You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The term "immediate dental implant" denotes that the implant is inserted directly after tooth removal, whereas delayed seating connotes implantation occurring at a future time. The notion of immediate implant placement was introduced in the 1970s, and this technique currently is widely accepted and demonstrates a high implant survival rate.1 Sometimes, however, there may be uncertainty concerning which criteria should be applied to determine whether implants should be inserted immediately or in a delayed manner to a time after tooth removal. In this regard, consideration needs to be given to prosthetic issues (eg, tooth position) and gingival and osseous support of the tooth being extracted. This article addresses how clinicians can achieve predictable, cosmetic implant restorative results in the esthetic zone after tooth removal. Guidelines are presented with respect to choosing either immediate or delayed implant placement based on clinical and radiographic examinations of the patient. The terms "placed," "inserted," "lodged," "implantation," and "installation" are used to signify implant placement.
Background Information
Indications and Contraindications for Immediate Implant Installation
The main benefits of immediate insertions are time savings and fewer surgical procedures and patient visits. When immediate implants can support a fixed provisional, additional benefits include improved case acceptance, the facilitation of ideal esthetics (due to optimal graft containment and papilla support) and the opportunity to avoid other temporary restorative options, such as a removable prosthesis. There are many situations that dictate the possibility of tooth removal and instant implantation if adequate amounts of bone and soft tissue are present, including endodontic failure, caries, removal of a deciduous tooth, deep probing depths due to periodontitis, vertical root fracture, and idiopathic root resorption. Contraindications to placing immediate implants include lack of soft tissue (recession), inadequate height or width of bone, closeness of adjacent teeth, adverse nerve location, failing to achieve implant primary stability, and inability to attain a reasonable restorative position, angulation, or sink depth.
Survival Rates
Implants immediately inserted into fresh extraction sockets or healed ridges have comparable survival rates (meta-analysis results from 10 studies were, respectively, 97.4% and 97.5%).1 Immediately placed and loaded dental implants with provisionals have a 96.4% survival rate.2 Immediate implants placed into infected locations3 or sites with periapical lesions usually have similar survival percentages to implants installed into healthy ridges.4 However, one study indicated a higher failure rate (3 times) when immediate implants are inserted into infected sites (implants lost: 13/481 at infected sites and 3/354 at non-infected sites).5 It should be noted that in the aforementioned articles dealing with pathosis the authors did not describe the extent of bone grafting performed or degree of infections that existed prior to immediate implantation.
Anatomic Dimensions in Esthetic Zone (Gingiva, Bone Teeth)
To facilitate treatment planning in the esthetic zone it is important for clinicians to know the dimensions of the gingiva, the osseous relationship with the overlying soft tissue, and the size of the teeth (Figure 1 and Figure 2) (Table 1).6
Anterior Esthetics: Decision Criteria to Determine Immediate Vs Delayed Placement
Pretreatment diagnostic data needs to be collected and assessed from three perspectives: prosthetic, surgical, and 3D scanning.
Prosthetic Perspective
Prosthetically, there are five diagnostic keys that help predict peri-implant esthetics after a failed tooth is extracted.7 Table 2 indicates that the optimal scenario for attaining a cosmetic result after immediate implantation occurs when the free gingival margin at the extraction site is coronal to the tissue adjacent to the contiguous teeth, the gingival form is flat-scalloped, a thick biotype and square tooth shape are present, and the osseous crest is high.7 The level of the crestal bone is a critical determinant for the gingiva's post-extraction position. Facially, if the osseous crest is ≤3 mm from the gingival margin, there will be minimal gingival recession (<1 mm) after tooth removal.7 If the osseous crest is >3 mm from the gingival margin, increased recession can result.7 This latter situation can be corrected with orthodontic tooth extrusion or bone grafting. Interproximally, if the alveolar crest is ≤5 mm from the contact area, a favorable esthetic papillary result can be obtained.8 However, when the osseous crest is >5 mm from the tip of the papilla, then extrusion or grafting (bone or soft tissue) may be needed to attain predictable papillary height.
Another factor that influences attaining a cosmetic result is a high lip line. Pertinently, 28% of patients have a high smile line and demonstrate midfacial gingiva, and 91% show papillae when smiling.9 If a high smile line exists, then delayed placement may be indicated to ensure that all anatomical considerations have been achieved (eg, ideal gingival contour) prior to implantation. The most important factor that determines timing of implant positioning and predictability of esthetic results is the patient's anatomy.
Surgical Viewpoint
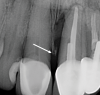
A classification system is needed to describe different clinical scenarios encountered when extracting teeth. Defining socket types is based on periodontal probing, visual evaluations, and radiographic assessments. Elian et al described the following classifications (Figure 3)10: Type I: The bony socket is intact, and the soft-tissue form is undisturbed. Type II: Bone loss is present in the coronal aspect of the socket; the soft tissue remains intact and undisturbed. Type III: Bony defects exist in conjunction with a soft-tissue deformity.
Categorizations of socket type help determine if implants should be placed immediately or delayed. A type I socket can be considered for immediate implant insertion. Types II and III, however, often require delayed implantation and augmentation of soft and or hard tissue before implant installation. To determine the socket type, the clinician can walk the periodontal probe circumferentially around the tooth to detect bone dehiscences. Also, related periapical radiographs may be examined.
After an extraction, subsequent papillary height is dictated by the interproximal bone height on teeth adjacent to the extraction site. It is the supercrestal fibers on contiguous teeth that maintain papillary height adjacent to the extracted site.8 If the osseous crest is <5 mm from the contact area, the papilla will reform; if it is >5 mm, regeneration is unpredictable and probably only 50% of the papilla will regenerate.8 Grunder also demonstrated that papillary height depends on the bone level of the tooth side, not the implant side, of an interdental area (Figure 4).11 Hereported that papillae height adjacent to extraction sites was 4.23 mm when an implant was placed.11 Note that a hopeless tooth should not be considered a useless tooth, because it can be orthodontically extruded and used to help restore ridge anatomy.12
3D Scanning (Radiographic Planning)
Prior to implant placement in the esthetic zone, the morphology of the alveolar ridge must be determined and the local anatomic or pathologic conditions restricting implant insertion evaluated. Panoramic and intraoral radiography is often inadequate to provide this information. Thus, cross-sectional imaging (ie, cone-beam computed tomography [CBCT]) is often recommended to attain the necessary data.13 In this regard, Kan et alclassified sagittal root positions as class I through IV using CBCT imaging (Figure 5).14 They indicated that the class I root position is the most favorable for immediate implant installation, because it has adequate palatal bone for implant positioning and there is enough bone to provide a buccal gap between the buccal plate and the placed implant, thereby reducing buccal plate resorption. A class II sagittal root position is also a candidate for immediate placement, but the anatomy suggests that immediate placement can be challenging. Class III and IV positions are contraindicated for immediate placement. Accordingly, the present authors suggest that a preoperative CBCT be obtained if an immediate placement is to be planned in the esthetic zone.
A concern regarding CBCT scans is radiation exposure for the patient. A CBCT scan submits on average around 130 microsieverts (µSv) to the patient.15 This is equivalent to about 16 days of background radiation.16 A digital full-mouth x-ray series (FMX) using rectangular collimation yields about 38 µSv of radiation.17 A CBCT scan facilitates planning a flapless procedure and helps avoid mistakes with respect to having too little bone required for implant placement. The International Team for Implantology recommends the SAC (straightforward, advanced, and complex) classification for implant cases.18 A CBCT scan helps define these classifications. SAC classifications are as follows: Straightforward: tooth position is clear and involves no soft- or hard-tissue grafting or modification of anatomic structures. Advanced: the proximity of important anatomical structures leads to increased difficulty for implant installation. Complex: tooth position is not clearly identifiable and possibly requires extensive soft- or hard-tissue grafting of the residual alveolar ridge. Candidates for immediate placement fall into the straightforward classification only.
Other Considerations for Surgical/Restorative Treatment Planning
Restorative treatment planning absolutely must precede the surgical plan. In the esthetic zone, screw-retained prosthetics are preferable to facilitate retrievability and avoid the presence of cement in the sulcus around the implant, which is a major contributing factor to peri-implantitis.19 However, buccal plate fenestrations are common when creating an osteotomy for a screw-retained implant (approximately 20% of the time).20 Therefore, if an implant is to be inserted in the cingulum position, a CBCT scan is essential to determine the shape and trajectory of the alveolar ridge. If it appears that the needed osteotomy will result in a buccal plate fenestration, then bone grafting should be done prior to implant seating. If perforation inadvertently occurs while developing an osteotomy, bone grafting should be done at the time of implantation. To avoid buccal bone grafting and maintain a screw-retained option, two choices are available: use of an angulated screw channel abutment, which can alter trajectory by 25 degrees,21 or utilization of a platform-switched implant that has a subcrestal angle correction (off-axis implant placement for anatomical considerations using a co-axis implant).22,23
Critical Criteria for Successful Immediate Implants in the Esthetic Zone
Case Selection: Indications and Contraindications
Considerations for optimal immediate implant placement include: (1) an ideal gingival position (at least 2 mm coronal to the cementoenamel junction [CEJ], or coronal to the adjacent teeth); (2) a type I socket classification; and (3) a class I or II sagittal root position.
Considerations for delayed implant placement are: (1) the gingival position being apical to adjacent teeth; (2) a type II or III socket classification; and (3) a class III or IV sagittal root position.
In some cases with a class III sagittal root position, immediate placement is possible but difficult. It should be noted that a contraindication to extraction, immediate implant placement, and temporization is limited restorative space (eg, cases with a deep bite), because it is difficult to keep the provisional from occluding with the opposing arch during centric occlusion or lateral excursions.
Atraumatic Extraction
In the esthetic zone, it is suggested that teeth be removed and immediate implants installed without elevating a buccal flap to preserve bone and avoid soft-tissue recession. It has been noted that 6 months after tooth removal with flap elevation, extraction sockets manifest a mean 1.24 mm vertical bone loss (range 0.9 mm to 3.6 mm). Usually, there is approximately 3.79 mm horizontal bone decrease (range 2.46 mm to 4.56 mm).24 In contrast, extractions of teeth with no flap elevation demonstrate a reduced amount of horizontal (around 1 mm)25-27 and vertical (around 1 mm) bone loss.28-31 However, studies suggesting there is no difference in the amount of vertical osseous resorption (1 mm) whether procedures are done flapless or with a flap when placing implants did not necessarily address immediate implants.32-35 Bone reduction after flapless extractions may be due to elimination of the blood supply from the periodontal ligament (PDL).10,36 Differences in osseous resorption rates in the aforementioned studies may also be attributed to initial buccal plate thickness (thicker plates resorb less).37
Several different techniques can be used to remove teeth atraumatically. Burs can be used to facilitate easy extractions and avoid buccal-lingual tooth luxation that can damage the buccal plate of bone.38 Pertinently, in maxillary anterior teeth, an 859 diamond can be sunk 10 mm on the mesial and distal of maxillary anterior teeth and run interproximally, with the clinician making sure not to touch the buccal and lingual plates of bone (Figure 6).38 The teeth can then be easily removed with an elevator. After a tooth with a healthy periodontium is removed, it is not necessary to curette the PDL to ensure that the socket fills with bone.39 Similarly, if a tooth with a healthy periodontium is extracted prior to immediate implant placement, the PDL does not need to be removed prior to implant insertion to attain bone fill around a dental implant; however, granulomatous tissue should be removed.39Placing implants too far buccally is an egregious error and must be avoided, because it poses a high risk for a soft-tissue dehiscence. A technique to avoid this is to fabricate a surgical guide and, prior to inserting the implant, place a probe across the contiguous teeth and make sure the implant is placed lingual to the probe leaving enough room for the implant and buccal plate of bone.
Implant Positioning, Angulation, and Depth
For maxillary anterior teeth, an osteotomy is created on the palatal aspect of the socket. It is advisable to use a side cutting drill (eg, Lindemann bur) and create a ledge in the palatal bone two-thirds the distance from the crest of bone to the apex. This ledge is used as a purchase point to place twist drills. It may be useful to enter the bone at an angle with a twist drill and then straighten it up as the osteotomy is created. Ideally, the implant will be positioned so that incisal edges of the mandibular teeth are aiming at the cingulum of the future anterior restoration. Maxillary anterior teeth protrude at about 110 degrees,40 thus the osteotomy must be drilled in a manner that positions the implant to be restored in the desired tooth position. The implant should be kept slightly lingual in the socket and should not touch the buccal plate of bone. The horizontal biologic influence of the implant should be respected to avoid inducing buccal alveolar bone loss.25
Implants should be positioned 1 mm subcrestally as viewed from the labial osseous crest to account for crestal bone resorption. In addition, to avoid an implant being pushed buccally upon insertion, it may be useful to reshape (remove) a small amount of palatal bone of the osteotomy at the crest prior to implantation. For cosmetic reasons, the platforms of immediate implants should be located 3 mm below the buccal gingival margin. This may or may not correlate with being 2 mm to 3 mm below the CEJ of the adjacent teeth if recession occurred.41 When an implant is placed 2 mm to 3 mm below the facial gingival level it is usually several millimeters subcrestal interproximally where the interdental osseous peaks are more coronal than the buccal bone level (Figure 1). Also note that a maxillary canine often tilts distally (around 11 degrees) and the root may be distally dilacerated; therefore, when replacing a maxillary first bicuspid with an implant, the implant should be placed parallel to the maxillary canine to avoid contacting the canine's apex.6
High Implant Stability
Depending on the size of the extracted tooth and the implant to be placed, somewhere along the root surface the implant will usually exceed the diameter of the root and provide mechanical retention. This retention and/or extension of the osteotomy of the implant beyond the apex of the extracted tooth provides primary implant stability. An immediate implant should be positioned at least 3 mm to 5 mm into bone to attain primary stability if mechanical retention cannot be achieved laterally.
An insertion torque of 30 Ncm to 40 Ncm should be attained when installing an implant if an abutment and provisional crown are to be seated (Figure 7 through Figure 16).32 Conversely, if primary stability is achieved with a low insertion torque, the authors recommend that a custom healing abutment be placed without a provisional restoration to avoid excess forces on the implant. Furthermore, without a custom healing abutment in the esthetic zone, the bone graft will not be contained and ideal tissue contours will be lost. For single-tooth restorations, the provisional prosthesis used when 30 Ncm to 40 Ncm is attained should not be in occlusion. If multiple implants are inserted, or the prosthesis turns the corner of the arch or is a full-arch provisional, then functional occlusion can be restored. If a permanent abutment is placed at the time of implant placement and subsequently does not have to be removed, this may help decrease recession, because it avoids disrupting the junctional epithelium that forms on the abutment.42
Fabrication of an Implant Provisional
It takes more time to fabricate a provisional restoration than extract the tooth and seat an implant. A screw-retained provisional is the most ideal temporary restoration (Figure 7 through Figure 16). This involves inserting a polyetheretherketone (PEEK) or titanium temporary abutment. A provisional composite resin or acrylic crown is then positioned on the abutment with respect to adjacent tooth reference points (contact points) and is fixed in the correct position. The gap between the provisional crown and the abutment is filled with the restorative material of choice. In this way the provisional crown and abutment are united to form a single structure. The subgingival portion of the crown should be slightly under-contoured.43 Provisional restorations should be used to act as a bone graft container and may aid in assessing esthetics, phonetics, and occlusal function before delivery of the final implant restorations.44,45 Patient compliance with respect to limiting mastication on a provisional, as well as daily oral hygiene, are important.
Bone Grafting With Respect to the Buccal Gap
"Jumping distance" is a term that refers to the gap between an immediately placed implant and the adjacent alveolar ridge and the bone's ability to bridge the gap.46 If the gap is <2 mm, it will usually fill with bone without the need for bone grafting.47-49 Some research has suggested that an even greater distance can heal without any osseous augmentation.50,51 Various materials can be used to fill the buccal gap, including xenograft or allograft bone substitute52; no ideal material has been identified.
Conclusion
Utilizing preoperative assessments from a prosthetic, surgical, and 3D perspective provides important information to aid clinicians in decision-making with respect to either delayed or immediate implant placement. Insertion of immediate implants is a predictable procedure, with attention to detail necessary to attain success. When placing an immediate implant in the esthetic zone, clinicians need to decide based on insertion torque values whether to utilize a custom healing abutment to maintain gingival contour and retain bone graft material or a fixed immediate provisional that preserves gingival contour, holds the bone graft material, and provides an esthetic restoration.
About the Authors
Joseph Carpentieri, DDS
Assistant Clinical Professor, Department of Prosthodontics, College of Dental Medicine, Columbia University, New York, New York; Private Practice, Surgical Implantology and Prosthodontics, White Plains, New York
Gary Greenstein, DDS, MS
Former Clinical Professor, Department of Periodontology, College of Dental Medicine, Columbia University, New York, New York; Private Practice, Surgical Implantology and Periodontics, Freehold, New Jersey
Queries to the author regarding this course may be submitted to authorqueries@broadcastmed.com.
References
1. Patel R, Ucer C, Wright S, Khan RS. Differences in dental implant survival between immediate vs. delayed placement: a systematic review and meta-analysis. Dent J (Basel). 2023;11(9):218.
2. Del Fabbro M, Testori T, Francetti L, et al. Systematic review of survival rates for immediately loaded dental implants. Int J Periodontics Restorative Dent. 2006;26(3):249-263.
3. Waasdorp JA, Evian CI, Mandracchia M. Immediate placement of implants into infected sites: a systematic review of the literature. J Periodontol. 2010;81(6):801-808.
4. Kaur J, Chahal GS, Grover V, et al. Immediate implant placement in periodontally infected sites - a systematic review and meta-analysis. J Int Acad Periodontol. 2021;23(2):115-137.
5. de Oliveira-Neto OB, Lemos CA, Barbosa FT, et al. Immediate dental implants placed into infected sites present a higher risk of failure than immediate dental implants placed into non-infected sites: systematic review and meta-analysis. Med Oral Patol Oral Cir Bucal. 2019;24(4):e518-e528.
6. Greenstein G, Cavallaro J, Tarnow D. Dental implantology: numbers clinicians need to know. Compend Contin Educ Dent. 2019;40(5):e1-e26.
7. Kois JC. Predictable single-tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent. 2004;25(11):895-907.
8. Choquet V, Hermans M, Adriaenssens P, et al. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001;72(10):1364-1371.
9. Hochman MN, Chu SJ, Tarnow DP. Maxillary anterior papilla display during smiling: a clinical study of the interdental smile line. Int J Periodontics Restorative Dent. 2012;32(4):375-383.
10. Elian N, Cho SC, Froum S, et al. A simplifed socket classification and repair technique. Pract Proced Aesthet Dent. 2007;19(2):99-104.
11. Grunder U. Stability of the mucosal topography around single-tooth implants and adjacent teeth: 1-year results. Int J Periodontics Restorative Dent. 2000;20(1):11-17.
12. Paolone MG, Kaitsas R. Orthodontic-periodontal interactions: orthodontic extrusion in interdisciplinary regenerative treatments. Int Orthod. 2018;16(2):217-245.
13. Tyndall DA, Price JB, Tetradis S, et al; American Academy of Oral and Maxillofacial Radiology. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113(6):817-826.
14. Kan JY, Roe P, Rungcharassaeng K, et al. Classification of sagittal root position in relation to the anterior maxillary osseous housing for immediate implant placement: a cone beam computed tomography study. Int J Oral Maxillofac Implants. 2011;26(4):873-876.
15. Ludlow JB, Davies-Ludlow LE, White SC. Patient risk related to common dental radiographic examinations: the impact of 2007 International Commission on Radiologic Protection recommendations regarding dose calculation. J Am Dent Assoc. 2008;139(9):1237-1243.
16. National Council on Radiation Protection and Measurements. Radiation Protection in Dentistry: Recommendations of the National Council on Radiation Protection and Measurements. Bethesda, MD: NCRP; NCRP Report No. 145; 2003.
17. Health Physics Society. Price JB. Answer to question #10779 submitted to "ask the experts." https://hps.org/publicinformation/ate/q10779.html#:~:text=A%20digital%20FMX%20(full%2Dmouth,collimation%20yields%20about%20388%20%C2%B5Sv. Accessed June 2, 2024.
18. Correia A, Rebolo A, Azevedo L, et al. SAC Assessment Tool in implant dentistry: evaluation of the agreement level between users. Int J Oral Maxillofac Implants. 2020;35(5):990-994.
19. Quaranta A, Lim ZW, Tang J, et al. The impact of residual subgingival cement on biological complications around dental implants: a systematic review. Implant Dent. 2017;26(3):465-474.
20. Chan HL, Garaicoa-Pazmino C, Suarez F, et al. Incidence of implant buccal plate fenestration in the esthetic zone: a cone beam computed tomography study. Int J Oral Maxillofac Implants. 2014;29(1):171-177.
21. Hussien AN, Rayyan MM, Sayed NM, et al. Effect of screw-access channels on the fracture resistance of 3 types of ceramic implant-supported crowns. J Prosthet Dent. 2016;116(2):214-220.
22. Chu SJ, Östman PO, Nicolopoulos C, et al. Prospective multicenter clinical cohort study of a novel macro hybrid implant in maxillary anterior postextraction sockets: 1-year results. Int J Periodontics Restorative Dent. 2018;38(suppl):s17-s27.
23. Egbert N, Ahuja S, Selecman A, Wicks R. Angulated implants for fabrication of implant supported fixed partial denture in the maxilla. J Dent (Shiraz). 2017;18(4):304-313.
24. Tan WL, Wong TL, Wong MC, Lang NP. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin Oral Implants Res. 2012;23(suppl 5):1-21.
25. Vera C, De Kok IJ, Chen W, et al. Evaluation of post implant buccal bone resorption using cone beam computed tomography: a clinical pilot study. Int J Oral Maxillofac Implants. 2012;27(5):1249-1257.
26. Degidi M, Daprile G, Nardi D, Piattelli A. Buccal bone plate in immediately placed and restored implant with Bio-Oss® collagen graft: a 1-year follow-up study. Clin Oral Implants Res. 2013;24(11):1201-1205.
27. Brownfield LA, Weltman RL. Ridge preservation with or without an osteoinductive allograft: a clinical, radiographic, micro-computed tomography, and histologic study evaluating dimensional changes and new bone formation of the alveolar ridge. J Periodontol. 2012;83(5):581-589.
28. Job S, Bhat V, Naidu EM. In vivo evaluation of crestal bone heights following implant placement with ‘flapless' and ‘with-flap' techniques in sites of immediately loaded implants. Indian J Dent Res. 2008;19(4):320-325.
29. Fickl S, Zuhr O, Wachtel H, et al. Tissue alterations after tooth extraction with and without surgical trauma: a volumetric study in the beagle dog. J Clin Periodontol. 2008;35(4):356-363.
30. Barros RRM, Novaes AB Jr, Papalexiou V. Buccal bone remodeling after immediate implantation with a flap or flapless approach: a pilot study in dogs. Titanium. 2009;1:45-51.
31. Blanco J, Nuñez V, Aracil L, et al. Ridge alterations following immediate implant placement in the dog: flap versus flapless surgery. J Clin Periodontol. 2008;35(7):640-648.
32. Maló P, Nobre M. Flap vs. flapless surgical techniques at immediate implant function in predominantly soft bone for rehabilitation of partial edentulism: a prospective cohort study with follow-up of 1 year. Eur J Oral Implantol. 2008;1(4):293-304.
33. De Bruyn H, Atashkadeh M, Cosyn J, van de Velde T. Clinical outcome and bone preservation of single TiUnite™ implants installed with flapless or flap surgery. Clin Implant Dent Relat Res. 2011;13(3):175-183.
34. Caneva M, Botticelli D, Salata LA, et al. Flap vs. "flapless" surgical approach at immediate implants: a histomorphometric study in dogs. Clin Oral Implants Res. 2010;21(12):1314-1319.
35. Araújo MG, Lindhe J. Ridge alterations following tooth extraction with and without flap elevation: an experimental study in the dog. Clin Oral Implants Res. 2009;20(6):545-549.
36. Balli G, Ioannou A, Powell CA, et al. Ridge preservation procedures after tooth extractions: a systematic review. Int J Dent. 2018;2018:8546568.
37. Ferrus J, Cecchinato D, Pjetursson EB, et al. Factors influencing ridge alterations following immediate implant placement into extraction sockets. Clin Oral Implants Res. 2010;21(1):22-29.
38. Cavallaro J, Greenstein B, Greenstein G. Extracting teeth in preparation for dental implants. Dent Today. 2014;33(10):92-100.
39. Botticelli D, Berglundh T, Lindhe J. Resolution of bone defects of varying dimension and configuration in the marginal portion of the peri-implant bone. An experimental study in the dog. J Clin Periodontol. 2004;31(4):309-317.
40. Sangcharearn Y, Ho C. Maxillary incisor angulation and its effect on molar relationships. Angle Orthod. 2007;77(2):221-225.
41. Sorni-Bröker M, Peñarrocha-Diago M, Peñarrocha-Diago M. Factors that influence the position of the peri-implant soft tissues: a review. Med Oral Pathol Oral Cir Bucal. 2009;14(9):e475-e479.
42. Abrahamsson I, Zitzmann NU, Berglundh T, et al. The mucosal attachment to titanium implants with different surface characteristics: an experimental study in dogs. J Clin Periodontol. 2002;29(5):448-455.
43. Levin BP, Wilk BL. Immediate provisionalization of immediate implants in the esthetic zone: a prospective case series evaluating implant survival, esthetics, and bone maintenance. Compend Contin Educ Dent. 2013;34(5):352-361.
44. Tarnow DP, Chu SJ, Salama MA, et al. Flapless postextraction socket implant placement in the esthetic zone: part 1. The effect of bone grafting and/or provisional restoration on facial-palatal ridge dimensional change - a retrospective cohort study. Int J Periodontics Restorative Dent. 2014;34(3):323-331.
45. Chu SJ, Salama MA, Garber DA, et al. Flapless postextraction socket implant placement, part 2: the effects of bone grafting and provisional restoration on peri-implant soft tissue height and thickness - a retrospective study. Int J Periodontics Restorative Dent. 2015;35(6):803-809.
46. Botticelli D, Berglundh T, Buser D, Lindhe J. The jumping distance revisited: an experimental study in the dog. Clin Oral Implants Res. 2003; 14(1):35-42.
47. Caneva M, Salata LA, de Souza SS, et al. Hard tissue formation adjacent to implants of various size and configuration immediately placed into extraction sockets: an experimental study in dogs. Clin Oral Implants Res. 2010;21(9):885-890.
48. Covani U, Cornelini R, Barone A. Bucco-lingual bone remodeling around implants placed into immediate extraction sockets: a case series. J Periodontol. 2003;74(2):268-273.
49. Botticelli D, Berglundh T, Persson LG, Lindhe J. Bone regeneration at implants with turned or rough surfaces in self-contained defects. An experimental study in the dog. J Clin Periodontol. 2005;32(5):448-455.
50. Botticelli D, Berglundh T, Lindhe J. Hard-tissue alterations following immediate implant placement in extraction sites. J Clin Periodontol. 2004;31(10):820-828.
51. Tarnow DP, Chu SJ. Human histologic verification of osseointegration of an immediate implant placed into a fresh extraction socket with excessive gap distance without primary flap closure, graft, or membrane: a case report. Int J Periodontics Restorative Dent. 2011;31(5):515-521.
52. Greenstein G, Cavallaro J. Managing the buccal gap and plate of bone: immediate dental implant placement. Dent Today. 2013;32(3):70-77.