You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Prior to a patient’s receiving a dental implant, the following procedures are usually completed: a medical and dental history; intraoral examination; updated radiographs; and casts, which may be mounted for evaluation. The clinician must foresee the completed prosthesis. If required, a diagnostic wax-up is made to study desired positions of teeth and soft tissue. A surgical guide is often employed to direct implant insertion buccolingually, mesiodistally, and apicocoronally. In addition, when the osteotomy is being developed, the 2-mm twist drill provides tactile feedback with respect to bone density. This furnishes the first clinical opportunity to assess osseous density to the full depth of the intended implant site and thereby facilitates altering the drilling sequence and treatment plan if necessary. Application of this information, which is referred to as treatment planning with a 2-mm twist drill, is discussed in this article.
Determining Osseous Density with a 2-mm Twist Drill
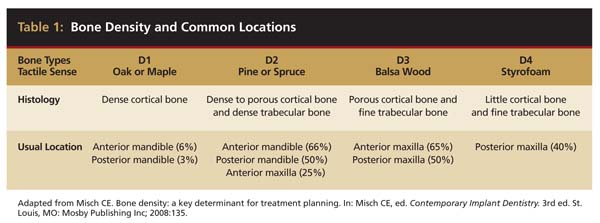
A round bur is usually used to mark the position where a 2-mm twist drill will be applied (Figure 1). Then the twist drill is employed to penetrate the cortical and trabecular bone (Figure 2). This provides information with respect to cortical bone thickness and medullary trabecular bone density. The amount of bone debris found on the twist drill can be interpreted as an indicator of bone quality (eg, the less debris and a more bloody appearance means softer bone). Four types of mineralized bone have been described by Misch (Table 1):1,2
- D1 feels like drilling into oak or maple.
- D2 feels like drilling into pine or spruce.
- D3 feels like drilling into balsa wood.
- D4 feels like drilling into Styrofoam®.
Tactile feedback from the 2-mm twist drill clearly facilitates differentiating between D1 and D4 bone; however, it is difficult to distinguish between the intermediate classes of bone quality (D2 and D3).3 Nevertheless, the amount of cortical bone at the crest determined with the twist drill can provide valuable information (Table 1).1,2
 |
In general, periapical and panoramic radiographs are poor indicators of bone density because lateral bony plates preclude accurate assessment of trabecular bone density. If a computed tomography (CT) scan is available, then bone density can be more accurately assessed.4 The higher the Hounsfield units, the denser the bone (D1: > 1250, D2: 850 to 1250, D3: 350 to 850, D4: 150 to 350) (Figure 3).5
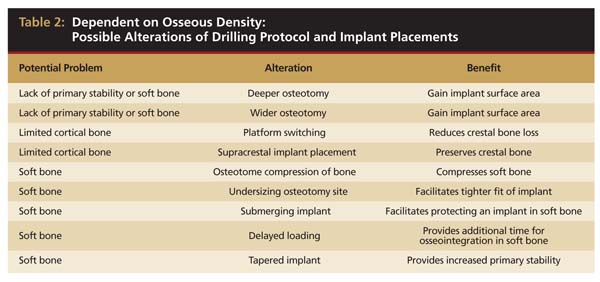
Ultimately, it is the tactile feedback provided by the 2-mm twist drill that allows the clinician to appraise the density of bone for the entire length of the implant to be placed. It is this tactile sensation that verifies assumptions related to the type of bone found in different regions of the mouth and overrides radiographic interpretations (eg, Hounsfield units) regarding bone density. The tactile feedback provided by the twist drill is the critical determinant with respect to identifying bone density. Based on this finding, clinicians should be prepared to alter their drilling protocol and size of implants to be placed (Table 2).
 |
Depth and Width of Osteotomy
The 2-mm twist drill is used to develop an osteotomy to its full depth at the implant site. Whether the drill caused a fenestration of the cortical bony plate should be determined. When this occurs, the twist drill can be redirected into solid bone and the damage can be repaired with a bone graft and a barrier. Recognition that the bone type is softer than expected may dictate drilling deeper or creating a wider osteotomy than planned in order to place a larger implant if bone is available. This will increase the biomechanical strength of the implant and bone contact area to dissipate occlusal forces on the implant. In general, an implant 1 mm wider in diameter will increase the surface area by 20% to 30%.6 To achieve this same gain in surface area with respect to height, an additional 3 mm in length is needed.7
Undersizing the Drilling Sequence
If D3 or D4 bone, in particular, is detected with a 2-mm twist drill, it may be beneficial not to drill the osteotomy to the width usually used with D1 or D2 bone. Instead, the clinician should undersize the drilling sequence (stop osteotomy development one drill size less than what would normally be used with the selected diameter implant). This will result in placing an implant into a smaller osteotomy than what is typically created, thereby increasing the frictional retention of the implant and providing greater primary stability.8 Similarly, another technique to increase stability is to use the last drill only half way down the osteotomy.
Submerging vs Not Submerging an Implant
If an implant is placed in soft bone and there is concern that the native bone may not provide sufficient primary stability when challenged by tongue forces or a bolus of food, it may be advantageous to submerge the implant under the soft tissue to supply it with additional protection during osseointegration.9 Likewise, if the bone is soft and the implant after being fully seated is a “spinner,” it is prudent to submerge the implant during the period of osseointegration.10
If an implant platform is placed at the crest of bone and the implant is submerged under a soft-tissue flap, formation of the biologic width and crestal bone loss will not occur until the healing abutment is attached.11 Therefore, if implant stability is derived from a limited amount of cortical bone, submerging the implant will help retain cortical bone, thereby providing additional primary stability during osseointegration.
Supracrestal vs Subcrestal Implant Placement
With D3 and D4 bone, consideration should be given to placing the implant supracrestally because of limited cortical bone (Figure 4). Pertinently, placement of the implant platform coronal to the crest of bone facilitates formation of the biologic width surpracrestally with no concomitant bone loss vs placement of the implant platform crestally or subcrestally, which results in bone loss and development of a subcrestal biologic width.12,13
Tapered vs Nontapered Implant
Tapered implants often are used if space is inadequate between teeth to accommodate a parallel walled implant or when there is concern that nontapered implants may perforate through the cortical plate of bone. It may also be advantageous to use tapered implants in situations of low density bone (Figure 5). In this regard, the theory is that if a small osteotomy is created, a tapered implant will compress the bone, especially in the coronal region, thereby improving initial stability of the implant.14,15 With respect to the standard Brånemark design, research has demonstrated a 1º taper results in better primary stability.16 In addition, when O’Sullivan et al17 compared five different implant designs with respect to removal of torque and primary stability in cadaver bone, they noted a tapered implant in D4 bone was superior to other implant designs. Others also found higher primary stability values when a tapered implant was compared with standard Brånemark implants.17
Countersinking
Some implants have a wider crestal module than implant body. To accommodate this facet of the implant, if it is to be placed crestally, a crest countersink drill can be used to enlarge the osteotomy in the cortical bone along the crest. However, if it is determined with the twist drill that D3 or D4 bone is present, countersinking should be avoided to retain as much cortical bone as possible to achieve primary stability.18
Platform Switching
The biologic width around dental implants is usually 1.5 mm to 2 mm.19 Therefore, if an implant is placed at the osseous crest and a healing abutment is put at this level, the bone will resorb 1.5 mm to 2 mm to accommodate development of the biologic width. The concept of platform switching denotes use of an abutment that is smaller than the platform of the implant (Figure 6).20 Platform switching facilitates starting to develop part of the biologic width on the implant platform, and this results in less bone loss. Thus, if the amount of cortical bone—or bone in general—is limited, platform switching may be beneficial because it may help preserve cortical bone.21
Immediate Placement of Implants
If it is determined with the twist drill that the bone is D1 or D2, then immediate placement of an implant(s) is reasonable. This is true in the esthetic zone if other factors are optimum (a low smile line, no buccal recession, the presence of buccal plate, thick biotype, and keratinized gingiva). Therefore, as indicated previously, if it is suspected that D3 bone is present, the clinician should consider placing a longer or a wider implant than if D2 bone is there because it will provide additional resistance to displacement. Immediate placement of implants in D4 bone is questionable because the bone often is too soft. However, if there is enough cortical bone to attain primary stability or if osteotomes can be used to condense the bone,22 then immediate implants can be placed. Several authors have reported favorable results in D4 bone.23,24 From a different perspective, if the bone is perceived as soft, then an immediate implant with provisionalization should not be attempted unless primary stability can be achieved with 30 Ncm to 40 Ncm of insertion force.25
When to Load Implants
Tactile feedback with the 2-mm twist drill facilitates decision-making in regard to how long an implant should remain in place for osseointegration before being loaded with a prosthesis. For example, with D1, D2, or D3 bone, an implant with a textured surface can be loaded 2 to 3 months after its placement.26 However, with D4 bone, it may be advantageous to wait 6 months before loading the implant.2 With respect to provisionalization, if there is D1 or D2 bone, immediate placement and provisionalization (out of occlusion) of the implant may be considered.
Number and Position of Implants
Increasing the number of implants can compensate for decreasing weakness of bone.27 A greater number of implants will provide increased functional loading area and reduced stress on bone. For example, in D2 bone, a pontic may be placed between two implants; whereas, in D3 bone, it may be advantageous to place one implant per tooth (Figure 7).28 In less dense bone, cantilevers should be avoided, and if contemplated, consideration should be given to increasing the number and size of the implants.
Angulation
With a 2-mm twist drill in the handpiece, the head of this tool is aimed at the opposite jaw to attain the proper angulation for drilling the osteotomy. The initial development of the osteotomy with the 2-mm drill should be done to a depth of approximately 5 mm, and then a guide pin should be placed to assess osteotomy angulation (Figure 8).29 At this juncture, alterations in angulation can be done with the twist drill. Also, guide pins can be placed into multiple osteotomies to assess parallelism between implants and/or adjacent structures. At this early stage, parallelism should be adjusted as necessary.
When a 2-mm twist drill is used to full depth of the osteotomy (eg, 10 mm), it is difficult to change osteotomy angulation with a twist drill. If a correction is necessary, a side-cutting bur (eg, Lindemann) should be used (Figure 9). Furthermore, if there are doubts as to closeness of the osteotomy to adjacent teeth or vital structures, then a radiograph with a guide pin in place should be obtained.30 Ultimately, the angulation and location of the osteotomy should be consistent with design of the future restoration.31
Other Decisions Based on Bone Density
D1 bone
The final osteotomy may need to be tapped.2 Also, the clinician should use sharp burs to avoid overheating the bone during osteotomy development.30 Plentiful irrigation is needed to avoid such overheating.31
D2 bone
This is most often found in the anterior mandible. In D2 bone, ridge reduction to gain a wider ridge for implant insertion does not result in a weakened stability because the buccal and lingual cortical plates and coarse trabecular bone furnish firm support for an implant.2
D3 bone
This type of bone is easy to negotiate; however, the drill needs to rotate while being pushed into position. In D3 bone, bone spreading is easier to accomplish and facilitates placing a larger diameter implant.2
D4 bone
Consideration is needed for creating the rest of the osteotomy past the 2-mm twist drill with osteotomes to preserve and condense the bone or undersize the drilling sequence.2
Osteotome Sinus Elevation
Initially, a 2-mm twist drill can be employed to come within 1 mm of the subantral floor (Figure 10).32,33 Usually, if the twist drill comes too close to the sinus floor, it provides tactile feedback that the cortical bone under the sinus has been reached. Subsequently, the osteotomy can be enlarged with burs and completed with an osteotome; or after the 2-mm twist drill is used, sequentially larger osteotomes can be employed for the rest of the sinus elevation procedure.32
Conclusion
The 2-mm twist drill can be used as an integral facet of finetuning treatment planning, and the issues that should be considered when using a 2-mm twist drill have been described. Information ascertained from tactile feedback can be helpful in treatment planning.References
1. Misch CE. Bone density: a key determinant for treatment planning. In: Misch CE, ed. Contemporary Implant Dentistry. 3rd ed. St. Louis, MO: Mosby Publishing Inc.; 2008:135.
2. Misch CE. Density of bone: effects on surgical approach and healing. In: Misch CE, ed. Contemporary Implant Dentistry. 3rd ed. St. Louis, MO: Mosby Publishing Inc.; 2008:645-667.
3. Trisi P, Rao W. Bone classification: clinical-histomorphometric comparison. Clin Oral Implants Res. 1999;10(1):1-7.
4. Todisco M, Trisi P. Bone mineral density and bone histomorphometry are statistically related. Int J Oral Maxillofac Implants. 2005;20(6):898-904.
5. Resnik R, Kircos L, Misch CE. Diagnostic images and techniques. In: Misch CE, ed. Contemporary Implant Dentistry. 3rd ed. St. Louis, MO: Mosby Publishing Inc.; 2008:38-67.
6. Curtis DA, Sharma A, Finzen FC, et al. Occlusal considerations for implant restorations in the partially edentulous patient. J Calif Dent Assoc. 2000;28(10):771-779.
7. Misch CE. Available bone and dental implant treatment plans. In: Misch CE, ed. Contemporary Implant Dentistry. 3rd ed. St. Louis, MO: Mosby Publishing Inc.; 2008:181.
8. Turkyilmaz I, Aksoy U, McGlumphy EA. Two alternative surgical techniques for enhancing primary implant stability in the posterior maxilla: a clinical study including bone density, insertion torque, and resonance frequency analysis data. Clin Implant Dent Relat Res. 2008;10(4):231-237.
9. Iezzi G, Degidi MA, Scarano A, et al. Bone Response to submerged, unloaded implants inserted in poor bone sites: a histological and histomorphometrical study of 8 titanium implants retrieved from man. J Oral Implantol. 2005;31(5):225-233.
10. Orenstein IH, Tarnow DP, Morris HF, et al. Factors affecting implant mobile at placement and integration of mobile implants at uncovering. J Periodontol. 1998;69(12):1404-1412.
11. Hermann JS, Buser D, Schenk RK, et al. Crestal bone changes around titanium implants. A histometric evaluation of unloaded non-submerged and submerged implants in the canine mandible. J Periodontol. 2000;71(9):1412-1424.
12. Piattelli A, Vrespa G, Petrone G, et al. Role of the microgap between implant and abutment: a retrospective histologic evaluation in monkeys. J Periodontol. 2003;74(3):346-352.
13. Weber HP, Buser D, Donath K, et al. Comparison of healed tissues adjacent to submerged and non-submerged unloaded titanium dental implants. A histometric study in beagle dogs. Clin Oral Impl Res. 1996;7(1):11-19.
14. O’Sullivan D, Sennerby L, Jagger D, et al. A comparison of two methods of enhancing implant primary stability. Clin Implant Dent Relat Res. 2004;6(1):48-57.
15. Misch CE, Wang HL, Misch CM, et al. Rationale for the application of immediate load in implant dentistry: part II. Implant Dent. 2004;13(4):310-321.
16. O’Sullivan D, Sennerby L, Meredith N. Influence of implant taper on the primary and secondary stability of osseointegrated titanium implants. Clin Oral Implants Res. 2004;15(4):474-480.
17. O’Sullivan D, Sennerby L, Meredith N. Measurements comparing the initial stability of five designs of dental implants: a human cadaver study. Clin Implant Dent Relat Res. 2000;2(2):85-92.
18. Vidyasagar L, Salms G, Apse P, et al. The influence of site preparation (countersinking) on initial dental implant stability. An in vitro study using resonance frequency analysis. Stomatologija, Baltic Dental and Maxillofacial Journal. 2004;6:14-16.
19. Cochran DL, Hermann JS, Schenk RK, et al. Biologic width around titanium implants. A histometric analysis of the implanto-gingival junction around unloaded and loaded nonsubmerged implants in the canine mandible. J Periodontol. 1997;68(2):186-198.
20. Lazzara RJ, Porter SS. Platform switching: a new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent. 2006;26(1):9-17.
21. Hürzeler M, Fickl S, Zuhr O, et al. Peri-implant bone level around implants with platform-switched abutments: preliminary data from a prospective study. J Oral Maxillofac Surg. 2007;65(7 suppl 1):33-39.
22. Fanuscu MI, Chang TL, Akça K. Effect of surgical techniques on primary implant stability and peri-implant bone. J Oral Maxillofac Surg. 2007;65(12):2487-2491.
23. Mayer TM, Hawley CE, Gunsolley JC, et al. The single-tooth implant: a viable alternative for single-tooth replacement. J Periodontol. 2002;73(7):687-693.
24. Bahat O. Brånemark system implants in the posterior maxilla: clinical study of 660 implants followed for 5 to 12 years. Int J Oral Maxillofac Implants. 2000;15(5):646-653.
25. Saadoun AP. Immediate implant placement and temporization in extraction and healing sites. Compend Contin Educ Dent. 2002;23(4):309-318.
26. Fradera AP, Roig EP, Sesma JM, et al. Multicenter retrospective study of implants loaded with functional prostheses 8 weeks after insertion. Implant Dent. 2005;14(1):43-49.
27. Bidez MW, Misch CE. Force transfer in implant dentistry: basic concepts and principles. J Oral Implantol. 1992;18(3):264-274.
28. Misch CE. Density of bone: effects on surgical approach and healing. In: Misch CE, ed. Contemporary Implant Dentistry. 3rd ed. St. Louis, MO: Mosby Inc; 2008:143.
29. Greenstein G, Cavallaro C, Tarnow D. Clinical pearls: things you need to know about surgical implant dentistry. Dentistry Today. In press.
30. Chacon GE, Bower DL, Larsen PE, et al. Heat production by 3 implant drill systems after repeated drilling and sterilization. J Oral Maxillofac Surg. 2006;64(2):265-269.
31. Ercoli C, Funkenbusch PD, Lee HJ, et al. The influence of drill wear on cutting efficiency and heat production during osteotomy preparation for dental implants: a study of drill durability. Int J Oral Maxillofac Implants. 2004;19(3):335-349.
32. Hahn J. Clinical uses of osteotomes. J Oral Implantol. 1999;25(1):23-29.
33. Davarpanah M, Martinez H, Tecucianu JF, et al. The modified osteotome technique. Int J Periodontics Restorative Dent. 2001;21(6):599-607.
About the Authors
Gary Greenstein, DDS, MS
Former Clinical Professor, Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York; Private Practice, Freehold, New Jersey
John Cavallaro, DDS
Former Associate Professor, Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York; Private Practice, Brooklyn, New York
Benjamin Greenstein, DMD
Private Practice, Freehold, New Jersey
Dennis Tarnow, DDS
Former Professor, Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York;
Private Practice, New York, New York