injectable Anesthetics
Local anesthetics are classified into two general categories according to linkages: amide (NHCO) linkage and ester (COO) linkage. These specialized linkages join to a common carbon chain that is joined to a hydrophilic chain of amino (which confers the pKa of the anesthetic). Chemically, all injectable local anesthetics used in oral healthcare today have three chemical components: an aromatic lipophilic group, an intermediate chain, and a hydrophilic amino group.
The lipophilic group in anesthetics is made up of the aromatic ring structure which ensures that the anesthetic agent is strong enough to penetrate the lipid-rich nerve membrane where impulse conduction is blocked. When the hydrophilic portion of the local anesthetic is combined with the hydrochloric acid, the anesthetic is allowed to diffuse through the interstitial fluid in the tissues to reach the nerve. The intermediate chain is the linkage that determines whether the anesthetic agent is classified as an amide or as an ester. The nature of the intermediate linkage is important in defining several properties of the local anesthetic including possible allergic reactions and biotransformation. The mechanism by which local anesthetics are metabolized is important because the overall toxicity of an agent is dependent on the balance between the anesthetics' rate of absorption into the bloodstream at the injection site and the rate the anesthetic is removed from the process of tissue uptake and metabolism. This is an important difference between the two classifications of anesthetics. Amide local anesthetics undergo biotransformation in the liver by microsomal enzymes. The liver function of the patient influences the rate of the biotransformation of the amide anesthetics. Those with impaired liver function are unable to process the anesthetics normally, which can lead to excessive levels of anesthetic in the blood, potentially leading to a toxic overdose. The metabolic products of both amide and ester anesthetics are almost entirely excreted by the kidneys, with a very small amount excreted unchanged in the urine. An easy way to tell the difference between an ester and amide is to determine if the generic name has an "i" before the - caine. This will only work with generic names and will not work with a trade or commercial name. All amide local anesthetics contain an "i" in the name (before the - caine). For example, lidocaine, mepivacaine, prilocaine, and bupivacaine all contain an "i" before the - caine. Esters such as procaine, chloroprocaine, and tetracaine do not contain an "i" before the - caine. Most injectable anesthetics are amides.4 All local anesthetics that are available in cartridges have pKas that range from 7.7 for Mepivacaine to 8.1 for Bupivacaine, thus making them weak bases. Procaine is the prototype for esters, although it is no longer available in dental syringe cartridge form.5
Table 1 summarizes some commonly used local anesthetics. Absorption of the pharmacologic agent is dependent on a number of factors, including whether the pH level of the tissue has dropped due to localized infection. Other factors include drug solubility, vascularity of the tissue at the injection site, and the impact of the agent on circulation. As such, duration is highly variable and specific for each drug. (Refer to the current Physician's Desk Reference - or "PDR" - for duration and potential side effects of specific products.)
Non-injectable Anesthetics
Non-injectable local anesthetics are a more recent development in dental anesthesiology. The U.S. Food and Drug Administration (FDA) approved them for use in adults who need localized anesthesia in periodontal pockets during scaling or root planning. Oraqix® (a lidocaine and prilocaine periodontal gel) is packaged into single-use cartridges and applied directly into the pocket with a blunt-tip applicator and its specially designed dispenser (Figure 4); it is not for injection. With a 2-minute onset and 20-minute duration, it can be applied to one or more periodontal pockets simultaneously. It can be reapplied as needed up to the maximum dosage of five full cartridges at one appointment.9
ADMINISTRATION OF LOCAL ANESTHESIA
Dentists and dental therapists (where applicable) are licensed to administer anesthesia, and many states and the District of Columbia allow dental hygienists to administer local anesthesia under the supervision of a dentist (Figure 5). State educational requirements vary for accreditation or board certification in the administration of local anesthetics by dental hygienists. Since requirements change and are different from state to state, it is important to check with your state dental practice act for the most up-to-date information.
Preparing the Patient
An injection may be routine for the dental provider, but it is often an unpleasant experience for the patient. Psychological support and reassurance is essential and will increase the patient's confidence in the dental provider. No particular method is generally appropriate, as some patients will grow confidence if an up-front approach, fully informative with nothing hidden is used. Sometimes patient fears cannot be dispelled and the provider must accept avoidance behavior while the injection is being administered. Such behavior may include clenched fists, closing of eyes, holding breath or humming out loud are just a few that have been encountered throughout one's career. Once the injection is complete, these patients will often state that the process was not as bad as they thought it would be.
Whenever possible, treatment should be given with the patient reclined in a supine position, which entails little risk of vasovagal attacks - hypotension and syncope. The vagus nerve interfaces with parasympathetic control over the heart, lungs, and digestive tract. Some physical or emotional conditions make the position impractical or impossible to use. Examples of when this positioning being unsuitable would be pregnant women, patients who have orthopedic disabilities, those who simply cannot be trained or psychologically reassured so that they would accept treatment in the supine position.
Patients should be positioned as supine as possible, keeping in mind that patient comfort is essential. Tight fitting garments may partially obstruct the flow of blood in the head and neck region. Patients can be instructed to loosen the collar of their shirt or blouse, when applicable, to prevent any possible complications during treatment. The patient should also be offered safety glasses to cover their eyes if they are not wearing eye glasses.
Nowadays, modern disposable needles guarantee a sharp tip with each injection, thus minimizing the actual discomfort of the injection if the provider's on top of their technique. Distraction analgesia also can help. If the tissue is gently pressed at some distance from the planned penetration site, or if the patient's lip is gently tugged or pinched, the perception of puncture pain will further be diminished. For palatal injections, the end of the mirror handle can be compressed against the palate to distract from the puncture discomfort.
Clinical Requirements for Local Anesthesia
Something that many of us do not think about is the clinical requirements for local anesthesia. The following are the necessary requirements.
Sterility
In theory, the administration of local anesthesia should be made under as sterile conditions as possible, just like all other surgical procedures. The fact that it is nearly impossible to achieve sterility in the oral cavity does not relieve the provider of their fundamental responsibility. Care must be taken and everything that can be sterile must be sterile. Injections made into healthy oral tissues virtually never give rise to infection. If the tissue at the injection site or near it is infected, there is a greater risk of spread. Up to this point, the situation is one of necessary compromise, but no compromise is allowable in respect to instruments. The needle, anesthetic cartridge, and syringe must be absolutely sterile. Only 0.00004 ml of infected serum is all that is needed to pass on serum hepatitis. A new sterile disposable needle, a fresh anesthetic cartridge, and a sterile syringe are required for each and every patient.
It should not be necessary to emphasize this further, but the use of "non-aspiring" cartridge syringes is no safeguard from cross contamination. Patient's blood is aspirated in more than 30% of such anesthetic cartridges and therefore a new cartridge is needed for each patient. The use of cartridges is a better system than the multiple dose vials, but even with a cartridge system, extra care must be taken. The rubber diaphragm should be swabbed with a 70% alcohol, two minutes before use.
Aspiration and Injection
Before injection of local anesthesia, controlled aspiration must always be made. Injections should be given with as little pressure as possible. In general, fluid flow will virtually be free, while injections into the papilla and hard palate will require some pressure. The mucosa of the hard palate is tightly adapted to the periosteum. Injections should be slow with using no more force or volume of local anesthetic than is absolutely necessary.
Preparing the Syringe
Prior to injection, the rubber plunger of the carpule should be displaced by slight pressure on the piston, because the plunger sticks to the glass during storage. If this is not done, the patient may experience discomfort when the plunger jerks at the beginning of the injection with the anesthetic solution being injected too quickly. The air bubble in the carpule should be expelled as far as possible at the same time.
The rubber plungers are treated with silicone during manufacturing, so this has become less of an occurrence. However, if paraffin is being employed by the manufacturer, difficulty may be encountered. It is recommended that carpules be stored at room temperature. If the problem persists, the provider may want to consider using carpules with silicone treated plungers to facilitate a smooth and even deposition of anesthetic.
Gas Bubbles
When anesthetic carpules are used, the actual needle cannot be filled with the anesthetic solution because of the elasticity of the rubber plunger, but the volume is so small that there is no consequence with small bubbles 1 to 2 mm in diameter. It is nitrogen gas that was bubbled into the anesthetic solution during the manufacturing process to preclude oxygen, which destroys the vasoconstrictor, from being trapped in the carpule. These small bubbles are harmless and may be ignored. Larger air bubbles with a diameter greater than 2 mm in the system must be eliminated to avoid the potential hazard of air being injected into the vein. These larger bubbles are an indication that the anesthetic has been frozen. These larger bubbles may also be accompanied by a stopper that extends beyond the carpule and is extruded. Because the sterility of the anesthetic solution is no longer guaranteed, the carpule should not be used. (Table 7 - Local Anesthetic Injection Sites)
ROLE OF ALLIED STAFF
Although at the time of this publication no state currently allows dental assistants to administer local anesthetic injections, dental assistants and other allied team members nonetheless are an intricate part of safe delivery of local anesthesia. Allied staff assembles, prepares, and transfers syringes to other dental professionals and often disassemble syringes. Safe handling of used needles is a critical role for allied staff to avoid needlestick and other sharps injuries.
Accuracy of the Medical History
The patient's medical history must be complete and up-to-date. Patients should provide a complete medical history, including information on current and past health conditions -especially liver and kidney functions, as these organs are important in clearing local anesthesia from the body. The medical history should be reviewed at each appointment and the patient asked about any changes.
The medical history should list all medications the patient is taking and document whether the patient uses any recreational drugs. The dentist should know if the patient is taking any drug, prescribed or otherwise, that may affect the use of local anesthesia. Examples of such drugs are tricyclic antidepressants, such as amitriptyline (Elavil®); beta blockers, such as propanolol (Inderol®); recent surgeries or general anesthetics, such as halothane (Fluothane®);5 and illicit drugs, such as cocaine. Finally, be sure the medical history notes any past allergic reactions. Over the counter medications and herbal supplements should also be noted in the medical history as each may interact with the local anesthetic and could affect the outcome of the procedure. Many dental practices post a copy of their medical history forms on their websites so patients can download them and fill them out in advance of their appointment.
Even with an initial medical history completed and on file, always question returning patients at each visit to ensure that any changes are noted. It is helpful to prompt them with specific questions about any new medications or recently diagnosed allergies or medical conditions.
Informed Consent
Allied staff also plays a crucial role in obtaining informed consent from patients undergoing dental procedures, including the administration of local anesthesia. Consent must be obtained in writing before any anesthetic is administered. Patients who are minors (e.g., under 18 years of age) or patients who by state law have legal guardians or authorized medical authorities cannot legally give consent. This includes, but is not limited to patients who are not mentally competent to understand any risks associated with the procedures. This can also include patients with developmental delays or dementia. In these situations, consent must be given by a parent, other family member, or court-appointed guardian. Resolve consent issues at a preoperative appointment, whenever possible.
Although local anesthetics have been used safely in the dental office for many years, the potential for complications does exist. As mentioned earlier, they must be used with caution. All information regarding the use of local anesthetics must be written in the patient's record. The type of injection, the type of anesthesia and its concentration, and the amount used should be notated in the record, as well as the patient's reaction(s) to the anesthetic. It cannot be stressed enough that the patient's medical history must be consulted before any local anesthesia is delivered. The patient may have a health condition or may be taking medications that could contraindicate the use of certain anesthetics, or even possibly any anesthetics. Those more susceptible to adverse reactions to local anesthetics include children, the elderly, and persons in poor health.10 After the anesthesia has taken effect, the patient loses all sensation to pain in the area anesthetized. This is the desired effect for the treatment period, but the numbness does not subside as soon as the treatment period is over. This temporary numbness can last for several hours after the appointment until the anesthesia wears off. The patient should be cautioned about not biting themselves while the anesthesia is still in effect. Also, it may seem as though the tongue, cheek, and lip feel fat, when indeed they are not.
Patient Monitoring
Allied team members are involved in monitoring the patient throughout the dental procedure, from start to finish. During the actual injection the assisting staff member should be positioned to block the patient's arms and hands should the patient reach for the dentist's hand. In addition to ensuring that the patient is as comfortable as possible, chairside staff should continually observe the patient after anesthesia is delivered to ensure that the patient is not in distress or developing an allergic reaction. Signs of an allergic reaction can include a number of factors, including any unusual swelling, excessive redness, shortness of breath or trouble with breathing. These should be addressed immediately. Since dentists may leave the treatment room after the injection, allied team members have a critical role in patient monitoring after the injection. Patients should not be left alone after local anesthesia has been administered. Patients of all ages should be observed to be sure they are not biting on anesthetized tissues. After a procedure is completed, allied staff should remind patients and caregivers to avoid biting or chewing to avoid tissue damage. It is also helpful to explain that if tissue damage does occur, what steps should be taken to identify and alleviate the discomfort until the issue is resolved.
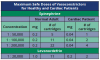
RECOGNIZING AND MANAGING CONTRAINDICATIONS, ALLERGIC REACTIONS, AND SIDE EFFECTS
About half of all emergencies in dental offices occur before or after administration of local anesthesia.9 Every dental team member should have and know the office protocol for managing emergencies, including who will call 911. Contraindications to local anesthetics are numerous. Before delivering local anesthesia, dentists should always consult the product insert packaged with local anesthetics or the PDR. Each product has a maximum amount based on the patient's weight. While most products are metabolized in the liver, plasma, or both, the half-life of the product is also important. This is the time that it takes to reduce potency by half. For 2% Lidocaine, this is about 90 minutes, and the half-life for 4% Articaine is 30 minutes. Except for prilocaine, which is metabolized in the kidney and plasma, the amide linkage anesthetics are metabolized in the liver.7 Therefore, impairment in liver function is a key contraindication to local anesthesia. The half-life of products should also be addressed with special consideration given to the duration of procedures and/or the age of the person, such as children under 12 years of age.
Common Complications
The treating provider generally informs patients about both simple, common complications, and serious, rare complications that can occur with the proposed procedures; and in doing so, they cover both extremes of the spectrum of complications. Although the use of local anesthetics to control pain is a safe, well-established procedure, adverse reactions can occur. These reactions include, but are not limited to, the following and are often found on the informed consent form:
• Allergic reactions to today's local anesthetics (lidocaine/septocaine/carbocaine) are extremely rare. Allergic reactions are characterized by cutaneous lesions, edema, redness, and other signs of allergies. Anaphylactic reactions involving trouble breathing, rarely happen, but will require a call to 911 if they do occur to ensure patient safety. If a patient has notated that they are allergic to local anesthetics, it may be necessary to do further testing to determine if they could tolerate a different anesthetic. As mentioned earlier, the amide class of anesthetics has a much lower allergic potential than does the ester class. Also, there may have been an additive to a particular anesthetic agent that the patient was allergic to, and not the agent itself.
Allergies to local anesthetics can be confirmed by intradermal testing by an allergy specialist. Most allergic reactions are limited to the outer tissues and can be treated with antihistamines; the more serious ones require treatment with epinephrine. The most common side effect of injections is syncope. Patients with a history of syncope should be considered for treatment with diphenhydramine.4 Allergic reactions to amide linkage anesthetics are relatively rare and mostly attributed to the preservatives or antioxidants found in the anesthetic. Ester linkage anesthetics have had a higher rate of reported allergy due to the para-aminobenzoic acid (PABA) preservative.
For documented allergy to both ester and amide groups, diphenhydramine can be used for procedures of short duration. A study that examined the impact of diphenhydramine administration in 17 patients found diphenhydramine efficacy similar to that found in seven patients using prilocaine. While larger studies are needed, diphenhydramine may be an effective alternative for patients with allergy to local anesthetics in emergency procedures.11
Most reported allergic reactions are caused by the preservatives methylparaben and metabisulfite.12 Metabisulfite is added as an antioxidant when vasoconstrictors are used in anesthetics. For patients reporting a documented allergy to sulfites, avoid anesthetics containing vasoconstrictors. For such patients with documented sulfite allergies, plain anesthetics such as mepivacaine 3% or Prilocaine 4% are available without the preservative.9
Latex allergies are commonly reported among patients. However, the latex stopper at the end of the cartridge is not made of "natural" latex commonly implicated in latex allergies. While the latex stoppers have not been implicated in available case reports of adverse reactions among dental patients, manufacturers of dental anesthetics must label any products that contain latex in cartridge anesthetics.13 As with many dental issues, no prospective epidemiologic study has evaluated this issue, but it cannot be ruled out in allergy situations. There are latex-free stoppers in certain brands of anesthetics available for patients with latex allergies. These are labeled as latex-free.
In addition to allergies, other contraindications are specific to certain anesthetics. Levonordefrin, an alternative to epinephrine, should not be used when a patient takes tricyclic antidepressants, and reduced dosages of epinephrine are recommended. For patients with significant cardiovascular disease, the dentist may choose to consult with their physicians. Recreational use of cocaine by patients can increase the risk of blood pressure and cardiac arrhythmias with injectable anesthetics.12-18 Data indicate that lidocaine and prilocaine may be safest for use among pregnant and lactating women.9 Paresthesia has been reported occasionally after local anesthesia with many of the amide linkages.12
• Fainting (vasopressor syncope) with or without a rapid pulse and lowered blood pressure. This is usually associated with fear and is a response mechanism.
• Hyperventilation syndrome is usually brought on by fear. It is characterized by tingling in the hands, lightheadedness, and tightness in the chest.
• Idiosyncratic reactions of unexplained origin are exaggerated responses to an average dose of a drug, in this case the local anesthetic. These reactions present clinically in a wide range of manifestations and the patient should inform the provider if they have a history of severe reactions to medical treatment.
• Rapid heartbeat (short term) can occur during the administration of local anesthesia due to the epinephrine that is included in most anesthetics. Everybody has epinephrine in their body naturally; it is often referred to as adrenaline. However, it can make your heart feel like it is racing for a few minutes when the medication is first introduced into your body. If the patient has high blood pressure, the patient should let the dental team know and an anesthetic can be used without epinephrine.
•Toxic reaction - The cardiovascular system and the central nervous system are the two main systems that are affected by local anesthesia toxicity. The degree of toxicity is directly related to the blood levels of the anesthetic agent, and the blood level is affected by10:
o Patient characteristics (such as weight and health);
o The type, amount, and concentration of anesthetic agent used;
o The rate of injection (a slower rate allows time for the area being injected to accept the volume of anesthetic agent);
o The rate of absorption;
o The presence of infection or inflammation increases chances of systemic toxicity.
Some of the signs of toxicity include restlessness, tremors, and convulsions, followed by central nervous system depression, respiratory and cardiovascular depression, and coma. Cardiac arrest may also occur. Although these adverse reactions would be rare with the amount of local anesthesia used in dentistry, it is still possible.10 Toxicity reactions occur from an overdose or rapid absorption of the anesthetic into the bloodstream via injection. Although providers will never use more anesthetic than recommended for patient body size, it is important to realize each patient has their own tolerance level. The patient should advise the provider if the patient is more, or less, tolerant of medications in general.
POTENTIAL COMPLICATIONS
There are also several potential complications that can arise from the injection itself that patients should be aware of:
• A quick feeling of "electrical shock" can occur as the anesthetic is administered near the nerve. This is often described as a feeling of an electrical shock. This sensation is normal and has no long term effects to the patient, but can be uncomfortable for a few seconds.
• Hematoma (swelling with bruising) can occur when a blood vessel is punctured during the injection. The released blood will pool under the influence of gravity and form a hematoma, thus leaving bruising that may be visible for up to 14 days.
• Jaw pain often occurs for two reasons. The first reason being the muscles around the jaw may be traumatized by the injection of anesthesia. Secondly, muscle fatigue results from the patient holding their mouth in an open position for an extended time period during the procedure.
• "Numbness" to additional areas of the patient‘s face can occur due to variations in nerve anatomy. For example, when we anesthetize the lower teeth, the nerve branches carry anesthetic to the lower lip and tongue as well the teeth. Sometimes the anesthetic may be carried along other nerve branches as well, in turn numbing other areas of the face unintentionally. Other common areas to receive anesthesia are the temples, eyelids, cheeks, and chin. Often, when the eyelids are anesthetized, the affected eye cannot close and will tear up. These areas will start to feel and react normally once the anesthesia wears off. Anesthesia typically lasts between 1 and 8 hours, but varies for each individual and on the anesthetic used.
• Paresthesia may occur if the nerve sheath is traumatized by the needle during the injection of anesthesia, bleeding into or around the nerve sheath, or injection with contaminated anesthetic solution (possibly from the alcohol or disinfecting solution used on the cartridge prior to use). This results in a residual tingling sensation, or in partial numbness of the affected tissue. Although paresthesia following a lower injection usually presents as a residual tingle in the lower lip and tongue, it can also affect the eyelids, cheeks, and chin. The symptoms of paresthesia gradually diminish, and recovery is usually complete. The numbness can last from a few hours or days, up to eight weeks. It is important that the patient inform the provider as soon as the patient experiences symptoms of paresthesia, so that the patient can undergo treatment immediately if needed. Early treatment is essential for success in certain cases of paresthesia. It usually reverses itself without treatment, but if the damage to the nerve was severe enough, it could be permanent.
• Reoccurrence of cold sores can occur in patients who already carry the virus for cold sores. In between outbreaks, the Herpes virus that causes cold sores lies dormant within the nerves. Therefore when the nerve is anesthetized, the virus may be awakened to form a new cold sore. Prescription medication can be taken prior to treatment to avoid a new outbreak.
•Trauma to lips and cheeks is a common complication of dental work. Largely because when patients are numb, they will not feel a bite injury as it occurs. It should be recommended that patients not eat while still numb. Patient's lips may become dry, chapped, and cracked as a result of the dental procedure.
•Injection into a blood vessel - As mentioned earlier, the presence of a local anesthetic in the bloodstream could be toxic. The oral cavity has a rich supply of blood vessels, and the dentist must be extremely careful to not inject the anesthetic into one of these blood vessels. The use of an aspirating syringe can prevent this from happening.
• Injection into an infected area - If a local anesthetic is injected into an infected area, it is possible for three things to happen. First, it will be difficult to achieve adequate anesthesia because anesthetic solution is not effective in the presence of an infection. Second, there is the chance that the infection will be spread. Lastly, the presence of an infection will increase the systemic absorption of the anesthetic, increasing the chance for a toxic reaction.
The benefits one can expect from local anesthesia include discomfort control during and after a dental procedure. When the patient is informed about what could happen, the patient is more at ease when and if it does happen.
ANATOMY
All providers delivering local anesthesia must have a detailed knowledge of the regional anatomy to avoid unnecessary injury to the patient and potential legal action. Even the most experienced practitioner can benefit from periodic review of the anatomy associated with local anesthesia and injection protocols to minimize the risk of complications.18 Local anesthesia by block can be delivered to two of the three branches of the trigeminal nerve, the maxillary nerve, and the mandibular nerve. Lingual anesthesia is achieved in the mandibular regions, except for anterior teeth with a block. For maxillary teeth, lingual anesthesia may be obtained with local injection.
The Maxillary Nerve
The maxillary nerve is exclusively sensory, passes through the foramen rotundum to reach the pterygopalatine fossa, where it has three divisions: the pterygopalatine nerve, the infraorbital nerve, and the zygomatic nerve.
The pterygopalatine nerve has several divisions, with two terminal branches that are most important in dental procedures. The anterior palatine nerve enters the oral cavity through the greater palatine foramen and is the larger of the two branches. It splits into a number of smaller branches at the greater palatine foramen and fans out as the greater palatine nerve, which supplies the mucosa of the hard palate to the canines. This nerve then goes into the palatine artery, which is inside connective tissue between the periosteum and the palatal mucosa. Injuries in the nerve endings in the palatal mucosa usually repair themselves, and patients will not normally experience any problems.
The posterior palatine nerve is the smaller of the two branches of the pterygopalatine nerve. This nerve, which provides sensory endings to the tonsils, goes through the lesser palatine foramen.
The infraorbital nerve encompasses three branches: the anterior, middle, and posterior superior alveolar nerves, which provide sensory endings to the maxillary teeth, the associated periodontal membranes, and gingiva on the lateral aspect of the maxilla. The nerve emerges at the infraorbital foramen. Injectable anesthetics act on the nerves in the superior dental plexus formed by the superior alveolar nerves in the base of the alveolar process. The patient will not experience any sensory deficits following procedures in this region.
Terminal branches of the infraorbital nerve fan out in the direction of the lower eyelid, nose, and upper lip from the infraorbital foramen. Several superior labial branches go into the lip between the muscles and mucous membrane to supply the mucosa of the upper lip and skin through the orbicularis muscle. When performing either apicoectomies on the maxillary canine or premolar teeth or carrying out sinus lift procedures on the atrophic maxilla, dentists must be especially careful to avoid injuring this nerve where it arises from the infraorbital foramen. Such an injury can cause a traumatic neuroma with permanent neurological loss. Conversely, injuries to the terminal branches that end in the lip will repair themselves.
The zygomatic nerve is a branch of the maxillary nerve that divides into a facial branch supplying the skin of the prominent part of the cheek and a temporal branch supplying the skin of the anterior temporal region.
The Mandibular Nerve
Both motor and sensory fibers make up this mixed nerve, which has four sensory branches. Its internal branch includes two nerves, the buccal and lingual nerves, which supply large areas of the oral mucosa. The middle branch - inferior alveolar nerve - supplies the mandibular teeth, skin, and mucosal membrane of the lower lip and skin of the chin. The auriculotemporal nerve in the external branch is never anesthetized in dentistry.
The buccal nerve, which is not involved in dental procedures, may need to be anesthetized because it sometimes causes pain perception during retraction. This nerve proceeds along the most forward (anterior) portion of the temporalis muscle downward along and within the fascia, along the outer portion of the buccinator muscle. Multiple branches of the buccal nerve travel through the buccinator muscle, providing innervation for most of the mucosa of the cheek.
Sensory and taste fibers are found in the lingual nerve, which separates from the inferior alveolar nerve approximately 5 to 10 mm below the base of the cranium. The lingual nerve is more forward (anterior) and slightly more to the middle (medial) in relationship to the inferior alveolar nerve. As shown in Figure 6, the lingual nerve follows along the outside (lateral) of the medial pterygoid muscle to the upper portion of the mylohyoid; at the mylohyoid muscle, the lingual nerve curves sharply anteriorly to continue on a flat plane across the inner surface of the floor of the mouth. This nerve is superficial in the posterior portion of the oral cavity. It sometimes can be seen with the naked eye through the thin membranes of the lingual mucosa, beginning at the third molars to the second molars. The nerve turns medially near the first molar and goes under the submandibular duct, with multiple branches that innervate the tongue.
Removal of impacted third molars presents the highest potential for injuring the lingual nerve, as it is most exposed medial to the retromolar trigome. This is most likely to occur in patients who have had repeated episodes of pericoronitis. While Figure 6 shows the usual pattern of this nerve, not all patients have this pattern. In about 10 percent of patients, the lingual nerve is located at a higher level in relation to the internal oblique ridge. An injury in this location is likely to cause varying degrees of permanent damage. Microsurgical repairs have an 80 percent success rate for return to pain-free sensory function if they are done within 90 days of the injury.
The inferior alveolar nerve divides in the premolar region into the incisive and mental nerves, which supply the teeth and periodontal ligaments of the mandibular teeth. The mental nerve further divides into three to five branches after exiting the mandible through the mental foramen. The incisive branch stays within the mandible, where it continues and becomes part of the inferior dental plexus.
The relative position of the lingual nerve varies depending on the age of the patient. As the mandible grows and moves more forward and more laterally, the lingual nerve becomes more posterior and superior to the ramus of the mandible. Beginning at the third molar area, the inferior alveolar nerve arches at the apex of the molars and continues below the roots of the first molars.
In the premolar region of the mouth, this nerve is about halfway between the roots and the lower mandible border. If dental surgery is planned in this area, the nerve should be located through the use of a panoramic image before the procedure begins. The inferior alveolar canal can be found about 4 to 7 mm from the mandible's lateral cortical cortex. Third molar surgery presents the greatest risk of injury to this nerve, but because the nerve is located inside the bony canal, nerve regeneration is more likely, along with the return of sensation, as long as fractured canal fragments do not block the canal. Microsurgical repair should not be considered until at least three months after the injury. Persistent neurosensory deficits are more likely in patients over age 40; in more than half of these patients, alveolar nerve injury may result in continuing problems, such as lip biting and drooling. For this reason, patients over age 40 should be given presurgical counseling on the possibility of such complications, and asymptomatic impacted third molars should not be removed.19
TYPES OF INJECTIONS
There are four main types of local anesthesia injections given in dentistry and a variety of adaptations for various procedural needs. This next section will briefly discuss each of the three types: infiltration, field block, and peripheral nerve block anesthesia.
Infiltration Anesthesia
Infiltration anesthesia involves the injection of the anesthetic solution into the tissues near tiny terminal nerve branches. This form of anesthesia is used anywhere in the oral cavity when procedures such as biopsies, gingivectomies, and other tissue surgeries are performed. It is used primarily for soft tissue anesthesia.
Field Block Anesthesia
Field block anesthesia is similar to infiltration anesthesia (the terms are sometimes used interchangeably), but the difference is that the anesthetic solution is deposited near larger terminal nerve branches for field block anesthesia. The injection is usually given at the apex of a tooth, and will involve one or two teeth. This form of injection is usually used for procedures involving maxillary teeth and bone, and for procedures involving the mandibular anterior teeth and bone. Field block anesthesia cannot be used in the mandibular posterior area because the bone there is too dense to allow the anesthetic solution to penetrate to the terminal nerve branches that innervate (provide sensation to) the teeth.
Peripheral Nerve Block Anesthesia
Peripheral nerve block anesthesia involves the injection of anesthetic solution near a main nerve trunk. In dentistry, this form of anesthesia is used for procedures involving the mandibular teeth and bone. The injection is made in the mandibular retromolar area (distal to third molar). This is commonly referred to as a mandibular block. The area involved is much greater than that for infiltration or field block anesthesia; one half of the patient's lower jaw will be anesthetized, including the tongue and lip.
Supplemental Local Anesthesia
There are some instances when the clinician may need to utilize other types of techniques in getting the area numb. Three of the more common techniques include: intraosseous, periodontal ligament injection, and intrapulpal injection anesthesia.
Intraosseous Anesthesia
Intraosseous anesthesia is used when the dentist has difficulty achieving pulpal anesthesia. For this type of injection, the anesthetic agent is delivered directly into the bone. An incision is made in the gingiva, and then a small round bur is used to make an opening in the bone, into which the anesthesia is injected. A perforator may also be used to make an opening in the bone. This is a solid needle that is attached to a slow-speed handpiece, which will perforate the bone. The anesthesia is then delivered through the opening with an 8 mm, 27 gauge needle.7
Periodontal Ligament Injection
The periodontal ligament injection (or intraligamentary injection) is a form of infiltration injection and is used to anesthetize one or two teeth in a quadrant. Typically it is used as an adjunct to field or nerve block injections when these methods are failing to provide adequate anesthesia for the patient. The anesthetic solution is delivered under pressure directly to the periodontal ligament and surrounding tissues. Generally, a special periodontal ligament injection syringe is used.
Intrapulpal Injection
If the clinician is having difficulty obtaining anesthesia during endodontic therapy (root canal), they may perform an intrapulpal injection. The anesthetic agent is delivered directly into the pulp chamber or canal after the pulp chamber has been exposed.
Relationship of Maxillary Nerve to Maxilla
Remember that the maxillary nerve branches into three different areas: one above and just posterior to the second molar, one branch just above the premolar, and one around the canine for the canine and lateral and central incisor. These are usual injection sites.
Relationship of Mandibular Nerve to Mandible
The mandibular nerve comes through the mandible just around the apex of the premolar or canine and exits. This is often the site of injection, and sometimes fibers from this nerve cross the midline, which can affect the profoundness of the anesthesia.
TECHNIQUES FOR DELIVERING ANESTHESIA
Allied staff is often responsible for preparing the anesthetic syringe for use by the provider who will administer the local anesthesia. When assembling a syringe, always wear gloves and protective eyewear, keep the needle sterile, and use care to avoid needlesticks. Keep the needle pointed away from you at all times.
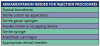
Armamentarium and Preparation of Syringe (Figure 5A and Table 4)
Needles are capped on two sides. Unlock the cap from the shortest side, holding the sharp end away from you. Screw this side of the needle into the hub of the syringe. Then, holding the syringe in one hand, insert an anesthetic cartridge into the syringe. At the same time use the other hand to pull back on the plunger, making room for the cartridge. Always keep the patient side of the needle capped and sterile at all times. The steps for assembling a syringe are summarized in Table 5.
Needles are available in long, short, and extra short lengths. Short lengths are used for maxillary buccal injections or palatal injections and never for mandibular blocks. Extra short needles are used for periodontal ligament anesthesia. A long needle is used for mandibular blocks or for designated posterior maxillary injections, as specified by the dentist. Needles also come in different gauges. Needle gauge correlates with the diameter of the needle; the smaller the number, the greater the diameter of the needle. (International standard 9626, Amendment 1, Stainless steel needle tubing for the manufacturer of medical devices. 2001)
Alternative Techniques
Many techniques may be used to minimize the discomfort and pain associated with the administration of anesthesia, some of which the dental assistant can perform.
• Always explain the procedure to the patient in advance.
• Use relaxation techniques to ease the patient's anxiety.
• Use vibrating devices, such as Vibraject® or DentalVibe®.
VibraJect®
Although its efficacy is still being studied, the VibraJect® is attached to the anesthetic syringe and when engaged causes the syringe and needle to vibrate. Pain is reduced through the Gate Control Theory. This theory is based on the fact that the vibration message is carried to the brain through insulated nerves and the pain message is carried through smaller uninsulated nerves. The insulated nerves overrule the smaller uninsulated nerves. The vibration and hum of the motor may also have a calming effect. (Figure 11)
Dental Vibe®
The DentalVibe® gently stimulates the sensory receptors at the injection site, causing the neural pain gate to close which blocks the pain of injections. An advantage to this system is that the tissue is vibrated before the needle penetrates. A disadvantage is this is a separate unit and not attached directly to the syringe, so that both hands are engaged with this technique.20, 21 (Figure 12)
Other Techniques
Other techniques that dentists can employ include:
• Neutralizing the acidic properties of the anesthetic by using sodium bicarbonate, such as Onset®, as a buffering agent that reduces the burning sensation of the anesthetic. A buffering agent also reduces the time for anesthesia to become effective and is highly effective in situations where pH changes caused by local infection make profound anesthesia more difficult. The buffering agent is added to the anesthetic cartridge before injecting. (Figure 13)
• Using pinching or pressure during the application to distract the patient.
• Keeping the speed of the injection constant.
• Using vapocoolants before the injection.
• Using a topical anesthetic at the site before the injection.
• Aspirating the syringe immediately after the needle is in injection site to check for blood.
Of all the techniques used to reduce pain, those found to be the most effective were slow, constant administration of the anesthesia.22 The use of warming the anesthetic may actually cause a breakdown of the epinephrine or levonordefrin. This breakdown makes vasoconstriction less effective, which results in shorter anesthetic times. This practice is not recommended.
FACTORS AFFECTING LOCAL ANESTHETIC ACTIVITY CLINICALLY
There are several factors that can affect the activity of local anesthetic in the dental clinic:
Dosage
An increase in the dose of a local anesthetic will increase the probability of a successful block by producing a solid and long-lasting anesthetic while decreasing the time to onset. An increase in the volume of local anesthetic using the same dose of local anesthetic does not appear to be beneficial in the clinical setting with the exception of the spread associated with epidural anesthesia, which normally is not done in dentistry unless the dental patient is being seen in a hospital setting.
Addition of Vasoconstrictors (Table 6)
Epinephrine is the most commonly used vasoconstrictor in local anesthetics. The usual dose and concentration is 5 mcg/ml or 1:200:000. Norepinephrine and phenylephrine have been used as vasoconstrictors, but do not exhibit properties that make them superior to epinephrine. Epinephrine acts to decrease vascular absorption, reduces blood concentration of local anesthetics, and decreases the risk of toxicity, thus allowing more local anesthetic molecules to reach the nerve membrane. As more molecules reach the nerve membrane, there is an increase in the depth and duration of the local anesthetic blockade. Epinephrine extends the duration of blockade for most short- to moderate-acting local anesthetics. The addition of epinephrine for neuraxial blockade has the added benefit of activating endogenous analgesic mechanisms through α-Adrenergic receptors. This may increase the intensity of analgesic action.
Site of Injection
The anatomical location of blockade influences onset and duration. Location affects the rate of diffusion, vascular absorption, and the amount of local anesthetic administered. Subarachnoid blockade exhibits the most rapid onset and shortest duration of action. Rapid onset, within the subarachnoid space, occurs because nerve roots are not covered with a sheath. The short duration of action is related to the small dose and volume of local anesthetic used to produce anesthesia. Brachial plexus blockade, in contrast, has slower onset and longer duration of action. Local anesthetics are deposited in the sheath around the brachial plexus. Diffusion must take place before reaching the site of action. The long duration of action is related to slow vascular absorption, large doses, and increased exposure of neural tissue to local anesthetics.
Carbonation and pH adjustment
In the isolated nerve, adding carbon dioxide to the local anesthetic solution accelerates the onset of blockade. This is a result of an increase in the base form of the local anesthetic, direct effect of CO2on the nerve, and a decrease in the local pH. Clinically results are mixed. Sodium bicarbonate may also accelerate the onset of action. The addition of bicarbonate increases the pH, which in turn increases the amount of local anesthetic in the uncharged base form. This theoretically accelerates the rate of diffusion across the sheath and membrane, resulting in a faster onset. Controversy exists concerning the clinical utility of pH adjustment. Studies remain ambiguous concerning the use of sodium bicarbonate to improve the speed of local anesthetic induced anesthesia.
Pregnancy
Hormonal changes during pregnancy are primarily responsible for the enhanced potency of local anesthetics. There is a correlation between progesterone levels and the mg per segment requirement of lidocaine required for the patient. Based on current research, the dosage of local anesthetics should be reduced for the pregnant patient by 30%, regardless of the trimester of pregnancy.
Mixtures of Local Anesthetics
Dental providers occasionally will combine local anesthetics to achieve quick onset and long duration. Often the provider will combine a local anesthetic with a fast onset with a local anesthetic that has a long duration of action to achieve this goal. Clinically there are few advantages to this technique. It should be noted that when mixing local anesthetics the risk of toxicity remains. Care should be exercised not to exceed the maximum dose. Toxicities of local anesthetics are not independent, but additive. A solution containing 50% of the toxic dose of local anesthetic A, and 50% of the toxic dose of local anesthetic B, will have the same implications as 100% of the toxic dose of either local anesthetic alone.
OCCUPATIONAL SAFETY AND RELATED REGULATIONS AND RECOMMENDATIONS
Avoiding needlesticks to the dental professional and patient is the biggest safety concern. Handling of the syringe post-injection, as well as during disassembly, are the two main times needlesticks occur. After the injection procedure, the needle is contaminated with patient blood and fluid. Therefore, never pass an uncapped needle after a procedure and never point an uncapped needle toward the body. Following injection, recapping of needles by hand is not recommended, as needlestick injuries can occur.
Use a recapping device for needles where possible. A variety of recapping devices are available; an example appears in Figure 14. If a recapping device is not available, the one-handed "scoop" technique is preferred for recapping needles between multiple injections on the same patient. The dentist should not pass the syringe back to the assistant. Instead, the dentist should recap the syringe.
Precautions should be taken when disassembling the syringe; always wear heavy or neoprene gloves when cleaning instruments prior to sterilization processing. Disassemble the syringe with the needle recapped by pulling back on the plunger, removing the cartridge, and unscrewing the needle from the syringe hub. Do not bend or break needles during disposal. Dispose of the needle and cover in a sharps container. When a sharps container is full to its "fill" line, dispose of it according to state or local regulations for biohazardous waste. Dental needles are intended for single use only; they should never be reused.
Occupational Injuries, OSHA, and CDC
Since there is no active surveillance of dental offices for disease transmission nationally, healthcare associated infections to dental professionals as a result of needlestick and other sharps injuries in dental offices are not quantified. However, case reports and legal cases provide ample evidence that transmission of bloodborne infections does occur; therefore, prevention of sharps injuries is very important. Should an injury occur, the patient should be referred for evaluation for risk of disease and the injured personnel should be offered post-exposure prophylaxis after consultation with an infectious disease expert within the local health department or hospital facilities. Your local contact should be listed in the sharps injuries protocol in your office.
The Centers for Disease Control and Prevention (CDC) estimate that approximately 600,000 to 1,000,000 needlestick and other percutaneous injuries occurred annually among U.S. healthcare workers, potentially exposing medical and dental team members to bloodborne pathogens such as human immuno-deficiency virus (HIV), hepatitis B virus (HBV), and hepatitis C virus (HCV). Numerous studies have demonstrated that as part of an overall safety and injury-reduction program, the use of safer medical devices, such as needleless systems and sharps with engineered safety features can be extremely effective in reducing accidental sharps injuries. According to the CDC, 62 to 88 percent of sharps injuries potentially could be prevented through the use of such devices. (Figure 15)
Although the 1991 federal Occupational Safety and Health Administration (OSHA) Bloodborne Pathogens Standard (29 CFR 1910.1030) required the use of engineering controls to help decrease the risk of occupational sharps injuries in healthcare settings, the Needlestick Safety and Prevention Act adopted by Congress in 2000 called for expansion of the OSHA standard.23The resulting 2001 revision of the Bloodborne Pathogens Standard specifically requires the review and consideration of "sharps with engineered sharps injury protections." For dental applications, such devices include safety needles and/or safety syringes that may be used to deliver local anesthesia. (Figure 16A and 16B) The revised standard clarifies the need for employers to select safer needle devices and to involve employees in identifying and choosing these devices. The updated standard also requires employers to maintain a log of injuries from contaminated sharps. Since the law went into effect in 2001, the number of reported needlestick injuries has decreased by one-third.24
The revised OSHA standard now requires:
• annual consideration and implementation of appropriate engineering controls, including needleless systems and/or sharps with engineered sharps injury protections;
• inclusion of non-managerial healthcare workers in evaluating and choosing devices; and
• documentation of these efforts within the practice setting's OSHA-required exposure control plan.
To comply, at least annually the employer must:
• review newly available devices designed to reduce sharps injuries;
• document consideration of sharps with engineered safety features as well as use of appropriate, commercially available, effective safer devices; and
• document employee involvement in the device review evaluation process.
Because OSHA recognizes that no one medical device can be considered appropriate or effective for all circumstances, it defines an "appropriate" safer medical device as one whose use, "based on reasonable judgment in individual cases, will not jeopardize patient or employee safety or be medically contraindicated." OSHA defines an "effective" safer medical device as one that, based on reasonable judgment, will make an exposure incident involving a contaminated sharp less likely to occur. To help determine if available safer sharps devices are appropriate and effective in the individual practice setting, CDC has created a set of sample Screening and Evaluation Forms, with an introduction that explains the process of safely evaluating new sharps safety devices for the individual practice setting.
Post-Exposure Management
Even with engineering controls in place, accidents can happen. Needlesticks and other occupational sharps injuries are considered medical emergencies and must be evaluated promptly by a qualified health care provider to best decrease the risk of transmission of infection with HBV, HCV, HIV, or other bloodborne pathogens. In the current "Guidelines for Infection Control in Dental Health-Care Settings, 2003,"24 CDC provides detailed information on post-exposure management.
The Needlestick Safety and Prevention Act also calls for health care facilities to maintain a sharps injury log. A sharps injury log can provide valuable information on the products and work practices within the dental setting that are most commonly implicated in occupational injuries. In turn, such information may be used to develop interventions that reduce or eliminate those risks within the practice setting.
A comprehensive sharps injury log must include detailed information on the percutaneous injuries sustained in the practice setting, including:
• the type and brand of device involved in exposure incidents,
• the department in which the exposure occurred, and
• an explanation of how the injury occurred.
States that have their own OSHA plans are required to have regulations that are "at least as effective" as those prescribed by the federal OSHA regulations. As such, dental practices operating in areas with state-run OSHA plans should ensure that they are in full compliance with the rules for their state. In addition, many states require that newly introduced engineering controls for injection equipment be reviewed by the state. Check your state OSHA requirements, as state OSHA requirements may vary depending on the state.
MANAGING EMERGENCIES
Emergencies, including life-threatening events, can happen to anyone at any time, but the stress associated with dental procedures can increase the risk that they may occur. About half of all emergencies occur around the time of injection, so be prepared with a written protocol. In addition to the steps that dentists can take while administering anesthetics, the dental assistant can help prevent some emergencies by always following some certain procedures25:
• Never underestimate the importance of the medical history. Always obtain complete information about any change in health status or drugs at the preoperative appointment and update it at the beginning of each appointment.
• Before the local anesthetic is administered, address any fears or nervousness the patient may be experiencing.
• Make sure the patient is in a supine position for the injections.
• Watch patients throughout the administration of anesthetics. Do not leave them alone following the injection.26
To be prepared for any contingencies, dental offices must not only have a plan for managing emergencies, but also review the written plan on a regular basis. The plan should include procedures for addressing events such as patient unconsciousness, breathing problems, seizures, drug-related reactions, or chest pain. The most important part is to know who will call 911 in the case of any life-threatening emergency. Life-threatening emergencies include a patient having difficulty breathing, chest pains, or difficulty swallowing and/or immediate facial swelling or redness.
Plans should exist in writing and should detail the role of each team member in case of an emergency. Different offices have different capacities for managing emergencies, from minimal to full resuscitation procedures. All team members should know how their offices manage medical emergencies. Report any unusual occurrence or destabilization of the patient to the dental provider immediately. In case of a medical emergency, know who in the office is responsible for calling 911 immediately.
• In an emergency, ensure that someone remains with the patient at all times, monitoring breathing and heart rate until the emergency is past or emergency medical personnel arrive.
• Be prepared to assist with cardiopulmonary resuscitation (CPR). The American Heart Association and the American Red Cross provide basic life support classes, and many states require dental health care workers to complete these courses. Be familiar with the procedures used in the office.
• Know the location of the emergency kit or equipment as well as the staff members who have access to it. Because of the kinds of medication it contains, these kits are often locked so be sure to know where to locate the key.
Emergency procedures should be explained to new employees on their first day on the job. The entire staff should practice staged emergencies at least semiannually; medical-emergency training records should be kept along with the OSHA-required training records. The office emergency kit should include the drugs and equipment necessary for addressing a wide range of emergencies. Emergency oxygen should be available as well. Everyone in the practice setting should know how to access this kit or equipment and how to correctly use it.
Allergic reactions are among the most common life threatening emergency in the dental setting and must be addressed promptly. Specific plans should be in place for managing allergies to local anesthetics in patients and should be regularly reviewed with the entire treatment team. While allergic reactions are rare, they can occur.26 A speedy response, including calls to 911 by a designated staff member, should be part of the plan. Response plans should be reviewed quarterly and in annual OSHA training to assure a prompt response to any potentially life-threatening allergic reactions.
NEW TECHNOLOGIES
Although Cook invented the modern dental syringe more than one hundred years ago, it is only recently that anesthetic delivery systems have seen major innovations. One new device, the STA or Single Tooth Application Wand™ (Figure 17), uses a microprocessor to control the delivery of a small amount of anesthesia ahead of the needle, thus ensuring a steady flow of anesthetic through the needle into the tissue. According to the manufacturer, this delivery method reduces the amount of pain that patients experience and increases their comfort. In addition, delivering anesthesia using this device may help patients avoid numbness of the tongue, lips, face, and other muscles.
The Wand/Single Tooth Application Wand
In response to the Needlestick Safety and Prevention Act, delivery devices, such as the STA and The Wand ™ (Figure 18) have been developed with engineering controls for anesthesia delivery. The safety system has a pen-like grasp that allows maximum tactile control and an auto-retracting design that shields the needle when not in use. The rate of injection is at a preprogrammed technique-specific rate selected by the dentist. A disposable cartridge sheath is required for each patient, but a standard dental needle and anesthetic cartridge can be used with this device. There are likely to be more delivery syringes available in the near future.
As with any medical device, follow the manufacturer's instructions for use, and apply the same safety principles as when handling any other sharp device. In addition, a nasal spray mist will soon be available for use to anesthetize maxillary teeth that will not use a needle. The tip is inserted and sprayed into the nasal cavity.
Needleless Jet-Injection Syringe Systems
Jet-injection devices are local anesthetic delivery systems that use pressurized force rather than needles to deliver local anesthetic to oral tissues. These systems were originally developed for mass immunization; however, they have been found to be useful in the delivery of local anesthetic to many areas of the oral cavity. High pressure forces the anesthetic from the carpule directly into the tissues with great precision. Considerably less anesthetic solution is used to achieve a rapid onset. Occasionally jet injection will be insufficient for select dental procedures. In those cases, it may then be used to accomplish more efficient topical anesthesia to allow for the painless administration of local anesthetic by needle injection into the deeper tissues. Many of the jet systems used in dentistry utilize the traditional dental anesthetic carpule. Since very little of the anesthetic solution is used during each injection, a single carpule can be used for multiple injections on separate patients. Because no part of the device penetrates the patient, it is only necessary to change the disposable tip that touches the patient before using again. However, sterilization between patients is recommended. Jet injection offers a great advantage in ensuring local anesthesia in persons with a phobia of classic injection (needle penetration). Other advantages of jet injection systems for the delivery of local anesthetic include rapid onset of anesthesia, predictable topical anesthesia of soft tissues, controlled delivery of anesthetic dose, elimination of needle-stick injury, and high patient acceptance. The disadvantages are cost and the potential to frighten patients with the sudden noise and pressure sensation that occur on delivery of the anesthetic.
Computer-Controlled Systems for the Delivery of Local Anesthetic
A computer-controlled pump modeled after those used in intravenous administration of general anesthetics is now available in dentistry for the delivery of local anesthetics. It works by delivering a constant volume of anesthetic at constant pressure, which enables less painful delivery of the anesthetic. It is widely believed that pain associated with local anesthetic injection is attributed to factors such as fluid pressure on injection and flow rate. A computer-controlled delivery device houses a conventional local anesthetic carpule that is linked by tubing to a disposable, pen-like handle with an attached needle. The device is operated by means of a foot control that delivers local anesthetic at precise pressure and volume ratios. Prior to insertion of the needle, the "wand" device will deliver a jet of the anesthetic into the tissue to provide adequate topical anesthesia prior to insertion of the needle. The device is highly effective in all areas of the oral cavity, including those areas of dense connective tissue such as the hard palate. While the system has the advantage of patient acceptance and ease of anesthetic delivery, disadvantages are higher cost and speed of injection; at the slowest pump rate, a total of 4 minutes is required to completely express a carpule.
Local Anesthetic Reversal Agent
The most annoying side effect of local anesthesia with vasoconstrictor is the lingering numbness of the soft tissue associated with minor dental procedures. This numbness may cause drooling, a crooked smile, diminished ability to speak properly, and injuries from unknowingly biting the lips, cheeks, and/or tongue. Among children, post-anesthetic trauma can occur when they chew the lip or tongue. This has the potential to be serious for young children. In addition, busy patients must often return to work or school without residual numbness.
Phentolamine Mesylate, sold under the brand name of OraVerse® (Figure 19), is an anesthetic reversal agent that reduces time of numbness by half. It is injected using the same technique that is used in local anesthesia, with about half the dosage of anesthetic used. Although not covered yet by insurance, it is becoming a standard of care in many practices. It is not indicated in children under 6 years of age or persons weighing less than 33 lbs.27, 28
SUMMARY
The success of the contemporary dental practice largely hinges on the use of local anesthesia for ensuring patient comfort and safety. Dental professionals should be aware of proper methods for handling syringes and needles, avoiding needlestick and sharps injuries in the office, complications of anesthesia, and how to manage any emergencies. A periodic review of anesthesia techniques is important for keeping abreast of recent developments in dental pain control. The review should include an introduction to new anesthetics, innovations in anesthesia or delivery devices as well as a discussion of complications of local anesthetics and their administration. Infection control and sterility should be maintained during all anesthetic procedures. Should a needlestick occur, manage the exposure immediately according to OSHA regulations and CDC recommendations.
References
1. Fillebrown T. A Textbook of Operative Dentistry. Philadelphia, P. Blakiston, Son & Co., 1889.
2. Reed KL. A Brief History of Anesthesiology in Dentistry. Texas Dent J 2002 Mar; 219-224. https://www.ncbi.nlm.nih.gov/pubmed/11922013. Accessed November 14, 2018
3. ADA House of Delegates. Guidelines for Teaching the Comprehensive Control of Pain and Anxiety in Dentistry. 2007. www.ada.org/sections/about/pdfs/anxiety_guidelines.pdf Accessed November 14, 2018.
4. Scarlett MI. Current Concepts in Local Anesthetics. Woman Dent J. 2004 Apr; 32-38. http://www.dentistryiq.com/articles/wdj/print/volume-2/issue-4/focus-on-anesthesia/current-concepts-in-local-anesthetics.html Accessed November 15, 2018.
5. Meechan JG. Effective Topical Anesthetic Agents and Techniques. Dent Clin North Am 2002 Oct; 46(4):759-66.
6. Bird, Doni, and Robinson, Debbie. Torres and Ehrlich Modern Dental Assisting. 8th ed., St. Louis: Elsevier Saunders 2005.
7. Phinney, Donna J., and Haldstead, Judy H. Delmar's Dental Assisting: A Comprehensive Approach. 2nd ed.; Clifton Park, New York. Delmar 2004.
8. Finkbeiner, Betty Ladley, and Johnson, Claudia Sullens. Mosby's Comprehensive Dental Assisting: A Clinical Approach. St. Louis: Mosby, 1995.
9. Malamed, SF, Reed, KL, and Fonner AM. Local Anesthesia Part 2: Technical Considerations. Anesth Prog. 2012 Fall; 59(3): 127-137. doi: 10.2344/0003-3006-59.3.127 PMCID: PMC3468291
10. Requa-Clark, Barbara, and Holroyd, Sam V. Applied Pharmacology for the Dental Hygienist. 3rd ed., St. Louis: Mosby, 1995.
11. Uckan S, Guler N, Sumer M, Ungor M. Local Anesthetic Efficacy for Oral Surgery: Comparison of diphenhydramine and prilocaine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998 Jul;86(1):26-30.
12. Haas DA. Localized Complications from Local Anesthesia. J Calif Dent 1998;26: 677-682.
13. Shojaei AR, Haas DA. Local Anesthetic Cartridges and Latex Allergy: A Literature Review. J Can Dent Assoc 2002 Nov; 68(10):622-6.
14. Haas DA, Lennon D. A 21-year Retrospective Study of Reports of Paresthesia following Local Anesthetic Administration. J Can Dent Assoc 1995:61:319-330.
15. Haas DA. Localized Complications from Local Anesthesia. J Calif Dent 1998; 26: 677-682.
16. Finder RL, Moore PA. Adverse Drug Reactions to Local Anesthesia. Dent Clin North Am 2002
17. Blanton PL, Jeske AH. Dental Local Anesthetics: Alternative Delivery Methods. JADA 2003 Feb;134(2):228-34.
18. Blanton PL, Jeske AH, ADA Council on Scientific Affairs, ADA Division of Science. Avoiding Complications in Local Anesthesia Induction: Anatomical Considerations. JADA 2003 Jun; 134(6):753-60.
19. Kaweckyj N. Maxillofacial Surgery Basics for the Dental Assistant. Part I. American Dental Assistants Association 2016.
20. Hirst, L. Good Vibrations? - DentalVibe vs. Vibraject. Dental Anxiety Network: December 9, 2013. http://www/dentalanxiety.net/gadgets/dentalvibe-vs-vibrajet. Accessed December, 1, 2018.
21. Saijo, M, et al. Lack of Pain reduction by a Vibrating Local Anesthetic Attachment: A Pilot Study. Anesthesia Progress. American Dental Society of Anesthesiology: Summer 2005: 52(2): 62-64. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2527045. Accessed December 1, 2018.
22. Meit S, et al. Techniques for Reducing Anesthetic Injection Pain-an Interdisciplinary Survey of Knowledge and Application. JADA 2004 Sep; 135:1241-1250.
23. U.S. Congress. The Needlestick Safety and Prevention Act (HR 5178). Available at http://www.osha.gov/SLTC/etools/hospital/hazards/sharps/sharps.html. Accessed November 30, 2018.
24. CDC. Guidelines for Infection Control in Dental Health-Care Settings-2003. MMWR Morbid Mortal Weekly Report December 19, 2003;52 (RR17);1-61.
25. Protzman S, Clark J. The Dental Assistant's Management of Medical Emergencies. American Dental Assistants Association 2017.
26. Blanton PL, Jeske AH. Misconceptions Involving Dental Local Anesthesia. Texas Dent J 2002; 119(4): 296-307.
27. Tavares M, et al. Reversal of Soft-Tissue Local Anesthesia with Phentolamine Mesylate in Pediatric Patients. JADA 2008 Aug; 139, 1095-1104
28. Hersh EV, et al. Reversal of Soft-Tissue Local Anesthesia with Phentolamine Mesylate in Adolescents and Adults. JADA 2008 Aug; 139, 1080-1093
About the Authors
LOCAL ANESTHESIA IN TODAY'S DENTAL PRACTICE (1436) original author:
Margaret I. Scarlett, DMD, is an accomplished clinician, scientist, and lecturer who retired from the Centers for Disease Control and Prevention after 23 years of federal service. She is a past author and editor of several dental publications, and a past president of the American Association of Women Dentists. As an innovator, including writing the very first 1986 CDC infection control guidelines for dental health-care workers, she continues to explore new and better ways to deliver prevention, care and treatment of the oral cavity. She consults on intraoral health and primary care and is a leading dental expert in infectious and chronic diseases and systemic-oral health issues.
This course has fully been updated and revised and published under a new name by:
Natalie Kaweckyj, LDA, RF, CDA, CDPMA, COA, COMSA, CPFDA, CRFDA, MADAA, BA, began her dental assisting career over 25 years ago after graduating from the CODA accredited program at ConCorde Career Institute. She spent twelve years working in a private practice where she worked clinically nine years and administratively the remaining three. She then moved onto teaching dental assisting and eventually became director of that program. Over lapping with teaching, Natalie began her tenure with Children's Dental Services in 2007 in management and currently serves as clinical coordinator responsible for the day to day operations at over 600 locations where services are provided throughout Minnesota. Natalie enjoys the challenges of the public health sector and is gratified in serving those that are underserved, especially in a hospital setting under general anesthesia. With over a decade of restorative functions experience under her belt, she enjoys working with professionals new to dentistry as her love for teaching comes into play with the utilization of clinicians to the full scope of their licenses. The clinic keeps Natalie busy with billing management when not at the hospital. Natalie also graduated with a BA in Biology and Psychology from Metropolitan State University in 2005.
Ms. Kaweckyj served two terms as ADAA President (2017-2018; 2010-2011). She remains active on several councils, and serves as a President of the Professional Dental Assistants Educational Foundation (PDAEF). She served as a three-term president for MnDAA and remains as the state business secretary. Natalie has been recognized with several ADAA awards, was one of the first ADAA Fellows in 1999 and became the first ADAA Master in 2004. She has published numerous continuing education courses, over 200 articles and lectures on a variety of dental subjects locally, nationally and internationally. Organized dentistry gave Natalie the insight that you can make a difference as a dental professional, and she was instrumental in seeing licensure for dental assistants come to fruition in MN in 2009 as well as several expanded functions. Her dream would be to see mandatory credentialing become a reality in all states for protection of the public and maintaining integrity of the dental assisting profession.