You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
When it comes to total tooth replacement, many patients consider dental implants to be the standard of care. Although implants have demonstrated high success rates, they are not without their complications.1 One of the most common is the loosening and ultimate fracture of the prosthetic screw that is used to attach the abutment or restoration to the osseointegrated fixture. The consequences of a fractured screw include, but are not limited to, discomfort, decreased function, and possible loss of the implant. Understanding the mechanical and environmental factors that influence the stability of implant-supported restorations is critical to predicting complications and managing them as they occur.
According to the American College of Prosthodontists, the single-unit crown is the most common implant-supported restoration, and approximately 2.3 million are performed annually.2 Research has shown that these restorations provide less resistance to screw loosening and fracture when compared with fixed implant-supported bridges.3 In one systematic review, after 5 years in function, single-unit crowns were shown to have a rate of loosening of 12.7% whereas fixed bridges had a rate of loosening of 5.6%.4 Detecting such disturbances can be difficult clinically because they may only be evident once a significant change has occurred.
Although implants have been shown to be a predictable treatment modality regarding their integration, prosthetic problems are still a common concern for the treating clinician. Prosthetic screw fracture can occur when a restoration is overloaded, but it is more often seen when a loose screw is under function in an undesirable position.5 Complications associated with prosthetic screws in single-unit implant-supported crowns have been reported to be dependent on a number of factors, many of which are mechanical and environmental.
Mechanical Factors
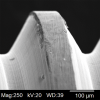
Prosthetic screws can be made of a variety of materials, including gold, pure titanium, and titanium alloy. When they are initially torqued to their full value, they undergo a period of tensile stress and elongation until they fit as intimately as possible with the internal components of the implant fixture. This initial tightening of the prosthetic screw is called the preload, and it is a critical component in maintaining the screw's torque value.6 Although some studies have suggested that gold screws generate better preload than their titanium counterparts, this is influenced by a number of factors.7,8 In further analysis of the prosthetic screws made of titanium, which are clinically common in dental practice, titanium alloy has been shown to provide greater resistance to loosening when compared with grade 4 pure titanium due to its lower coefficient of friction, which is often represented as μ.9 The coefficient of friction is a dimensionless number that represents the ratio of the amount of frictional force between two dissimilar objects and the amount of force holding them together on a scale of 0 to 1. Clinically, a lower coefficient of friction is desirable because it has been correlated with greater resistance to wear and higher preload values.10 Coefficient of friction is a significant factor in determining preload maintenance. Because it is currently impossible to machine perfectly fitting components, the first areas of contact between the screw and fixture are its highest, roughest areas (Figure 1). Of the initial torque placed on an implant screw, approximately 90% is used to overcome the friction in these uneven areas, and approximately 10% is converted to actual preload.11 The initial points of contact between the screw and implant are typically their imperfect areas, which are eventually flattened over time (Figure 1). Subsequently, this settling effect of the screw joints results in a loss of preload that occurs naturally without any additional forces acting on it in a process referred to as embedment relaxation. Although the time that this takes has been shown to vary, a clinical guideline of retorquing prosthetic screws 10 minutes after their initial placement has been proposed to reinforce the clamping effect and reestablish the desired torque value to maintain adequate preload. However, there is debate regarding the effectiveness of this guideline, and a universal protocol has not yet been established.12
Environmental Factors
One of the main factors that influences prosthetic screw loosening and the potential for fracture over time is the presence of parafunctional habits, such as bruxism. Typically, implants are best able to resist forces when they are directed down the long axis of the restoration-fixture complex.13 However, during the complicated movements associated with grinding habits, lateral forces will usually be acting on the implant as well, and they can have consequences over time. It has been reported that the lateral forces placed on implant-supported restorations can equate to approximately 25 Ncm during mastication, which is more unstable and unpredictable in its distribution of force along the implant components when compared with ideal loading forces.14 Although occlusal overload caused by bruxism has been shown to result in implant failure, this is typically an early problem associated with premature loading of the fixture. Later, after integration of the implant has been achieved, such overload has been correlated with screw loosening, screw fracture, and other negative consequences.15 For known bruxers, offering an occlusal splint as a first-line treatment is advisable to protect the integrity of the fixture and restoration and to prevent loosening of the screw and possible fracture.
Another factor that has an influence on metal fatigue and the propagation of existing imperfections over time that can lead to fracture is corrosion. Corrosion typically occurs as a result of the interaction between the metal components of the implant-restoration and the saliva and microbial flora of the oral environment.16 Although there is an inert layer of titanium dioxide that forms between the metal surfaces and the surrounding anatomy, a number of factors, including salivary components such as proteins and mineral salts as well as an acidic environment initiated by bacterial biofilms, have been shown to initiate and expedite titanium corrosion.17 For example, bacterial strains such as Streptococcus mutans and Actinomyces naeslundii have been shown to play a role in titanium oxide degradation by propagating organic acids that contribute to an acidic environment. As a component of their metabolism, they release different sulfides and H+ ions that can influence the development of corrosion over time and possibly lead to failure of the implant components. It has been suggested that coating titanium with compounds such as titanium nitride, silicon carbide, or silver and copper nanoparticles can lead to decreased torque loss and resistance to breakdown over time, but more research is necessary.17-19
Methods for Retrieval
Screw fracture demands retrieval of the broken fragments, which can be a difficult procedure—even for experienced clinicians. A number of methods for retrieval have been documented, and the best approach will depend on the specifics of the clinical scenario. When clinicians are familiar with a variety of techniques, it helps them to maximize their chance of success.
A number of implant rescue kits have been made available from implant manufacturers (eg, Medentika, Salvin Dental Specialties, Hiossen, Nobel Biocare, etc), and the most useful first-line treatment for a fractured prosthetic screw will typically be the rescue kit from the appropriate implant manufacturer if such a kit is to be used. Although in vitro studies have supported the use of rescue kits over other conventional means to retrieve screw fragments,20 such kits may not always be available or appropriate for the particular clinical scenario. When they are used, the manufacturer's instructions should always be carefully followed to safely remove the broken screw fragments and protect the implant's internal components. Oftentimes, rescue kits include a metal sleeve for guidance and protection so that a rotary handpiece can be used to create a channel in the screw fragment to engage it. Reverse torque is then applied to facilitate its removal. This technique may be particularly useful when the screw fragment is in the apical half of the implant. However, great care should be taken when using any handpiece near an implant because excessive heat can easily be generated if the number of revolutions per minute (rpm) reaches 2,000 rpm or greater, and this can result in surrounding bone damage at the implant's surface.20 Alternative conventional retrieval methods include the use of an ultrasonic instrument and hand instruments, but care must still be taken to not generate too much heat or cause internal damage.
Because there is no standard protocol for fractured screw removal, the methods and solutions that have been employed are numerous and often creative. One option involves the use of a small round carbide bur to create a slot in the top of the screw fragment. A small hand screwdriver can then be used to engage the slot and reverse the screw fragment out. Depending on the depth, a surgical bur may be required, and great care should be taken to avoid damaging the internal threads of the fixture. In this technique, the bur will often bounce off of the screw during contact and can easily touch the internal walls. This approach may also be useful in cases involving a stripped multiunit abutment.21
Visibility is often poor in retrieval cases, and poor visibility can make it difficult to position a handpiece so that it is directly centered over the fragment. Although visibility can be improved through the use of a microscope or loupes, the latter of which may be more readily available, other techniques have used modified impression copings to properly position a reverse-tapping rotary instrument to remove the fragment.22
All of the retrieval methods discussed here have merit when they are used in appropriate clinical situations. The following case report presents a modified conventional approach involving traditional dental materials that may be used to successfully and safely retrieve a screw fragment.
Case Report
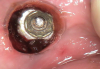
A 61-year-old male patient presented with the chief complaint of a missing implant-supported crown. The patient's dental history revealed a habit of grinding and clenching, and signs of wear were clinically evident during the examination. Because the implant restoration was placed 7 years prior at another practice, and the manufacturer and model were not immediately available, a universal protocol would be required to attempt the rescue. The patient reported that the crown had been dislodged for many weeks. As a result, the soft tissue had grown over the implant, completely covering it (Figure 2). A preoperative periapical radiograph was taken to help visualize the location and size of the remaining fragment (Figure 3). In addition, an intraoral camera would be used during the procedure to view the internal aspect of the fixture and aid in the retrieval process.
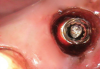
Once anesthesia was achieved, a periodontal probe was used to identify the extent of the implant platform, and then an appropriately sized biopsy punch was used to access the implant (Figure 4). Following access, a presoak of tartar and stain remover was injected into the fixture for a period of 10 minutes. This helped to remove any debris and corrosive elements that may have contributed to the difficulty of retrieval (Figure 5). A 0.36-mm capillary suction tip was used to remove the solution, and a new volume was deposited to penetrate the fixture as needed.
After the soak was complete, an ultrasonic tip was used with copious irrigation in a counterclockwise motion in short intervals to further loosen the screw fragment. The short intervals helped to reduce the amount of heat produced while still providing efficacy. After several rounds with the ultrasonic tip, a 25-gauge metal cannula was used to engage the top of the screw fragment and help rotate it in a counterclockwise direction. This use of the cannula was alternated with the ultrasonic tip to gain adequate movement of the fragment (Figure 6). Once the screw fragment was able to be retrieved, it was removed with the narrow suction tip (Figure 7). A healing abutment was then placed to contour the tissue until adequate healing occurred.
Following the healing period, a scan body was placed, and scan data were acquired to fabricate a new screw-retained, implant-supported restoration using a digital protocol (Figure 8). The patient returned, and after verification using a 3D printed model (Figure 9) and try-in, the restoration was delivered, and the prosthetic screw was torqued to the appropriate value. To block the screw channel, a piece of PTFE tape was placed over the prosthetic screw head to protect it; a universal bonding agent was applied to the occlusal third of the channel, air thinned, and light cured; and then a universal composite was placed, which provided an esthetic final result (Figure 10).
Conclusion
In modern dentistry, dental implants provide the standard of care for tooth replacement. Managing their complications is an inevitable part of the maintenance schedule; however, they are still recommended as ideal treatment. The current literature has identified risk factors for screw loosening and fracture that are clinically useful to the treating doctor in the design and delivery of such restorations. Advances in material science, implant design, and novel techniques for retrieval are helping to reduce the occurrence of any negative sequelae. Although no universal screw retrieval procedure exists that can manage every clinical scenario, being familiar with the current techniques documented in the literature provides clinicians with the tools to have the greatest chance of success.
Queries regarding this course may be submitted to authorqueries@aegiscomm.com
About the Author
Stephen Dadaian, DDS
Private Practice
Cresskill, New Jersey
References
1. Jung RE, Pjetursson BE, Glauser R, et al. A systematic review of the 5-year survival and complication rates of implant-supported single crowns. Clin Oral Implants Res. 2008;19(2):119-130.
2. American College of Prosthodontics. Facts & figures. American College of Prosthodontics website. https://www.gotoapro.org/facts-figures/. Accessed March 21, 2022.
3. Sailer I, Mühlemann S, Zwahlen M, et al. Cemented and screw-retained implant reconstructions: a systematic review of the survival and complication rates. Clin Oral Implants Res. 2012;23(Suppl 6):163-201.
4. Pjetursson BE, Brägger U, Lang NP, Zwahlen M. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin Oral Implants Res. 2007;18(Suppl 3):97-113.
5. Bakaeen LG, Winkler S, Neff PA. The effect of implant diameter, restoration design, and occlusal table variations on screw loosening of posterior single-tooth implant restorations. J Oral Implantol. 2001;27(2):63-72.
6. Winkler S, Ring K, Ring JD, Boberick KG. Implant screw mechanics and the settling effect: overview. J Oral Implantol. 2003;29(5):242-245.
7. Doolabh R, Dullabh HD, Sykes LM. A comparison of preload values in gold and titanium dental implant retaining screws. SADJ. 2014;69(7):316-320.
8. Nithyapriya S, Ramesh AS, Kirubakaran A, et al. Systematic analysis of factors that cause loss of preload in dental implants. J Indian Prosthodont Soc. 2018;18(3):189-195.
9. Shinohara R, Ueda K, Watanabe F. Influence of the difference between implant body and screw materials on abutment screw loosening. Dent Mater J. 2019;38(1):150-156.
10. Martin WC, Woody RD, Miller BH, Miller AW. Implant abutment screw rotations and preloads for four different screw materials and surfaces. J Prosthet Dent. 2001;86(1):24-32.
11. Siamos G, Winkler S, Boberick KG. The relationship between implant preload and screw loosening on implant-supported prostheses. J Oral Implantol. 2002;28(2):67-73.
12. Cardoso M, Torres MF, Lourenço EJ, et al. Torque removal evaluation of prosthetic screws after tightening and loosening cycles: an in vitro study. Clin Oral Implants Res. 2012;23(4):475-480.
13. Song JY. Implant complications in bruxism patients. J Korean Assoc Oral Maxillofac Surg. 2021;47(2):149-150.
14. Morneburg TR, Pröschel PA. In vivo forces on implants influenced by occlusal scheme and food consistency. Int J Prosthodont. 2003;16(5):481-486.
15. Alsubaiy EF. Abutment screw loosening in implants: a literature review. J Family Med Prim Care. 2020;9(11):5490-5494.
16. Olmedo DG, Tasat DR, Duffó G, et al. The issue of corrosion in dental implants: a review. Acta Odontol Latinoam. 2009;22(1):3-9.
17. Camargo SEA, Roy T, Xia X, et al. Novel coatings to minimize corrosion of titanium in oral biofilm. Materials (Basel). 2021;14(2):342.
18. Anchieta RB, Machado LS, Bonfante EA, et al. Effect of abutment screw surface treatment on reliability of implant-supported crowns. Int J Oral Maxillofac Implants. 2014;29(3):585-592.
19. Olmedo MM, Iglesias Godino FJ, Fernández Liétor P, et al. Corrosion and fracture analysis in screws of dental implants prostheses. New coatings. Eng Fail Anal. 2017;82:657-665.
20. Agustín-Panadero R, Baixauli-López M, Gómez-Polo M, et al. In vitro comparison of the efficacy of two fractured implant-prosthesis screw extraction methods: conventional versus mechanical. J Prosthet Dent. 2020;124(6):720-726.
21. Gober DD, Weitz ML. A solution for stripped dental implant screws. Perio-Implant Advisory website. https://www.perioimplantadvisory.com/clinical-tips/periodontal-complications/article/16412213/a-solution-for-stripped-dental-implant-screws. Published August 8, 2017. Accessed March 22, 2022.
22. Yoon JH, Lee H, Kim MY. Safe removal of a broken abutment screw with custom drill guide and rotary instrument: a clinical report. J Prosthodont. 2016;25(2):170-173.