You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Prognosis data assesses the likelihood of success following endodontic treatment and is frequently the main patient concern during treatment planning conversations. Clinicians must understand, though, that prognosis is not a static number and can be heavily influenced by factors both within and outside of their control. To accurately assess the likelihood of success, dental practitioners must be able to identify patient-, tooth-, and treatment-related factors that may affect treatment outcomes.
Clinicians can gain an understanding of both treatment predictability and the impact of prognostic factors through outcome studies. Nonetheless, reported success rates vary among outcome studies due to differences in various parameters, including the way each study defines success, the length of follow-up period, and inter-operator and inter-evaluator variability. This article aims to present an up-to-date analysis of endodontic outcome studies with standardized success criteria and will cover outcomes in nonsurgical root canal therapy (NSRCT), nonsurgical retreatment (RETX), and surgical retreatment (SRETX). Having an understanding of prognosis and the factors that impact prognosis can allow clinicians to better predict the success of proposed treatments to maximize patient outcomes.
Nonsurgical Root Canal Therapy
The endodontic literature is replete with studies commenting on critical determinants that wield significant influence on the success of NSRCT. Since Ng et al's systematic review publications more than a decade ago,1,2 ongoing advancements in research and clinical practice have further enhanced clinicians' understanding of the factors that influence the outcomes of NSRCT. According to a recent outcome study by Chang et al, the overall rate of tooth retention after NSRCT was 96.1%.3 As previously alluded to, this reported retention rate does not reflect a static number. The prognosis literature is clear that preoperative and treatment-related factors can dramatically impact outcomes following care.
Preoperative Factors
Preoperative factors that can impact outcomes following NSRCT can be both patient-related and tooth-related. Patient-related factors include race and systemic health. In a retrospective study, demographic variables such as age, gender, and socioeconomic status were also considered, with only race being associated with adverse outcomes. A multiple regression model revealed a heightened likelihood of adverse consequences arising from endodontic procedures among Black and non-Black minority ethnic patients when compared to their white counterparts.4
Systemic disease states have a demonstrable impact on outcomes. Both diabetes mellitus and hypertension may increase the likelihood of developing endodontic pathology and can also impact healing following treatment. These two conditions may promote endodontic pathology by modulating immune responses and reducing resistance to bacterial infections. Individuals with type 2 diabetes mellitus (T2DM) have a notable association with an elevated risk of developing apical periodontitis (AP).5,6 In cases where individuals with T2DM have preoperative periapical lesions, success for NSRCT decreases by 10% to 20% over a follow-up period of 2 years or more.7 Another study on systemic diseases suggested that diabetes mellitus and hypertension independently elevate the risk of tooth extraction following NSRCT.8 Interestingly, a recent study showed that diabetes mellitus changes the structural makeup of tooth roots, which may predispose the tooth to failure by vertical root fracture.9
It was previously postulated that human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) could influence host response to bacterial infections. However, there is no statistically significant difference in success rates between patients with HIV/AIDS and those without.10 On the other hand, patients with an allergy to amoxicillin have a higher chance of losing teeth after NSRCT.3 Although further investigation is needed to confirm this relationship, it is proposed that patients with multiple drug hypersensitivity have an increased prevalence of proinflammatory cytokines.
Not only do disease states modulate outcomes after NSRCT, so do patient habits. There is a statistically significant association between smoking and AP.11 The study underscores smoking as a preoperative risk factor for NSRCT, potentially diminishing the success of the treatment by elevating the occurrence of periapical lesions and impairing tissue healing.3,11
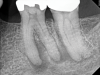
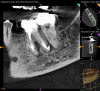
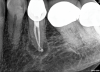
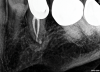
Just as systemic conditions and patient habits impact outcomes after NSRCT, the local dental environment and dental disease states also impact outcomes (Figure 1 through Figure 5). In the Toronto study evaluating 4- to 6-year outcomes following NSRCT, the presence of a periapical radiolucency emerged as a key prognostic factor, substantially reducing the success rate by a factor of four.12 Single-rooted teeth experienced better outcomes compared to multirooted teeth in the presence of periapical lesions.1 Teeth diagnosed preoperatively with irreversible pulpitis or necrosis, in the absence of AP, showed a more favorable prognosis compared to those with preoperative AP.2
Treatment-Related Factors
Treatment-related factors that may impact outcomes following endodontic treatment are entirely under clinician control, and include both endodontic and restorative treatment decisions. Several endodontic factors have been demonstrated to impact outcomes, including access preparations, complete disinfection and obturation, and material selection. The size of the access preparation is inversely related to treatment outcomes, with larger accesses associated with poorer outcomes. Post-endodontic tooth fractures are associated with large endodontic access preparations. A more conservative access design that allows more dentin to remain increases fracture resistance.13 Achieving the proper balance between a conservative access preparation and the thorough identification of all canals is crucial for success.
Positive outcomes in endodontics are predicated on complete cleaning and disinfection of the root canal system, followed by adequate obturation. Irrigants are essential for complete disinfection in NSRCT, and sodium hypochlorite (NaOCl) has proven highly effective by irreversibly oxidizing sulfhydryl groups of essential bacterial enzymes.14 Research demonstrates 40% to 60% of canals irrigated with NaOCl exhibit no detectable cultivable bacteria. Even with effective microbial disinfection, however, if infected pulp tissue remains at the apex, apical pathology will remain persistent.14 As endodontic obturation material sits within the cleaned and shaped space, it can be assumed that obturation is often a reflection of the quality of disinfection. This is shown in the prognosis literature in that both overfilling and underfilling of the canal spaces are associated with less predictable NSRCT, with over-extension of obturation material associated with the lowest success rates.1
In primary NSRCT, different obturation materials may yield varying prognoses. More historic materials, including Resilon and silver points, have been shown to negatively impact outcomes and, therefore, have been removed from the marketplace.15 Gutta-percha with appropriate sealers remains the first and optimal choice for obturation. Sealer predictability appears consistent across types, as clinical studies have shown that the type of sealer utilized is not a strong prognostic factor.16 What matters most is the homogeneity of root canal filling; dense and homogenous fillings have a better prognosis than fillings with voids.16
Not only do treatment decisions during NSRCT impact outcomes, but restorative care following treatment has been closely tied to endodontic prognosis. Both the timing and type of restoration matters with respect to outcomes. The success of NSRCT is closely linked to the timely placement of a definitive restoration. Eighty-five percent (85%) of failed NSRCT cases were attributed to incomplete restoration,17 and teeth restored beyond 4 months post-NSRCT had a threefold increased risk of extraction when compared to those restored within the first 4 months.18 Posterior teeth restored with indirect, full-coverage restorations exhibited higher survival rates than those restored with direct restorations.19 This is true for both premolar and molar teeth, as success rates of premolars restored with crowns (95%) were higher compared to those restored with composite resins (77%).20 Anterior teeth with sufficient tooth structure can be predictably restored with indirect restorations.21
Post placement in endodontically treated teeth is associated with increased risks and challenges. Generally, teeth restored with posts exhibit a higher likelihood of extraction compared to those without posts.22 The type of post used also plays a significant role, as threaded, tapered posts may elevate the risk of tooth fracture by 20 times when compared to threaded, parallel posts.22 Additionally, teeth restored with posts face an augmented risk of failure when utilized as abutments for either fixed or removable partial dentures.22 The critical factor in these scenarios is the amount of remaining tooth structure, as preservation of tooth structure becomes pivotal in determining the success and longevity of the dental restorations.22
Nonsurgical Retreatment
Historically, RETX was considered only a marginally predictable treatment option. Improvements in armamentarium and technique, however, have increased the predictability of RETX, which is currently associated with success rates comparable to those of NSRCT. With traditional techniques, the success rate of retreatment was reported at 82%, while recent studies incorporating modern RETX techniques, including the use of microscope magnification and ultrasonic instruments, indicate that success rates are 90.4%.3,23,24
Just as for NSRCT, several preoperative conditions have been linked to RETX outcomes. These factors include the presence of AP and pre-existing perforations, which can reduce success rate by 12% and 30%, respectively.25 The extent of preoperative swelling, sinus tract formation, pain, and radiographic size of AP are also associated with less predictable outcomes and reduced predictability of surgical retreatment.25
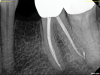
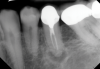
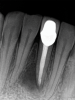
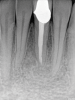
The quality of the initial NSRCT is inversely associated with RETX outcomes, with poorer quality initial treatment tied to more predictable retreatment (Figure 6 through Figure 8).23 Inadequate quality of the initial NSRCT (eg, untreated anatomy, under-instrumentation, ledged and underfilled canals, and overextended obturation) was associated with greater predictability following RETX. However, if clinicians cannot identify and correct the mistakes made in the previous root canal therapy, it becomes more challenging to improve treatment outcomes.23
The advent of cone-beam computed tomography (CBCT) imaging in endodontic diagnosis and treatment planning has allowed clinicians to more accurately diagnose and locate pathology. Brochado Martins and colleagues discussed the concept of selective retreatment, which involves treating only the roots with recurrent or persistent pathology. After evaluating 75 teeth with more than 12 months of follow-up, they demonstrated promising results, with a success rate of 92.6% for the retreated roots and an overall success rate per tooth of 86.7%.26 Only 3.5% of the unretreated roots developed AP postoperatively.26 While selective retreatment could be a reliable treatment option, further clinical trials with larger sample sizes and longer follow-up periods are needed to confirm the efficacy of this treatment method.26
Surgical Retreatment
Surgical retreatment (SRETX), also known as apical microsurgery or apicoectomy, represents an additional treatment modality to manage recurrent or persistent AP. Like NSRCT and RETX, SRETX outcomes are affected by both preoperative and treatment-related factors. These preoperative factors include both patient- and tooth-related considerations. Most studies that assess the impact of a patient's age and sex on periapical healing following surgical retreatment have been inconclusive.25 One publication found a 10% higher 1-year periapical healing rate in patients younger than age 45 years compared to older patients.27 However, the healing rate at a 5-year follow-up showed no significant difference between the two age groups. Ng and Gulabivala in 2023 proposed that younger patients may be able to heal more rapidly, but over a longer follow-up period the differences dissipate.25 Similarly, studies that tried to evaluate the impact of tobacco smoking on postsurgical periapical healing were unable to draw definitive conclusions. One study found that the 10- to 13-year failure rate of SRETX was higher in individuals who smoke, while another found that smoking did not influence periapical wound healing.28
In general, anterior and maxillary teeth are associated with higher success rates when compared, respectively, to posterior and mandibular teeth.25 This may be attributed to the fact that maxillary anterior teeth provide easier surgical access. The only exceptions are maxillary lateral incisors, which tend to have higher failure rates than other teeth because of their tendency to exhibit palatal curvature at their apex, thus increasing the likelihood of palatal cortical plate perforation during surgery.25 Higher failure rates are also observed in teeth that have an isthmus, or communication, between two canals, which is commonly seen in molars.29 Over-retropreparation of the isthmus may weaken the apex and lead to vertical root fracture.29
In addition to preoperative factors, treatment-related factors are tied to prognosis following SRETX. Traditional surgical techniques have a reduced prognosis compared to modern microsurgery techniques (59% vs 94%). Modern techniques allow for greater precision and include the use of a microsurgical instrument along with a surgical operating microscope for magnification and illumination.30,31 Under magnification, anatomical details of a resected apex surface can be easily visualized, including isthmuses, canal fins, microfractures, and lateral canals (Figure 9 and Figure 10).30,31 Furthermore, under microscopy, access to the apex requires less apical bone removal, facilitating the development of smaller bony crypts. Decreased crypt size is associated with faster healing.25 Ultrasonic instruments aid in the creation of parallel, deep preparations with a shallow bevel and precise apical fillings that improve the prognosis of SRETX.30,31
The choice of retrofilling material also impacts outcomes, with bioceramic materials being associated with markedly greater predictability than amalgam or super EBA (ethoxy benzoic acid).25 If hemostatic materials are used during treatment, research suggests that the choice of hemostatic agent does not significantly influence periapical healing.32
A study revealed a distinct correlation between buccal bone plate height and healing success. Teeth with a buccal bone plate height exceeding 3 mm exhibited on average a 94.3% success rate in contrast to those with a height less than 3 mm, which achieved only a 68.8% success rate after 1 year.33 Consequently, clinicians need to focus on preserving the buccal cortical bone surrounding the crypt during the enucleation of periapical lesions, prioritizing this over the root surface for improved outcomes.
Guided tissue regeneration (GTR) has found extensive use in periodontal treatments and has been proposed for use in addressing specific endodontic concerns, notably in cases of "through and through lesions" where both buccal and palatal cortical plates are absent in the periapical area. Despite GTR's promise, current randomized controlled trials present conflicting conclusions regarding its efficacy in apical surgery.34
Clinicians should be cognizant of postoperative indicators that may impact outcomes following SRETX. The presence of blood or serum exudate under the flap does not compromise periapical healing, while conversely, a reduction in tenderness to percussion of the treated tooth is correlated with enhanced periapical healing.25 Timely suture removal is pivotal in ensuring the most favorable outcome in wound healing with minimal suture tract infection. The secure bonding of the flap to the underlying tissues has emerged as the most reliable predictor of optimal wound strength, reaching its peak at around 7 days postoperatively before plateauing.25 Outcome studies have revealed that the quality of coronal restoration is equally as important for surgical postoperative management as it is in NSRCT.25 Coronal restoration improves periapical healing outcomes by maintaining the integrity of the tooth and preventing any leakage that may lead to intraradicular infection.
Summary of Study Outcomes
In this article, numerous prognostic factors have been defined that impact outcomes for the three endodontic treatment modalities described: primary NSRCT, nonsurgical retreatment, and surgical retreatment. A summary of significant study outcomes for prognostic factors of these treatment modalities is provided in Table 1.
Conclusion
With advancements in technology and a deeper understanding of prognostic factors that can impact the outcomes following endodontic treatments, success rates are steadily rising. A 2024 retrospective study revealed promising tooth retention rates following various procedures: 96.2% for NSRCT, 92.4% for RETX, and 97.8% for SRETX.3 Nonetheless, there persists a professional commitment to further explore strategies aimed at mitigating risk factors, whether through rigorous scientific inquiry or the enhancement of clinical skills. Ultimately, best practices dictate that treatment plans should be tailored to individual patients based on their unique presentation and the clinician's understanding of the significant and impactful prognostic factors.
About the Authors
Min Son, DMD Candidate
Harvard School of Dental Medicine, Boston, Massachusetts
Yen Dinh, DMD Candidate
Harvard School of Dental Medicine, Boston, Massachusetts
Bart Voto, DMD Candidate
Harvard School of Dental Medicine, Boston, Massachusetts
Rebekah Lucier Pryles, DMD, Certificate in Endodontics
Assistant Clinical Professor, Department of Endodontics, Tufts University School of Dental Medicine, Boston, Massachusetts; Lecturer, Department of Restorative Dentistry and Biomaterials Science, Harvard School of Dental Medicine, Boston,Massachusetts; Private Practice limited to Endodontics, White River Junction, Vermont
Brooke Blicher, DMD, Certificate in Endodontics
Assistant Clinical Professor, Department of Endodontics, Tufts University School of Dental Medicine, Boston, Massachusetts; Lecturer, Department of Restorative Dentistry and Biomaterials Science, Harvard School of Dental Medicine, Boston,Massachusetts; Private Practice limited to Endodontics, White River Junction, Vermont
Queries to the author regarding this course may be submitted to hauthorqueries@broadcastmed.com.
References
1. Ng YL, Mann V, Gulabivala K. Outcome of secondary root canal treatment: a systematic review of the literature. Int Endod J. 2008;41(12):1026-1046.
2. Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: Part 1: periapical health: Outcome of nonsurgical root canal treatment. Int Endod J. 2011;44(7):583-609.
3. Chang Y, Choi M, Wang YB, et al. Risk factors associated with the survival of endodontically treated teeth: a retrospective chart review. J Am Dent Assoc. 2024;155(1):39-47.
4. Patel N, Scambler S, Ranjbari M, et al. The influence of patient race on the outcome of endodontic treatments: a pooled analysis of one-year recall data from four cone beam computed tomography outcome studies. Br Dent J. 2022 Dec 13. doi: 10.1038/s41415-022-5335-y.
5. Segura‐Egea JJ, Jiménez‐Pinzón A, Ríos‐Santos JV, et al. High prevalence of apical periodontitis amongst type 2 diabetic patients. Int Endod J. 2005;38(8):564-569.
6. López-López J, Jané-Salas E, Estrugo-Devesa A, et al. Periapical and endodontic status of type 2 diabetic patients in Catalonia, Spain: a cross-sectional study. J Endod. 2011;37(5):598-601.
7. Fouad AF, Burleson J. The effect of diabetes mellitus on endodontic treatment outcome: data from an electronic patient record. J Am Dent Assoc. 2003;134(1):43-51.
8. Wang CH, Chueh LH, Chen SC, et al. Impact of diabetes mellitus, hypertension, and coronary artery disease on tooth extraction after nonsurgical endodontic treatment. J Endod. 2011;37(1):1-5.
9. PradeepKumar AR, JothiLatha S, Durvasulu A, et al. Impact of type 2 diabetes mellitus on the occurrence of vertical root fracture: a case control study. J Endod. 2024;50(4):450-455.e1.
10. Quesnell BT, Alves M, Hawkinson RW Jr, et al. The effect of human immunodeficiency virus on endodontic treatment outcome. J Endod. 2005;31(9):633-636.
11. Cabanillas-Balsera D, Segura-Egea JJ, Jiménez-Sánchez MC, et al. Cigarette smoking and root filled teeth extraction: systematic review and meta-analysis. J Clin Med. 2020;9(10):3179.
12. Friedman S, Abitbol S, Lawrence HP. Treatment outcome in endodontics: the Toronto study. Phase 1: initial treatment. J Endod. 2003;29(12):787-793.
13. Kishen A. Mechanisms and risk factors for fracture predilection in endodontically treated teeth. Endod Topics. 2006;13(1):57-83.
14. Sjögren U, Hägglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endod. 1990;16(10):498-504.
15. Use of silver points. American Association of Endodontists (AAE) Position Statement. October 2017. https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/silverpointsstatement.pdf. Accessed April 9, 2024.
16. Ng YL, Mann V, Rahbaran S, et al. Outcome of primary root canal treatment: systematic review of the literature - Part 1. Effects of study characteristics on probability of success. Int Endod J. 2007;40(12):921-939.
17. Salehrabi R, Rotstein I. Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study. J Endod. 2004;30(12):846-850.
18. Pratt I, Aminoshariae A, Montagnese TA, et al. Eight-year retrospective study of the critical time lapse between root canal completion and crown placement: its influence on the survival of endodontically treated teeth. J Endod. 2016;42(11):1598-1603.
19. Fransson H, Dawson VS, Frisk F, et al. Survival of root-filled teeth in the Swedish adult population. J Endod. 2016;42(2):216-220.
20. Suksaphar W, Banomyong D, Jirathanyanatt T, Ngoenwiwatkul Y. Survival rates from fracture of endodontically treated premolars restored with full-coverage crowns or direct resin composite restorations: a retrospective study. J Endod. 2018;44(2):233-238.
21. Dammaschke T, Nykiel K, Sagheri D, Schäfer E. Influence of coronal restorations on the fracture resistance of root canal‐treated premolar and molar teeth: a retrospective study. Aust Endod J. 2013;39(2):48-56.
22. Chugal N, Lin LM. Endodontic Prognosis: Clinical Guide for Optimal Treatment Outcome. 1st ed. Cham, Switzerland: Springer; 2017.
23. De Chevigny C, Dao TT, Basrani BR, et al. Treatment outcome in endodontics: the Toronto study-Phase 4: initial treatment. J Endod. 2008;34(3):258-263.
24. He J, White RK, White CA, et al. Clinical and patient-centered outcomes of nonsurgical root canal retreatment in first molars using contemporary techniques. J Endod. 2017;43(2):231-237.
25. Ng YL, Gulabivala K. Factors that influence the outcomes of surgical endodontic treatment. Int Endod J. 2023;56(suppl 2):116-139.
26. Brochado Martins JF, Guerreiro Viegas O, Cristescu R, et al. Outcome of selective root canal retreatment - a retrospective study. Int Endod J. 2023;56(3):345-355.
27. von Arx T, Jensen SS, Hänni S, Friedman S. Five-year longitudinal assessment of the prognosis of apical microsurgery. J Endod. 2012;38(5):570-579.
28. Truschnegg A, Rugani P, Kirnbauer B, et al. Long-term follow-up for apical microsurgery of teeth with core and post restorations. J Endod. 2020;46(2):178-183.
29. Kim S, Jung H, Kim S, et al. The influence of an isthmus on the outcomes of surgically treated molars: a retrospective study. J Endod. 2016;42(7):1029-1034.
30. Kim S, Kratchman S. Modern endodontic surgery concepts and practice: a review. J Endod. 2006;32(7):601-623.
31. de Lange J, Putters T, Baas EM, van Ingen JM. Ultrasonic root-end preparation in apical surgery: a prospective randomized study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104(6):841-845.
32. Penarrocha-Diago M, Maestre-Ferrin L, Penarrocha-Oltra D, et al. Influence of hemostatic agents upon the outcome of periapical surgery: dressings with anesthetic and vasoconstrictor or aluminum chloride. Med Oral Patol Oral Cir Bucal. 2013;18(2):e272-e278.
33. Song M, Kim SG, Shin SJ, et al. The influence of bone tissue deficiency on the outcome of endodontic microsurgery: a prospective study. J Endod. 2013;39(11):1341-1345.
34. Taschieri S, Del Fabbro M, Testori T, Weinstein R. Efficacy of xenogeneic bone grafting with guided tissue regeneration in the management of bone defects after surgical endodontics. J Oral Maxillofac Surg. 2007;65(6):1121-1127.