You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Nausea and vomiting is one of the most common postoperative complaints from patients following general anesthesia, second only to pain. Its occurrence is miserable for the patient and both troubling and perplexing to the provider. It is not surprising that a staggering number of publications have been dedicated to the prevention and management of this complication. Unfortunately, its pathophysiology is incompletely understood, and the many contributing factors have rendered the majority of these publications inconclusive. In many cases, this has spawned misconceptions and anecdotes that are not scientifically grounded. This continuing education article summarizes current thinking and guidelines on the subject and also addresses the issue of hiccups, a less frequent but nevertheless troubling complication.
DEFINITIONS AND PHYSIOLOGY
Postoperative nausea and vomiting (PONV) is the conventional title for this complication, and PONV has become the official medical subject heading in the National Library of Medicine. However, this label should not detract from the fact that nausea and vomiting are distinct entities that may occur at any point during or after a clinical procedure. Vomiting or emesis, which is the actual oral expulsion of gastrointestinal contents, is the result of contractions of the gut and the thoracoabdominal wall musculature. This contrasts with regurgitation, which is the effortless passage of gastric contents into the mouth. Retching is the term used to describe the muscular events of vomiting without expulsion of vomitus (ie, dry heaves). The term nausea refers to a subjective feeling of the need to vomit. The nauseated patient does not necessarily vomit or retch. Nausea should be distinguished from dyspepsia (upset stomach), which encompasses epigastric burning, gnawing discomfort, bloating, or pain. It is not uncommon for nausea to accompany dyspepsia, but they are distinct events.
The vomiting center lies in the medulla oblongata and comprises the reticular formation and the nucleus of the tractus solitarius. When activated, motor pathways descend from this center and trigger vomiting. These efferent pathways travel within the 5th, 7th, 9th, 10th, and 12th cranial nerves to the upper gastrointestinal tract, within vagal and sympathetic nerves to the lower tract, and within spinal nerves to the diaphragm and abdominal muscles.1 The vomiting center can be activated directly by irritants or indirectly following input from four principal areas: the gastrointestinal tract, the cerebral cortex and thalamus, the vestibular region, and the chemoreceptor trigger zone (CRTZ). The CRTZ is closest in proximity, lying between the medulla and the floor of the fourth ventricle. Unlike other brain centers, it is not protected by the blood-brain barrier. This is to say that the endothelium of its capillaries is not tightly joined or surrounded by glial cells and is permeated easily by irritants regardless of their lipid solubility or molecular size. The components of this vomiting network are illustrated in Figure 1, along with principal receptors and ligands that provide activation.
Before vomiting occurs, there may be a period of antiperistalsis, in which rhythmic contractions occur up the digestive tract instead of downward. This may commence as far down as the ileum, with the antiperistaltic wave pushing contents of the lower small intestine contents upward into the duodenum and stomach within a few minutes. Then, distention within these upper portions of the gastrointestinal tract generates afferent impulses to the vomiting center, where the actual act of vomiting is initiated.1 For this reason, an empty stomach does not preclude the expulsion of vomitus. At the onset of vomiting, intrinsic contractions occur in both the duodenum and the stomach, the lower esophageal sphincter relaxes, and vomitus moves from the stomach into the esophagus. Next, the inspiratory and abdominal muscles contract and expel the vomitus into the mouth.
FACTORS CONTRIBUTING TO PONV
PONV is multifactorial in its origin. In addition to well-established emetogenic agents such as opioids and inhalation anesthetics, a large number of factors appear to render patients more susceptible. Patient-related factors with the most established significance include female gender, nonsmoking history, anxiety and prior history of PONV, motion sickness, and migraine. No explanation has been offered for the increased incidence in female patients, but this increased risk persists throughout life, even following menopause, which obviates any role for estrogen as a factor. It is speculated that smokers may have developed some tolerance because of the chronic emetogenic influence of nicotine, which is lacking in the nonsmoker. A history of motion sickness suggests a more susceptible vestibular component. Nevertheless, it is surprising that none of these factors is a reliable predictor independently. For example, a prior history of PONV would intuitively suggest high risk, but female gender is actually a stronger independent predictor.2
The nature and extent of the surgical procedure have been studied extensively. The most commonly cited procedures and their possible mechanisms are as follows: tympanoplasty (vestibular stimulation), ENT and oral surgery (swallowed blood), breast surgery (anxiety and emotional load), laparoscopy (peritoneal irritation), and abdominal and hysterectomy (GI and vagal stimulation). With the exception of strabismus surgery in children, no surgical procedure is a sound independent predictor. PONV in these cases more likely reflects prolonged exposure to emetogenic anesthetics and underlying patient-related factors.3 Emetogenic agents have the strongest evidence for risk of PONV. Patient and surgical risk factors likely play a role in the susceptibility to these agents. Opioids have well-established emetogenic effects. The degree of risk is predicated on the total dose administered, not on the particular agent or whether it is administered intraoperatively or postoperatively.3 Furthermore it occurs more frequently following ambulation, which suggests a vestibular component in its pathogenesis. Inhalation anesthetics are also well-established emetogenics, with the volatile agents more so than nitrous oxide.4-6 Their degree of risk is directly related to duration of exposure. Propofol is commonly regarded as an antiemetic, but whether nonsedative doses actually impart an antiemetic influence is equivocal.7,8 At sedative doses, however, both propofol and midazolam appear to increase threshold for postoperative nausea.9 Nevertheless, there is little doubt that propofol is far less emetogenic than the inhalation agents.4,10
ANTIEMETIC DRUGS
The efficacy of antiemetic drugs is predicated on their ability to act as antagonists at receptor sites within the vomiting center and associated regions (Figure 1). From an empiric standpoint, those that block acetylcholine and histamine appear most useful when vestibular triggers are suspected, and dopamine blockade targets the emetogenic influence of opioids in the vomiting center and CRTZ. The serotonin antagonists act not only in the vomiting center but also within the GI tract, where surgical manipulation or many of the chemotherapeutic agents generate their noxious influence. Anxiolytic medications are useful in cases where anticipatory anxiety is high. Despite the logic of these drug actions, more than a thousand publications have failed to clearly establish the superiority of a particular agent, regardless of risk factors. Part of this is due to inconsistency in study design, but it also reflects the extreme difficulty of factoring the many contributors and causes for both nausea and vomiting. Selected antiemetic drugs and their relative activity in blocking receptor sites are summarized in Table 1.11
Dopamine Antagonists
Drugs that block dopamine are effective antiemetics for most causes of PONV. Unfortunately, their ability to also block dopamine transmission within the basal ganglia may result in so-called extrapyramidal syndromes (EPSs) that include akathisia, parkinsonian symptoms, and tardive dyskinesia. Of these syndromes, akathisia is most common and presents as a subjective feeling of restlessness leading to a compelling need to move. Patients feel that they must get up and walk or continuously move about. This behavior may be mistaken for agitation, and their distinction is critical to avoid an inclination to further sedate the patient. Although extrapyramidal symptoms are bizarre and generally frighten the patient and practitioner alike, they are never fatal. Like Parkinson’s disease, this syndrome reflects not only a defect in dopaminergic transmission, but also a relative excess of cholinergic activity within the basal ganglia. For this reason, the more specific anticholinergic actions of diphenhydramine are useful for countering acute episodes.12 Promethazine (Phenergan) and prochlorperazine (Compazine) are among the most commonly used antiemetics. In the emergency room setting, promethazine was found to have a greater sedative effect, but prochlorperazine was more effective as an antiemetic with a similar incidence of akathisia.13,14
In addition to its antidopaminergic action, metoclopramide (Reglan) has a prokinetic action on the upper digestive tract. By acting as an agonist at a specific subtype of serotonin receptor (5-HT4), it simultaneously increases tone in the lower esophageal sphincter and increases gastric motility, both of which promote gastric emptying. These actions make it an attractive antiemetic in patients with a history of gastroesophageal reflux.
Many antiemetic and psychotropic drugs that have dopaminergic and cholinergic blocking activity have been implicated in producing a prolonged Q-T interval, an electrocardiographic change that may trigger tachyarrhythmias such as torsades de pointe. Recently, this has been a well-published concern for droperidol. However, this worry was spawned by case reports wherein large doses were administered in hospital emergency departments and intensive care units. This proarrhythmic side effect is not considered relevant at low antiemetic doses, that is, those not exceeding 0.625 mg.3
5-HT3 (Serotonin) Blockers
The 5-HT3 (serotonin) antagonists were introduced initially to combat radiation and chemotherapy-induced nausea and vomiting. This was based on pivotal roles for radiation, cisplatin, and other chemotherapeutic agents in triggering serotonin release within the gastrointestinal wall. The subsequent reduction in the cost of these antiemetics and additional understanding of the roles of serotonin within the vomiting center have expanded the use of 5-HT3 antagonists for PONV. Newer members of this class have not been found more effective than the initial prototype, ondansetron (Zofran).
Use of these agents is particularly attractive when drugs that have antidopaminergic or anticholinergic actions are to be avoided. Dopamine blockade obviously should be avoided if possible in patients with Parkinson’s disease. Severe dementias such as Alzheimer’s disease are due to degenerative changes in cortical cholinergic pathways, and drugs that have significant anticholinergic actions should be avoided.15
Novel Agents
Drugs that block the neurokinin 1 (NK1) receptor have proven efficacy in chemotherapy-induced nausea and vomiting. They are most effective in preventing delayed nausea and generally are used in conjunction with 5-HT3 antagonists for this reason. Aprepitant (Emend) is the first of these agents to be introduced, but its efficacy for PONV is not established. Likewise, the cannabinols such as tetrahydrocannabinol found in marijuana and dronabinol (Marinol), a synthetic derivative, have proven efficacy only for chemotherapy-induced nausea and vomiting.
Glucocorticoids such as dexamethasone are well-established antiemetics for chemotherapy-induced as well as postoperative nausea and vomiting. How they produce this effect is unknown, but it is speculated that they may suppress production of inflammatory autacoids that may somehow potentiate known vomiting pathways within the vomiting center. A similar mechanism has been proposed to explain the beneficial effects of nonsteroidal anti-inflammatory drugs in nausea and vomiting induced by systemic irradiation. Glucocorticoids have a slow onset of action, and their benefit is limited to prophylactic regimens.
Acupuncture has been fairly well established in the prevention of PONV.16 It consists of stimulating the so-called P6 wrist point (located on the ventral surface of the forearm approximately three fingerwidths proximal to the wrist joint) by using acupuncture, acupressure, and other techniques. The reader is referred to an excellent review of principles and devices by Chernyak and Sessler.17
Occasionally one hears anecdotal evidence regarding the use of ephedrine to prevent nausea and vomiting. This generally is related to obstetrical and other procedures performed under neuroaxial blockade, during which vasovagal and other causes for hypotension are implicated in precipitating PONV. Any antiemetic benefit is likely secondary to preventing these events. Likewise one hears mention of supplemental oxygen as conferring an antiemetic influence, but this also is untrue.18
Drugs of Choice
Results from an astounding number of clinical trials have not been able to clearly distinguish drugs of choice for specific clinical situations, especially for acute intervention. For the patient who is experiencing nausea and vomiting during the postoperative period, reasonable choices are promethazine, prochlorperazine, and ondansetron. Considering its low generic cost and low side effect profile, ondansetron is most attractive. In terms of prophylaxis, however, results from large meta-analyses favor the use of ondansetron, dexamethasone, or droperidol alone or in combination.3,19
PREDICTING AND MANAGING PONV
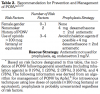
The routine use of prophylaxis for PONV is unwarranted. This is particularly true for moderate or deep sedation techniques using midazolam, propofol, and conventional doses of opioids. However, for patients with well-defined risks, especially when inhalation agents are to be used, prophylaxis may be justified. Apfel not only has authored an impressive list of clinical studies but also has performed an extensive analysis of the literature.3 His recommendation regarding risk assessment and management provides an excellent guideline for sedation and anesthesia in dental practice (Table 2).3,20
Management of Aspiration
If a patient experiences nausea, vomiting, or regurgitation, proper management can minimize any significant consequences. The nauseated patient may be more comfortable in Fowler’s or semi-Fowler’s position, but if vomiting or regurgitation occurs, or appears eminent, the patient should be placed in a reclined position, with the head lower than the chest and abdomen; a partial or full Trendelenburg is preferred. This will reduce the risk for aspiration. Also, the patient should be turned on the right side based on anatomical considerations. The right primary bronchus branches at a less acute angle from the trachea, and aspirated material is more likely to enter the right lung, at least initially. Turning the patient to the right side may spare the left lung from aspirant. While positioning the patient, initiate high-volume suctioning using a tonsil or Yankauer tip. Avoid placing the suction tip too deeply into the oropharynx to avoid triggering further retching and pushing vomitus farther into the obstructed airway.
When vomiting ceases, it is essential to evaluate the patient for possible aspiration. The patient should be supported with supplemental oxygen and both lungs auscultated. If any evidence of abnormal sounds such as wheezing or rhonchi is noted, or if oxygen saturation by pulse oximetry is decreased despite oxygen supplementation, the patient should be immediately transferred to an emergency department for further evaluation. If bronchospasm is suspected, management should follow that for an asthmatic attack; a bronchodilator should be administered (eg, albuterol 2 to 4 inhalations). If the patient cannot cooperate with this form of drug administration and the bronchospasm is severe, epinephrine 0.3 mg (a 1:1,000 concentration) should be administered intramuscularly for adults, or 0.15 mg for children. Intubation of the patient should be considered only when hypoxemia remains severe (eg, SpO2 <80), despite conventional efforts at oxygenation.
More extravagant treatment options such as bronchial lavage or administration of antibiotics and glucocorticosteroids are dated and rarely if ever viable.21,22 These may be indicated in the most severe cases, but they will be addressed more appropriately by the emergency room physician.
Hiccups
Hiccup (singultus) is a fairly common phenomenon that generally is only a nuisance but may become more troubling when prolonged. A hiccup consists of sudden contraction of the diaphragm and intercostal muscles followed immediately by laryngeal closure. They commence most often during inspiration and are inhibited by elevations in PaCO2; this serves as the basis for breath holding or breathing into a paper bag as a common therapeutic intervention.23,24
A so-called ‘‘bout’’ of hiccups may last for a day or two, but episodes lasting longer than 48 hours are labeled as persistent, and those lasting longer than 2 months are regarded as intractable.25 More than 100 causes of persistent or intractable hiccups have been identified, including infection, trauma, tumor, and a myriad of gastrointestinal, metabolic, and psychogenic disorders. In contrast, brief bouts of hiccups associated with anesthesia practice are more often precipitated by anesthetic medications or gastric distention from swallowing blood and debris.
The hiccup reflex is not fully understood but consists of three general components: an afferent limb traveling within the phrenic and vagus nerves, a central processor, and an efferent limb traveling within the phrenic nerve to the diaphragm and accessory nerves to intercostal muscles.25 The central processor is least understood but is located somewhere between the cervical spine and brainstem. Processing is provided by several poorly defined neurotransmitters, including gamma-aminobutyric acid (GABA) and dopamine.
Triggers for hiccups are conventionally described as central or peripheral in origin. Central mechanisms are implicated in intractable cases and appear related to various central nervous system disorders, including neoplasia.25,26 More often the origin of the triggering stimulus occurs peripherally in epigastric locations following gastric distention, irritation, or reflux.23-26 This would explain its occurrence following dental surgery, particularly in cases of excess swallowing of blood and debris. A number of drugs have been implicated in provoking hiccup, including certain antibiotics, antineoplastic agents, and dopamine agonists used in Parkinson’s disease.23-25 However, more familiar culprits to the dentist include the benzodiazepines, opioids, methohexital, and dexamethasone.25 It is difficult to define precise mechanisms because drugs known to induce hiccups (eg, benzodiazepines, antidopaminergic drugs) have also been used in their treatment.
Treatment for hiccups is obvious when the cause or trigger is identified. The use of proton pump inhibitors is effective targeted therapy for hiccups attributable to gastroesophageal reflux disease (GERD). Metoclopramide (Reglan) also may be used, as it promotes gastric emptying. More often, however, the cause is elusive, and most of the treatments are anecdotal or are based on dated publications that have failed scientific scrutiny. Nevertheless, most of these remedies are innocuous and will not harm the patient if attempted. They include rapidly swallowing water or ice chips, breath holding, and rebreathing from a paper bag.24-26 In all of these cases, a subsequent elevation in PaCO2 could explain positive results when they occur.
If hiccups continue for longer than an hour or two, despite attempts with innocuous remedies, pharmacological intervention can be considered. Many drug classes have been suggested in the scientific literature, each having distinctly different actions, but none of these have unequivocal efficacy. Chlorpromazine is most frequently cited and is the only agent that has been tried enough to receive US Food and Drug Administration approval for this indication. It can be administered as a single intramuscular or intravenous dose of 25 mg to 50 mg or can be prescribed orally as 25 mg three times daily. However, other antidopaminergic agents can be used as alternatives. These include prochlorperazine, droperidol, and metoclopramide in dosages used for postoperative nausea and vomiting. Additional options include baclofen 5 mg three times daily and gabapentin 300 mg three times daily, but these provide a more gradual response and are indicated for more chronic or prolonged episodes.24,25
Despite the many options, this author’s personal recommendation is to use nonpharmacological approaches initially, and if the episode continues or reappears following discharge, prescribe chlorpromazine 25 mg tabs three times daily for 1 to 2 days. One alternative deserves mention. Benzonatate (Tessalon Perles) is approved as an antitussive agent but has an established off-label use in hiccups. It is an ester local anesthetic derived from tetracaine. After absorption and circulation to the respiratory tract, it distributes into the mucosa, anesthetizing vagal afferent fibers that contribute to both cough and hiccups. The recommended dose is 100 mg PO every 4 hours, not to exceed 600 mg each day. To avoid excessive numbness of the mouth and throat, the patient must be warned against biting or chewing the medication before swallowing. Onset of action generally occurs within 20 to 30 minutes after administration, and improvement should follow one or two doses if this strategy is to be deemed effective.
About the Author
Dr. Becker is an Associate Director of Education, General Dental Practice Residency, at Miami Valley Hospital in Dayton, Ohio.
REFERENCES
1. Guyton AC, Hall JE. Textbook of Medical Physiology. 11th ed. Philadelphia, PA: Elsevier; 2006:823-824.
2. Apfel CC, Kranke P, Eberhart LH. Comparison of surgical site and patient’s history with a simplified risk score for the prediction of postoperative nausea and vomiting. Anaesthesia. 2004;59:1078-1082.
3. Apfel CC. Postoperative nausea and vomiting. In: Miller RD, Eriksson LI, Fleisher LA, et al, eds. Miller’s Anesthesia. 7th ed. Philadelphia, PA: Elsevier, Churchill Livingstone; 2009.
4. Gupta A, Stierer T, Zuckerman R, et al. Comparison of recovery profile after ambulatory anesthesia with propofol, isoflurane, sevoflurane and desflurane: a systematic review. Anesth Analg. 2004;98:632-641.
5. Leslie K, Myles PS, Chan MT, et al. Risk factors for severe postoperative nausea and vomiting in a randomized trial of nitrous oxide-based vs nitrous oxide-free anaesthesia. Br J Anaesth. 2008;101:498-505.
6. Myles PS, Leslie K, Chan MT, et al. Avoidance of nitrous oxide for patients undergoing major surgery: a randomized controlled trial. Anesthesiology. 2007;107:221-231.
7. Gan TJ, El-Molem H, Ray J, Glass PS. Patient-controlled antiemesis: a randomized, double-blind comparison of two doses of propofol versus placebo. Anesthesiology. 1999;90:1564-1570.
8. Scuderi PE, D’Angelo R, Harris L, et al. Small-dose propofol by continuous infusion does not prevent postoperative vomiting in females undergoing outpatient laparoscopy. Anesth Analg. 1997;84:71-75.
9. Hvarfner A, Hammas B, Thorn SE, Wattwil M. The influence of propofol on vomiting induced by apomorphine. Anesth Analg. 1995;80:967-969.
10. Apfel CC, Kranke P, Katz MH, et al. Volatile anaesthetics may be the main cause of early but not delayed postoperative vomiting: a randomized controlled trial of factorial design. Br J Anaesth. 2002;88:659-668.
11. Nasricha PJ. Treatment of disorders of bowel motility and water flux: antiemetics and agents used in biliary and pancreatic disease. In: Brunton LL, Lazo JS, Parker KL, eds. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 11th ed. New York, NY: McGraw-Hill; 2006.
12. Vinson DR, Drotts DL. Diphenhydramine for the prevention of akathisia induced by prochlorperazine: a randomized, controlled trial. Ann Emerg Med. 2001;37:125-131.
13. Ernst AA, Weiss SJ, Park S, et al. Prochlorperazine versus promethazine for uncomplicated nausea and vomiting in the emergency department: a randomized, double-blind clinical trial. Ann Emerg Med. 2000;36:89-94.
14. Drotts DL, Vinson DR. Prochlorperazine induces akathisia in emergency patients. Ann Emerg Med. 1999;34(4 Pt 1):469-475.
15. Dierdorf SF, Walton JS. Anesthesia for patients with rare and co-existing diseases. In: Barash PG, Cullen BF, Stoelting RK, eds. Clinical Anesthesia. 5th ed. Philadelphia, PA: JB Lippincott; 2006.
16. Lee A, Fan LT. Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting. Cochrane Database Syst Rev. 2009;(2):CD003281.
17. Chernyak GV, Sessler DI. Perioperative acupuncture and related techniques. Anesthesiology. 2005;102:1031-1049.
18. Orhan-Sungur M, Kranke P, Sessler D, Apfel CC. Does supplemental oxygen reduce postoperative nausea and vomiting? A meta-analysis of randomized controlled trials. Anesth Analg. 2008;106:1733-1738.
19. Apfel CC, Korttila K, Abdalla M, et al. A factorial trial of six interventions for the prevention of postoperative nausea and vomiting. N Engl J Med. 2004;350:2441-2451.
20. Gan TJ, Meyer T, Apfel CC, et al. Consensus guidelines for managing postoperative nausea and vomiting. Anesth Analg. 2003;97:62-71.
21. Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001;344:665-671.
22. Anderson E. Aspiration pneumonia and lung abscess. In: Tintinalli JE, Kelen GD, Stapczynski JS, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 6th ed. New York, NY: Access Emergency Medicine, McGraw Hill; 2010.
23. Ropper AH, Samuels MA. Disorders of the autonomic nervous system, respiration, and swallowing. In: Ropper AH, Samuels MA, eds. Adams & Victor’s Principles of Neurology. 9th ed. New York, NY: McGraw-Hill; 2009.
24. Aldrich TK, Tso R. The lungs and neuromuscular diseases. In: Mason RJ, Murray JF, Broadus VC, Nadel JA, eds. Murray & Nadel’s Textbook of Respiratory Medicine. 4th ed. Philadelphia, PA: Elsevier Saunders; 2005.
25. Smith HS. Hiccups. In: Walsh D, ed. Palliative Medicine. Philadelphia, PA: Elsevier Saunders; 2009.
26. Moretti R, Torre P. Hiccups. In: Bope ET, Rakel RE, Kellerman R, eds. Conn’s Current Therapy 2010. Philadelphia, PA: Elsevier Saunders; 2010.