You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Historically, periodontics involved diseases surrounding teeth. The primary goal was to save teeth, and great efforts were made, both surgically and restoratively, to accomplish this. Periodontal surgical tools, such as guided-tissue regeneration1-3 and soft-tissue root coverage grafting,4 evolved to include tissue engineering5,6 and periodontal microsurgery with microscope enhancement.7 Nonsurgical tools also developed and now include subgingival antimicrobial therapy,8,9 subgingival microscopy,10 and host-modulated resistance.11
As the field of periodontics expanded to include dental implants, a paradigm shift occurred because of their long-term predictability12,13 and an emphasis on evidence-based dentistry.14 With dental implants now the legal standard of care for tooth replacement in many states,15 the new goal is to save bone16 not just teeth. The rationale for this is multifactorial. People are living longer; therefore, the longevity of restorative solutions and the amount of bone remaining when those restorations eventually need replacement have become essential factors in treatment planning, as well as preserving bone for esthetic considerations. Further, maintaining teeth with advanced periodontal disease may have deleterious effects on a patient’s long-term health.17 In this youth-orientated society, patients are demanding additive solutions to restorative treatment, such as dental implants,18 vs subtractive solutions involving the preparation of teeth.
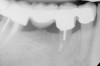
To meet the needs of the new paradigm, treatment techniques have evolved for bone preservation. Figure 1 shows a case in which tooth No. 5 had advanced bone loss and the treatment option was to save it. The patient did not opt to have this treated, however. Figure 2 shows the same area approximately 18 months later when the advanced bone loss was also affecting the adjacent teeth. Traditional treatment—extraction of this tooth—would have led to a significant hard- and soft-tissue defect. Use of the alternative treatment—grafting of the socket at the time of extraction19,20—preserved the hard and soft tissue (Figure 3 and Figure 4). Grafting the socket to minimize postextraction ridge shrinkage is a much more conservative approach than performing ridge augmentation after extraction,21 which would have been required if the socket grafting had not been done in conjunction with the extraction.
This article discusses the changes in treatment planning that are required with the new paradigm of when to save a tooth and when to extract and place an implant.
Main Factors
Numerous factors must be considered in the treatment planning process when cases present with advanced periodontal disease and/or advanced decay. For the purpose of this article, five main factors will be discussed. These factors are the decay rate/endodontic status, status of the adjacent teeth, periodontal status, proximity of critical anatomic structures, and esthetic considerations.
Decay Rate/Endodontic Status
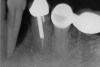
In treatment planning, the decay rate of the patient’s teeth, including the endodontic status of the individual tooth, becomes an important factor when considering long-term outcomes. In the pictured case (Figure 5), tooth No. 11, which previously had been treated endodontically, had recurrent decay and tooth No. 12 had advanced decay with endodontic involvement. In less than 30 days, recurrent decay that reaches the endodontic fill through a leaky restoration (temporary or not), ill-fitting crowns, or broken fillings can re-infect the entire length of the root canal system in a previously endodontically treated tooth.22 Therefore, saving a previously endodontically treated tooth, as in this case, may involve endodontic re-treatment, which can be a deciding factor for tooth preservation.
In addition, xerostomia becomes more likely with advanced patient age and/or the use of certain medications.23 This problem can lead to a higher decay rate, which has implications for a situation similar to the above case. In this case, in which tooth No. 12 would need endodontic treatment, surgical crown lengthening, a post, a crown, etc, to save it, the alternative of extraction and implant placement should be considered. The implant would not be susceptible to future decay, root fracture, or endodontic failure. The fee for this treatment also may be comparable to tooth preservation. If the tooth also requires a post, core, or other treatment, then its prognosis24 would be less optimistic than that of a dental implant. Also, if the implant can be placed at the time of extraction, there would be only one surgical visit; whereas, the endodontic and crown-lengthening procedures usually involve many treatment visits.
Bone removal is also a factor. In this example, tooth No. 12 had a short root. Removal of bone to reestablish a 3-mm biologic width as well as about 2 mm of ferrule25 would decrease the long-term prognosis of the tooth, especially because there would be an existing compromise regarding the crown-to-root ratio.26 Osseous recontouring for crown lengthening also may remove bone from the adjacent teeth (in this example, the distal of tooth No. 11).
Regarding the long-term results of endodontic therapy vs extraction and implant placement, the literature has yielded widely disparate results.27 The endodontic studies have had dissimilarities in criteria for success and failure, and randomized controlled studies comparing single-tooth implants and restored endodontically treated teeth are unavailable.28 The long-term success rate of endodontic treatment is high if the tooth is treated with a well-fitting single-tooth crown with adequate ferrule.29 However, the main causes of loss of endodontically treated teeth are prosthetic failure (59.4%) and periodontal failure (32%), with endodontic failure (compared with prosthetic and periodontal) accounting only for ~ 8.6% of tooth loss.30 Another factor to consider with the option of endodontic treatment is if the tooth in question has an existing periapical radiolucency. Teeth with existing periapical radiolucencies generally have a lower success rate than those without a presenting periapical radiolucency. However, if the radiographic diameter of the periapical lesion is greater than 5 mm, the success rate of treatment significantly decreases.31,32 Also, endodontic re-treatment has a significantly lower success rate, especially if the tooth has a periapical radiolucency.33 Apical surgery has a relatively low success rate (~ 64%) and a lower re-treatment success rate (~ 36%).34 Though the published success rates of endodontic treatment vary, it is clear that endodontic re-treatment is generally less predictable than the initial endodontic treatment and apical surgery has an even lower long-term success rate.24
These rates should be compared with the long-term success rate of dental implants in the treatment planning decision. Though the results vary with implant outcomes as well, the long-term survival rates up to 16 years generally are higher than 95%.35,36 In summary, regarding endodontically treated teeth, the long-term endodontic success rate is high for those teeth with a well-fitting crown with adequate ferrule. However, the failure rate significantly increases when including the restorative and periodontal factors. This is a significant factor when considering treating teeth with large presenting periapical lesions and when contemplating their use as abutments for fixed or removable partial dentures (RPDs), as will be discussed in the next section.
Status of Adjacent Teeth
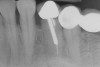
The clinician also must consider the status of the adjacent teeth. Figure 6 shows teeth Nos. 29 and 31 prepared for a fixed bridge. Factors to be considered in this example were the short root of tooth No. 29 with a distal biologic width violation and a short root trunk on tooth No. 31 (which leads to furcation involvement with a small amount of facial or lingual bone loss). This patient also had periodontal disease, which further decreased the long-term prognosis of the fixed bridge option. No prospective studies directly compare the longevity of the two options: a three-unit fixed bridge vs an implant.37 Other factors that complicate comparisons of an implant vs a fixed three-unit bridge are the variability of fixed bridges as well as the variability of the implants (amount of bone, implant length, etc). For example, endodontically treated abutment teeth do not last as long as nonendodontically treated abutment teeth.38 Restorations on teeth with endodontic posts and a minimal length of ferrule do not persist as long as those on teeth without a post and at least a 2-mm ferrule.39
In a meta-analysis, three-unit fixed bridges of all kinds were found to have a success rate of ~ 84% at 60 months,40 while the single-tooth implant success rate was determined to be 95.1% at the same period. During longer study periods, the success rate of implants did not decrease nearly as much as that for fixed bridges. In a meta-analysis of nine studies, the 15-year success rate of fixed partial dentures (FPDs) was found to be about 66%, while a 20-year study of single-tooth implants had a success rate of 91%.41 In addition to the above success rates of fixed bridges, fixed bridges with more than three units have significantly lower long-term success rates than three-unit fixed bridges.42 Also, a FPD does not last as long as either an endodontically treated tooth with a single well-fitting crown or a single implant with one crown.42
In this example, the more predictable option would have been to place an implant in the No. 30 position and restore the area as three single units. However, the treatment delivered involved a four-unit fixed bridge, which then included tooth No. 28. Unfortunately, this bridge failed at approximately 5 years (Figure 7 and Figure 8) because of a root fracture of tooth No. 29 and advanced furcation involvement with residual endodontic infection of tooth No. 30. The inclusion of tooth No. 28 into the bridge also decreased its long-term prognosis because of its preparation.43 The alternative restorative option of a RPD also would decrease the prognosis of the RPD abutment teeth, which fail more often than FPD abutment teeth.43
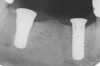
Figure 9 shows the implant placement at the time of extraction and Figure 10 shows the implant-supported fixed bridge. In one surgical procedure, the implants in the Nos. 29 and 31 positions were placed at the time of the extraction of these two teeth. The implants were restored approximately 3 months after placement.
Periodontal Status
The third factor to consider is determining the existing periodontal status of the tooth as well as the overall periodontal status of the dentition. It is beyond the scope of this article to provide an in-depth evaluation of periodontal status. The determinants include pocket depth, age of the patient with the associated amount of clinical attachment loss, smoking status, health factors (eg, diabetes mellitus, stress levels, immunodeficiency disease), furcation status, crown-to-root ration, occlusal factors (eg, clenching, bruxing), type of vertical osseous lesion, mobility, and compliance (eg, oral hygiene, motivation). Tooth position also should be considered. In a very large retrospective study of periodontal maintenance patients (600 patients, with an average of 22 years in maintenance in a single periodontal practice), certain trends were delineated.44 The researchers found maxillary molars were the teeth most often lost, followed by mandibular molars. Also, on average, posterior teeth were lost more frequently than anterior teeth. Retrospectively, this study classified patients in three major groups: well maintained, downhill, and extreme downhill. Most patients (83%) were well maintained with very little tooth loss, demonstrating the effectiveness of periodontal maintenance in a periodontal practice. Few patients, ~ 4%, experienced major tooth loss (extreme downhill). Procedures such as guided-tissue regeneration (GTR) and dental implants were not treatment options in this study, which was published in 1978. Studies have been done to better delineate prognosis, but accurate prognosis of individual teeth with attachment loss remains a challenge.45
When considering the options on a tooth with a significant vertical osseous lesion, the technique of GTR should be considered. As with the endodontic studies, there is significant variability in success rates, as well as high variability in clinician success rates.46 The long-term success rates also are shorter in observation periods than in implant or endodontic studies42 because the practice of GTR is a more recent introduction to the surgical armamentaria. Also, GTR studies are harder to correlate to each other because of the high variability in techniques and materials. Further, their sample sizes are generally smaller compared to those in either endodontic or implant studies. In a recent review article of predictability of clinical outcomes following regenerative therapy in intrabony defects (using GTR), inclusion criteria for minimal time of observation was only 6 months.46 Further, the long-term success rate is determined greatly by patient compliance. In this author’s opinion, the successfully treated areas are probably more susceptible to future bone loss than the adjacent teeth without initial significant vertical osseous lesions.
GTR, however, is still a viable option because there is consistency in published data—treating a vertical osseous lesion with this technique results in more clinical attachment gain than just open-flap debridement without performing GTR.46 The success rate in smokers, however, is significantly lower than in nonsmokers.47 Figure 11 and Figure 12] show a case in which tooth No. 22 had a large distal defect. Figure 13 shows the 6-year re-entry photograph, and Figure 14, the 6-year posttreatment radiograph, demonstrating complete clinical fill of the defect. Factors to consider in GTR include defect size (at least 3 mm to 4 mm), number of defect walls (at least two bony walls, but a three-wall defect is the most predictable to treat; Figure 15 shows a one wall defect, which is not graftable), furcation status (furcations are less predictable to obtain increased clinical attachment levels46), and mobility.48 However, patient compliance is critical in regard to both short-term and long-term success rates with GTR.
Proximity to Critical Structures
Next, the clinician must consider the teeth’s proximity to critical structures. Figure 16 shows a panoramic radiograph of a patient with advanced periodontal disease. As can be seen in this radiograph, the bone loss around the maxillary molars was very close to the maxillary sinuses and the bone loss of the distal and furcal areas of tooth No. 30 was close to the inferior alveolar nerve. This demonstrates an adverse effect of keeping teeth too long. In this case, the bone height in the area of tooth No. 19, where the tooth had been lost years earlier (and no RPD was worn), was significantly more coronal than in the area of tooth No. 30.
Because the new treatment planning paradigm stresses preserving bone for potential future implant placement,16 there are changes to the algorithm of when to extract teeth. Currently, it is recommended to consider extraction if keeping teeth will compromise the bone within 10 mm of critical structures, such as the inferior alveolar nerve or the maxillary sinus (though the various techniques to augment the maxillary sinus are considered generally to be more predictable with less morbidity than is vertical bone augmentation).
Esthetic Considerations
The last major factor to consider is esthetics. In this category, the paradigm of bone preservation is merged with the current high esthetic expectations of patients. Even small changes in recession or loss of papillary height can be deemed an esthetic failure. Therefore, facial flap elevation and bone removal in esthetic areas should be minimized. It is this author’s observation that GTR and crown-lengthening procedures usually lead to more recession than extraction and placement of a dental implant, especially immediately placed implants.
Figure 17 shows a case of advanced recession on the facial of tooth No. 10, which had a periodontal-endodontic lesion. Tooth No. 10 was extracted with an implant placed during the same appointment. As demonstrated in this case (Figure 18 and Figure 19), the facial gingival margin can be moved coronally with immediate implant placement.
Because esthetics is such an important factor in today’s dental treatment, new treatment modalities, such as socket preservation, are being incorporated into everyday practice. Grafting the socket at the time of extraction decreases the postoperative shrinking of the ridge in both the horizontal and vertical dimensions.49 This is especially important in the esthetic zone. It is essential to use materials that are bioabsorbable and do not require a surgical flap because flapping the tissue will lead to more bone resorption and nonresorbable materials lead to less native bone available for the implant. Using materials that are bioabsorbable and do not require a flap, therefore, are optimal.
Summary
Every patient and situation is unique, but guidelines help in the algorithm of whether to perform tooth preservation procedures vs extraction procedures, with the option of implant-supported restoration. The paradigm has shifted the primary treatment planning goal from tooth preservation to bone preservation, especially in the esthetic zone.16 Saving teeth when reasonable is still the objective but long-term outcomes need to be better delineated in the dental literature. With the emphasis on evidence-based dentistry,14 the treatment planning paradigm is changing and success rates for all options should be considered:
- Endodontic treatment with a well-fitting crown with sufficient ferrule has a high long-term success rate.29
- Endodontic re-treatment, especially with a large periapical radiolucency, and apical endodontic surgery both have significantly lower long-term success rates than initial endodontic treatment.31,32
- Preparing teeth for restorations significantly decreases their long-term prognosis.43
- When replacing a failing FPD, the alternative of an implant in the edentulous space has a superior long-term survival rate compared with a replacement FPD42 (also when replacing an existing FPD with a new FPD, the new restoration will probably not last as long as the initial restoration).
- A three-unit FPD lasts longer than one with four or more units, but not as long as the alternative of single-unit restorations on teeth and a single-unit restoration on a dental implant(s).42
- When replacing a failing three-unit FPD, the alternative of an implant-supported crown in the edentulous area and two single crowns on the adjacent natural teeth needs to be discussed with the patient. This treatment option has the best long-term prognosis. Also, potential future prosthetic failure most likely will be a single-unit failure instead of another three-unit failure (fixed denture abutment teeth do not last as long as teeth with single crowns).42
- RPD abutment teeth do not last as long as FPD abutment teeth.43 The option of an RPD is therefore almost always a compromised option.
- GTR yields better clinical attachment levels than open-flap curettage. However, there is a high variability between studies and between clinicians and a much higher failure rate occurs in smokers.46,47
- Endodontically treated abutment teeth do not last as long as nonendodontically treated abutment teeth.38
- Periodontal maintenance works well long term with most patients.44
- Dental implants are the standard of care for tooth replacement in many states because of their high long-term success rate.15
- When contemplating surgical crown lengthening, consideration should be given to not removing bone within 10 mm of critical anatomic structures or from furcations.16
- When a tooth would require surgical crown lengthening with endodontic treatment and associated post, build-up, etc, the alternative of a dental implant should be considered because the fee could be similar for both options. However, the implant option is generally more predictable long term.37
- As esthetic considerations are such an important factor in treatment planning, procedures such as socket grafting at the time of extraction to decrease ridge shrinkage in the esthetic zone should be incorporated into treatment planning.16
Based on these findings, placement of an implant should be considered in the following instances:
- When molar teeth have extensive furcations (deep Class II and all Class III) and GTR is not deemed as a predictable procedure.
- When recurrent decay is present in patients with a high caries rate, especially in those who are older and/or using certain medications, which can lead to xerostomia.
- If attempting to save a tooth with surgical crown lengthening would lead to bone loss within 10 mm of a critical anatomic structure or remove a critical amount of bone from the adjacent tooth, and/or additional endodontic treatment would be required in which the fee could exceed extraction and implant placement (a generally longer-term restorative option).
- When a young patient presents with a high degree of bone loss from periodontitis (demonstrating a high degree of susceptibility to periodontal disease) or has individual teeth with advanced bone loss.
- When patient compliance is poor and/or the patient is a smoker and GTR is an option because dental implants are more resistant to smoking and poor compliance than is the long-term outcome of GTR.
- When endodontic re-treatment has been performed, especially with a residual periapical lesion.
- If saving a tooth would compromise esthetics significantly.
The following is a list of when to consider saving the tooth:
- When endodontic treatment (if necessary) can be performed and the tooth can be sealed with a well-fitting single-tooth restoration with adequate ferrule.
- When the vertical osseous defects can be grafted predictably.
- When the patient is psychologically motivated to keep his or her teeth and has been informed of the various options.
- When the patient has very good compliance and performs good oral hygiene.
References
1. Bowers GM, Reddi AH. Regenerating the periodontium in advanced periodontal disease. J Am Dent Assoc. 1991;122(10):45-48.
2. Sottosanti JS. Calcium sulfate: a biodegradable and biocompatible barrier for guided tissue regeneration. Compend Contin Educ Dent. 1992;13(3):226-234.
3. Anson D. Calcium sulfate: a 4-year observation of its use as a resorbable barrier in guided tissue regeneration of periodontal defects. Compend Contin Educ Dent. 1996;17(9):895-899.
4. Miller PD Jr. Root coverage using a free soft tissue autograft following citric acid application. Part 1: technique. Int J Periodontics Restorative Dent. 1982;2(1):65-70.
5. Camelo M, Nevins ML, Schenk RK, et al. Periodontal regeneration in human class II furcations using purified recombinant human platelet-derived growth factor-BB (rhPDGF-BB) with bone allograft. Int J Periodontics Restorative Dent. 2003;23(3):213-225.
6. Yamada Y, Ueda M, Hibi H, et al. A novel approach to periodontal tissue regeneration with mesenchymal stem cells and platelet-rich plasma using tissue engineering technology: a clinical case report. Int J Periodontics Restorative Dent. 2006;26(4):363-369.
7. Shanelec DA. Periodontal microsurgery. J Esthet Restor Dent. 2003;15(7):402-408.
8. Slots J, Rams TE. Antibiotics in periodontal therapy: advantages and disadvantages. J Clin Periodontol. 1990;17(7 pt 2):479-493.
9. Williams RC, Paquette DW, Offenbacher S, et al. Treatment of periodontitis by local administration of minocycline microspheres: a controlled trial. J Periodontol. 2001;72(11):1535-1544.
10. Stambaugh RV. A clinician’s 3-year experience with perioscopy. Compend Contin Educ Dent. 2002;23(11A):1061-1070.
11. Preshaw PM, Hefti AF, Jepsen S, et al. Subantimicrobial dose doxycycline as adjunctive treatment for periodontitis. A review. J Clin Periodontol. 2004;31(9):697-707.
12. Buser C, Mericske-Stern R, Dula K, et al. Clinical experience with one-stage, non-submerged dental implants. Adv Dent Res. 1999;13:153-161.
13. Ekelund JA, Lindquist LW, Carlsson GE, et al. Implant treatment in the edentulous mandible: a prospective study on Brånemark system implants over more than 20 years. Int J Prosthodont. 2003;16(6):602-608.
14. Bauer J, Spackman S, Chiapelli F, et al. Evidence-based dentistry: a clinician’s perspective. J Calif Dent Assoc. 2006;(7):511-517.
15. Curley AW. Dental implant jurisprudence: avoiding the legal failures. J Calif Dent Assoc. 2001;29(12):847-853.
16. Greenstein G, Cavallaro J, Tarnow D. When to save or extract a tooth in the esthetic zone: a commentary. Compend Contin Educ Dent. 2008;29(3):136-146.
17. Horowitz RA. Advanced periodontal therapy—to save or replace the questionable tooth. Inside Dentistry. 2008;4(1):2-5.
18. Tepper G, Haas R, Mailath G, et al. Representative marketing-oriented study on implants in the Austrian population. II. Implant acceptance, patient-perceived cost and patient satisfaction. Clin Oral Implants Res. 2003;14(5):634-642.
19. Sottosanti JS. Aesthetic extractions with calcium sulfate and the principles of guided tissue regeneration. Pract Periodontics Aesthet Dent. 1993;5(5):61-69.
20. Anson D. Maxillary anterior esthetic extractions with delayed single-stage implant placement. Compend Contin Educ Dent. 2002;23(9):829-848.
21. Iasella JM, Greenwell H, Miller RL, et al. Ridge preservation with freeze-dried bone allograft and a collagen membrane compared to extraction alone for implant site development: a clinical and histologic study in humans. J Periodontol. 2003;74(7):990-999.
22. Torabinejad M, Ung B, Kettering JD. In vitro bacterial penetration of coronally unsealed endodontically treated teeth. J Endod. 1990;16(12):566-569.
23. Kossioni AE, Dontas AS. The stomatognathic system in the elderly. Useful information for the medical practitioner. Clin Interv Aging. 2007;2(4):591-597.
24. Heydecke G, Peters MC. The restoration of endodontically treated, single-rooted teeth with cast or direct posts and cores: a systematic review. J Prosthet Dent. 2002;87(4):380-386.
25. Ichim I, Kuzmanovic DV, Love RM. A finite element analysis of ferrule design on restoration and resistance and distribution of stress within a root. Int Endod J. 2006;39(6):443-452.
26. Bader HI. Treatment planning for implants versus root canal therapy: a contemporary dilemma. Implant Dent. 2002;11(3):217-223.
27. Friedman S, Mor C. The success of endodontic therapy—healing and functionality. J Calif Dent Assoc. 2004;32(6)493-503.
28. Iqbal MK, Dim S. For teeth requiring endodontic treatment, what are the differences in outcomes of restored endodontically treated teeth compared to implant-supported restorations [published erratum appears in: Int J Oral Maxillofac Implants. 2008;23(1):56]. Int J Oral Maxillofac Implants. 2007;22 suppl:96-113.
29. Aquilino SA, Caplan DJ. Relationship between crown placement and the survival of endodontically treated teeth. J Prosthet Dent. 2002;87(3):256-263.
30. Vire DE. Failure of endodontically treated teeth: classification and evaluation. J Endod. 1991;17(7):338-342.
31. Strindberg IZ. The dependence of the results of pulp therapy on certain factors. An analytic study based on the radiographic and clinical follow-up examinations. Acta Odontol Scand. 1956;14(suppl 21):1-174.
32. Sundqvist G, Figdor D, Persson S, et al. Microbiologic analysis of teeth with failed endodontic treatment and the outcome of conservative re-treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85(1):86-93.
33. Friedman S. Treatment outcome and prognosis of endodontic therapy. In: Orstavik D, Pitt Ford TR, eds. Essential Endodontology. Oxford, UK: Blackwell Science; 1998:367-401.
34. Peterson J, Gutmann JL. The outcome of endodontic resurgery: a systematic review. Int Endod J. 2001:34(3):169-175.
35. Lambrecht JT, Filippi A, Kunzel AR, et al. Long-term evaluation of submerged and nonsubmerged ITI solid-screw titanium implants: a 10-year life table analysis of 468 implants. Int J Oral Maxillofac Implants. 2003;18(6):826-834.
36. Wagenberg B, Froum SJ. A retrospective study of 1925 consecutively placed immediate implants from 1988 to 2004. Int J Oral Maxillofac Implants. 2006;21(1):71-80.
37. Salinas TJ, Eckert SE. In patients requiring single-tooth replacement, what are the outcomes of implant as compared to tooth-supported restorations [published erratum appears in: Int J Oral Maxillofac Implants. 2008;23(1):56] Int J Oral Maxillofac Implants. 2007;22(suppl):71-95.
38. De Backer H, Van Maele G, De Moor N, et al. Single-tooth replacement: is a 3-unit fixed partial denture still an option? A 20-year retrospective study. Int J Prosthodont. 2006;19(6):567-573.
39. Mezzomo E, Massa F, Suzuki RM. Fracture resistance of teeth restored with 2 different post-and-core designs fixed with 2 different luting cements: an in vitro study. Part II. Quintessence Int. 2006;37(6):477-484.
40. Scurria MS, Bader JD, Shugars DA. Meta-analysis of fixed partial denture survival: prostheses and abutments. J Prosthet Dent. 1998;79(4):459-464.
41. Lekholm U, Grondahl K, Jemt T. Outcome of oral implant treatment in partially edentulous jaws followed 20 years in clinical function. Clin Implant Dent Relat Res. 2006;8(4):178-186.
42. Torabinejad M, Anderson P, Bader J, et al. Outcomes of root canal treatment and restoration, implant-supported single crowns, fixed partial dentures, and extraction without replacement: a systematic review. J Prosthet Dent. 2007;98(4):285-311.
43. Miyamoto T, Morgano SM, Kumagai T, et al. Treatment history of teeth in relation to the longevity of the teeth and their restorations: outcomes of teeth treated and maintained for 15 years. J Prosthet Dent. 2007;97(3):150-156.
44. Hirschfeld I, Wasserman B. A long-term survey of tooth loss in 600 treated periodontal patients. J Periodontol. 1978;49(5):225-237.
45. Wilson TG Jr. The current status of determining periodontal prognosis. Curr Opin Periodontol. 1993;67-70.
46. Aichelmann-Reidy ME, Reynolds MA. Predictability of clinical outcomes following regenerative therapy in intrabony defects. J Periodontol. 2008;79(3):387-393.
47. Rosenberg ES, Cutler SA. The effect of cigarette smoking on the long-term success of guided tissue regeneration: a preliminary study. Ann R Australas Coll Dent Surg. 1994;12:89-93.
48. Cortellini P, Tonetti MS, Lang NP, et al. The simplified papilla preservation flap in the regenerative treatment of deep intrabony defects: clinical outcomes and postoperative morbidity. J Periodontol. 2001;72(12):1701-1712.
49. Phillips K, Kois JC. Aesthetic peri-implant site development. The restorative connection. Dent Clin North Am. 1998;42(1):57-70.
About the Author
David Anson, DDS, Private Practice, Beverly Hills, California