You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The American Association of Orthodontists (AAO) recommends an initial orthodontic consultation for a child by no later than 7 years of age.1 Most orthodontic conditions can be treated easier and faster during this active growth period. The primary goal of interceptive orthodontics (phase 1, or early orthodontic therapy) is to intervene and enable a streamlined phase 2 comprehensive orthodontic treatment. Several conditions may be monitored for interceptive orthodontics in children ages 6 to 8. These include excessive space, severe crowding (lack of primate spacing), open bites, deep bites, anterior and/or posterior crossbites, severe overjet (ie, >10 mm), and abnormal eruption patterns such as ectopic permanent teeth. In this review, the etiologies of these clinical presentations will be discussed and divided into abnormalities in dental development, craniofacial growth alterations, and oral habits.
Abnormalities in Dental Development
Crossbite
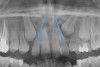
A common developmental abnormality is a localized anterior crossbite on permanent incisors, which may lead to trauma to these teeth. The most common cause of localized incisor crossbite is an anterior occlusal interference, which causes a functional shift when the patient moves from centric relation to centric occlusion (Figure 1 and Figure 2). This is not a true class III malocclusion, and proper diagnosis is critical to select the correct treatment. Sometimes this bite relationship is called a pseudo-class III relationship.2 Intervention in these cases is important because these teeth are at higher risk for recession, periodontal damage, and incisal chipping. Limited anterior braces and sometimes a palatal expander may be used to place the maxillary incisors facial to the mandibular incisors; this is referred to as "jumping the bite."
Too Few or Too Many Teeth
Another common developmental abnormality is the presence of either too few or too many teeth. This could be caused by a dental impaction, the presence of supernumary teeth, or missing teeth. When considering abnormal eruption patterns it is important to count the teeth and look for symmetry. The first sign of abnormalities in eruption may be that adult teeth are not erupting symmetrically within a 6-month span. The primary teeth may not be mobile. When warranted, it may be beneficial to obtain 2- or 3-dimensional radiology to gather more information, as these images may enable etiologies to be diagnosed such as the impaction of a central incisor due to the presence of an odontoma.3,4
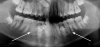
Dental impactions may occur for several reasons. A common occurrence is insufficient arch length leading to crowding. Another potential reason is early loss of primary teeth without proper space maintenance, allowing the permanent dentition to drift mesially and block out the primary tooth's successor. Maxillary canines are the most commonly impacted teeth besides third molars. These teeth have the longest path of eruption, are one of the last teeth to erupt into the mouth, easily become blocked out due to crowding or trauma history, and have a genetic component to being palatally impacted.5,6 Early signs of canine impaction may be severe crowding and the permanent lateral incisor crowns flaring distally. The crown of the impacted canine, in essence, is applying pressure to the roots of the lateral incisors in these instances (Figure 3 and Figure 4).
To prevent dental impactions, space maintenance and increasing the arch length are crucial factors. Literature shows that the extraction of primary canines often self-resolves about 90% of canine impactions as long as the canine crown is not mesial to the incisors, as per review of a panoramic image.7 Rapid palatal expansion (RPE) therapy is another approach to gain room and arch length.8
Supernumerary teeth constitute another form of dental eruption abnormality (Figure 5). Mesdiodens and distodens are relatively common, as are supernumerary premolars. Extraction of these teeth should be strongly considered so that they do not damage the roots of the permanent dentition. An additional caveat is that these anomalies often recur9; therefore, follow-up radiology is imperative.
Another important consideration is the possibility of missing teeth. The most common missing permanent teeth, excluding third molars, are second premolars and lateral incisors.10 The most likely reason for this is genetic or developmental in nature. Regarding missing premolars, the author prefers a conservative approach of maintaining the primary molars while planning for future implant placement when warranted. However, extraction may be preferred if the premolars are mobile with root loss, ankylosed, or become submerged, which may lead to future periodontal concerns. When lateral incisors are missing, esthetics must be a strong consideration in treatment decision-making. The two main treatment routes are canine substitution or leaving space for implant replacement once growth is completed.11 Females usually achieve growth completion between ages 16 to 18, while males are delayed to between ages 18 to 20.12,13
Canine substitution may be a viable option if the color of the canine is not significantly darker than the incisors, the anatomy is favorable from an esthetic perspective, and the gingival margin height discrepancy is insignificant. In such cases, canine substitution may be an alternative to premolar extraction in class II malocclusion camouflage treatment.14,15 It is important to explain to the patient that crowns may be indicated in the future to attain the most esthetic outcome.
Crowding
A third abnormality in dental development is crowding. Early intervention for severe crowding, ie, involving teeth that are >10 mm in mesial-distal width, may be necessary. Common causes of crowding include teeth that are large, eg, central incisors that are >10 mm wide, the presence of an arch circumference length and tooth size discrepancy, and early loss of primary teeth without space maintenance.16,17 Treatment options include serial extraction of primary teeth and possibly permanent premolars, which may especially be indicated in cases where a patient has particularly large teeth.18 Expansion is another option to balance out the arch length and tooth size discrepancy.
Finally, interproximal reduction may be used to decrease tooth width/size and improve upper/lower arch coordination. With this treatment, literature suggests an insignificant change in caries risk, and surfaces should be polished smoothly to minimize plaque build-up in the spaces that are created.19,20
Craniofacial Growth Modification
Although the face is a 3-dimensional structure, craniofacial growth modification is a topic that may be stratified by reviewing the transverse, vertical, and anterior-posterior dimensions. A transverse growth inadequacy is often illustrated in the form of a posterior (and often anterior) crossbite.21 The most common cause of this inadequacy is an underdeveloped maxilla, or, alternatively, an overdeveloped mandible; oftentimes a combination of these characteristics is the source of the problem. One example is a patient who has had cleft lip/palate repair, which may lead to craniofacial growth restriction in all dimensions (Figure 6 and Figure 7). When considering the transverse dimension, the most common treatment for a posterior crossbite is RPE therapy.21 In mild cases, archwire or dental expansion may suffice.
Craniofacial growth in the vertical dimension also must be considered. A patient with a vertical growth pattern may be diagnosed with an "adenoid face" or "long face syndrome."22 A vertical growth pattern often is associated with sleep-disordered breathing (SDB), a condition that is relatively common, present in 1% to 4% of children.23 It is important to note that snoring is not normal. The Mallampati score, which commonly is used preoperatively to evaluate airway patency, is often assessed along with neck circumference and body mass index to evaluate risk of SDB.24
It is crucial that dentists evaluate airway patency, because airway impingement may contribute to adverse craniofacial growth compensations and lead to sleep apnea in adulthood. Consequences of these conditions include vertical lower facial growth, an underdeveloped maxilla, lip incompetence, gummy smile, development of a tongue thrust habit along with mouth breathing, a forward head posture, and subocular venous pooling due to poor oxygenation (Figure 8). SDB may be associated with bed wetting, diagnosis of attention-deficit/hyperactivity disorder (ADHD), aggression, anxiety, poor academic performance, and childhood obesity.23,25 Treatment options for adenoid facies syndrome include RPE treatment, use of tooth positioners, and tonsil adenectomy (T&A). RPE treatment often helps convert mouth breathers into nasal breathers and improves tongue posturing. T&A surgery is warranted if airway obstruction is due to these enlarged tissues.
Lastly, the anteroposterior dimension is commonly recognized in dental and/or skeletal malocclusions. Skeletal malocclusions are highly prevalent, affecting 27.9% of the US population.26 Interventional treatments are performed predominantly for psychological-social reasons. A class II malocclusion occurs due to an overdeveloped maxilla and/or underdeveloped mandible, relative or absolute. On the contrary, a class III malocclusion presents with a relative or absolute underdeveloped maxilla and/or overdeveloped mandible. Class III malocclusions often have a genetic component in regard to an overdeveloped mandible (eg, "Habsburg jaw" royal family27).
Class II malocclusions (Figure 9) may be treated to reduce risk of dental trauma of protruding maxillary incisors or to break a lip trap habit. Some devices used for this purpose include headgears or functional appliances. Many orthodontists may wait to treat class II malocclusions in the permanent dentition because studies find inconclusive evidence of the effectiveness of phase I treatment.28 Early intervention is a strong consideration for class III malocclusion (Figure 10), with the goal of avoiding surgical treatment for either an adolescent or adult. This approach takes into consideration psychological-social concerns as well with regard to balancing facial disproportions and correcting the appearance of an "underbite" and/or prominent lower jaw.29 However, because there is a genetic component, surgery cannot be ruled out as a comprehensive treatment option. An early intervention would include facemask therapy with RPE to orthopedically protract and widen the upper jaw.
Oral Habits
The control of oral habits, such as thumb sucking, finger biting, lip biting, and tongue thrusting, also can serve as a means of orthodontic intervention. Thumb sucking is quite common as it offers a child comfort. Often it coincides with a tongue thrust habit. Thumb sucking should be addressed and, ideally, stopped before the patient generates any adult teeth. This potentially troublesome habit applies pressures to the maxillary and mandibular incisors, leading to an open bite and maxillary incisor proclination.30 Meanwhile, mandibular incisors may be retroclined. The open-bite tendency often leads to a tongue thrust habit, which continues to perpetuate the open bite.
Tongue and thumb pressures also contribute to a high-vaulted palate, which can lead to mouth breathing (Figure 11).31 Additional risks exist for infection and callus development on the thumb. Ideally, the child should quit this habit by age 4, before permanent occlusal changes develop.32 Quitting can be achieved through positive reinforcement and by offering the child comfort during thumb-sucking triggers. The use of bitterants (eg, Mavala Stop, Thum, Control-It!), which are painted on or rubbed into the thumb, is another option.33 A habit breaker appliance may also be utilized if these techniques are unsuccessful. Devices such as a palatal crib, rake, or bluegrass appliance interfere with the thumb and tongue habits and allow the bite to passively close.34 The author recommends utilizing a habit breaker appliance for 6 to 9 months and maintaining reinforcement for a few months once the habit is eliminated (Figure 12 through Figure 14).
Treatment for finger biting includes similar concepts as thumb sucking. This habit also may lead to dental flaring, calluses on fingers, and risk of infection.
Meanwhile, a lip-biting habit can lead to excessive overjet and lip incompetence. The overjet can be severe, equal to the thickness of the lip. Similar to thumb-sucking pressures, with lip biting the maxillary teeth flare and lower incisors tip back. Lips may appear as chapped or cracked. Positive reinforcement measures should be taken to try and break this habit. If they don't work, similar habit breaker devices as those used for thumb sucking may be employed.
A tongue thrust habit, which was previously discussed briefly, may occur sometimes as a result of or in combination with thumb sucking or vertical craniofacial growth patterns. It may also develop as a result of a delayed transition between infantile and adult swallowing patterns, which usually begins around age 2. By age 6, 50% of children have completed this transition.30 Tongue spurs or a palatal crib may be used to control this habit.
Prevention of Orthodontic Issues
A variety of topics may be discussed regarding prevention of orthodontic problems, including breastfeeding, diet and jaw growth stimulation concepts, space maintenance, and tooth positioners. Breastfeeding helps support proper upper and lower jaw development and positioning. While bottle-feeding positions the mandible distally, breastfeeding advances the mandible. This encourages the development of a class I occlusion. The sucking pressure allows for a 50% decrease in malocclusion and posterior crossbites based on muscle development.35,36 In addition, breastfeeding has numerous positive benefits, promoting nasal breathing and proper palate formation, minimizing the development of a tongue thrust habit while improving tongue pressures and stimulating taste buds.37
Chewing is important for jaw growth stimulation. According to Mew, the modern diet only requires 3% to 5% masticatory muscle forces.38 He, as well as Fujita and Maki,39 suggests that chewing tough foods may activate bony cells and promote jaw growth. Processed, softer foods may contribute to crowding, narrow dental arches, malocclusions, dental decay, and impacted third molars.40 In the United States, approximately 50% of all wisdom teeth are removed.41
In cases of premature loss of primary teeth or missing permanent teeth, space maintenance is crucial.42 Possible causes of such tooth loss include caries, trauma, or a congenital disorder. If proper spacing is not maintained, mesial tooth drift may occur,43,44 which can lead to impaction or ectopic eruption of permanent teeth, as previously discussed. Various designs of space maintainers are available, depending on the location in the mouth that needs space preservation. Common devices include the Nance arch for the maxilla (Figure 15), a lower lingual holding arch for the mandible (Figure 16), and a band and loop or distal shoe for unilateral cases of space loss (Figure 17). Band and loop appliances seem to have the highest longevity intraorally; generally, unilateral devices fare better than their bilateral counterparts.45
Tooth positioners, also known as eruption guidance appliances, are another popular device used to guide dental eruption and arch development during the mixed dentition. These typically are worn nightly for up to 6 months and come in various sizes, based on mesial-distal widths of permanent incisors. HealthyStart™/Ortho-Tain® (HealthyStart, http://www.healthystartchild.com; Ortho-tain, http://www.orthotain.com) and LM-Activator™ (LM Dental, https://www.lm-dental.com) are two examples of these devices. While the literature on tooth positioners is sparse, one study showed that treatment allowed for reduced overjet and overbite, improved class II molar relationships, and decreased mandibular anterior crowding in the early mixed dentition.46,47
Conclusion
To reiterate, the AAO recommends initial orthodontic consultations by no later than 7 years of age. The concept of interceptive orthodontics optimizes dentofacial growth and development. The aim of this treatment approach is to prevent or minimize dental development abnormalities while providing craniofacial growth modification, habit intervention, and preventative holistic concepts. Ultimately, the objective of this interventional model is to enable a straightforward comprehensive orthodontic treatment plan in the adolescent years.
About the Author
Whitney Mostafiz, DMD, MS, Adjunct Clinical Assistant Professor, Department of Orthodontics, New York University College of Dentistry; Private Practice specializing in Orthodontics, New York, New York
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. American Association of Orthodontists. AAO website. https://www.aaoinfo.org/_/frequently-asked-questions/. January 29, 2019.
2. Reyes A, Serret L, Peguero M, Tanaka O. Diagnosis and treatment of pseudo-class III malocclusion. Case Rep Dent. 2014;2014:652936. doi: 10.1155/2014/652936.
3. Singla S, Gupta S. Compound odontoma associated with impacted maxillary central incisor dictates a need to be vigilant to canine eruption pattern: a 2-year follow-up. Contemp Clin Dent. 2016;7(2):273-276.
4. Becker A. Early treatment for impacted maxillary incisors. Am J Orthod Dentofacial Orthop. 2002;121(6):586-587.
5. Manne R, Gandikota C, Juvvadi SR, et al. Impacted canines: etiology, diagnosis, and orthodontic management. J Pharm Bioallied Sci. 2012;4(suppl 2):S234-S238.
6. Bishara SE. Impacted maxillary canines: a review. Am J Orthod Dentofacial Orthop. 1992;101(2):159-171.
7. Ericson S, Kurol J. Early treatment of palatally erupting maxillary canines by extraction of the primary canines. Eur J Orthod. 1988;10(4)283-295.
8. O'Neill J. Maxillary expansion as an interceptive treatment for impacted canines. Evid Based Dent. 2010;11(3):86-87.
9. Stevenson W, McKechnie AD. Recurring supernumerary teeth. Report of a case. Oral Surg Oral Med Oral Pathol. 1975;40(1):76-80.
10. Rakhshan V. Congenitally missing teeth (hypodontia): a review of the literature concerning the etiology, prevalence, risk factors, patterns and treatment. Dent Res J (Isfahan). 2015;12(1):1-13.
11. Turpin DL. Treatment of missing lateral incisors. Am J Orthod Dentofacial Orthop. 2004;125(2):129.
12. Shah RA, Mitra DK, Rodrigues SV, et al. Implants in adolescents. J Indian Soc Periodontol. 2013;17(4):546-548.
13. Westwood RM, Duncan JM. Implants in adolescents: a literature review and case reports. Int J Oral Maxillofac Implants. 1996;11(6)750-755.
14. Thierens LAM, Verhoeven B, Temmerman L, De Pauw GAM. An esthetic evaluation of unilateral canine substitution for a missing maxillary lateral incisor. J Esthet Restor Dent. 2017;29(6):442-449.
15. Lupini D, Lempert SM, Cozzani M. Canine substitution of a missing maxillary lateral incisor in an orthodontic re-treatment case: long term follow up. South Eur J Orthod Dentofac Res. 2017;4(1):14-19.
16. DeAngelis V. Selection of teeth for extraction as an adjunct to orthodontic treatment. J Am Dent Assoc. 1973;87(3):610-615.
17. Almeida RR, Almeida MR, Oltramari-Navarro PV, et al. Serial extraction: 20 years of follow-up. J Appl Oral Sci. 2012;20(4):486-492.
18. Lopes Filho H, Maia LH, Lau TC, et al. Early vs. late orthodontic treatment of tooth crowding by first premolar extraction: a systematic review. Angle Orthod. 2015;85(3):510-517.
19. Barcoma E, Shroff B, Best AM, et al. Interproximal reduction of teeth: differences in perspective between orthodontists and dentists. Angle Orthod. 2015;85(5):820-825.
20. Jarjoura K, Gagnon G, Nieberg L. Caries risk after interproximal enamel reduction. Am J Orthod Dentofacial Orthop. 2006;130(1):26-30.
21. Almeida RR, Almeida MR, Oltramari-Navarro PV, et al. Posterior crossbite-treatment and stability. J Appl Oral Sci. 2012;20(2):286-294.
22. Agarwal L, Tandon R, Kulshrestha R, Gupta A. Adenoid facies and its management: an orthodontic perspective. Indian J Orthodontics Dentofacial Research. 2016;2(2):50-55.
23. Chang SJ, Chae KY. Obstructive sleep apnea syndrome in children: epidemiology, pathophysiology, diagnosis and sequelae. Korean J Pediatr. 2010;53(10):863-871.
24. Liistro G, Rombaux P, Belge C, et al. High Mallampati score and nasal obstruction are associated risk factors for obstructive sleep apnoea. Eur Respir J. 2003;21(2):248-252.
25. Umlauf MG, Chasens ER. Sleep disordered breathing and nocturnal polyuria: nocturia and enuresis. Sleep Med Rev. 2003;7(5):403-411.
26. Joshi N, Hamdan AM, Fakhouri WD. Skeletal malocclusion: a developmental disorder with a life-long morbidity. J Clin Med Res. 2014;6(6):399-408.
27. Lippi D, Pierleoni F, Franchi L. Retrognathic maxilla in "Habsburg jaw". Skeletofacial analysis of Joanna of Austria (1547-1578). Angle Orthod. 2012;82(3):387-395.
28. Wheeler TT, McGorray SP, Dolce C, et al. Effectiveness of early treatment of Class II malocclusion. Am J Orthod Dentofacial Orthop. 2002;121(1):9-17.
29. Begum Khan M, Karra A. Early treatment of Class III malocclusion: a boon or a burden? Int J Clin Pediatr Dent. 2014;7(2):130-136.
30. Kamdar RJ, Al-Shahrani I. Damaging oral habits. J Int Oral Health. 2015;7(4):85-87.
31. Tanny L, Huang B, Naung NY, Currie G. Non-orthodontic intervention and non-nutritive sucking behaviours: a literature review. Kaohsiung J Med Sci. 2018;34(4):215-222.
32. Ovsenik M, Farcnik FM, Korpar M, Verdenik I. Follow-up study of functional and morphological malocclusion trait changes from 3 to 12 years of age. Eur J Orthod. 2007;29(5):523-529.
33. Borrie FR, Bearn DR, Innes NP, Iheozor-Ejiofor Z. Interventions for stopping dummy or finger or thumb sucking habits in children. CochraneDatabase of Systematic Reviews. 2015;3:CD008694. doi: 10.1002/14651858.
34. Diwanji A, Jain P, Doshi J, et al. Modified bluegrass appliance: a nonpunitive therapy for thumb sucking in pediatric patients-a case report with review of the literature. Case Rep Dent. 2013;2013:537120. doi: 10.1155/2013/537120.
35. Viggiano D, Fasano D, Monaco G, Strohmenger L. Breast feeding, bottle feeding, and non-nutritive sucking; effects on occlusion in deciduous dentition. Arch Dis Child. 2004;89(12):1121-1123.
36. Peres KG, Cascaes AM, Nascimento GG, Victora CG. Effect of breastfeeding on malocclusions: a systematic review and meta-analysis. Acta Paediatr. 2015;104(467):54-61.
37. Mew J. The influence of the tongue on dentofacial growth. Angle Orthod. 2015;85(4):715.
38. Mew M. Craniofacial dystrophy: modern melting faces. Paper presented at: Ancestral Health Symposium 2012; August 9-11, 2012; Cambridge, MA. https://www.youtube.com/watch?v=VdsAAnatzHY. Accessed January 29, 2019.
39. Fujita Y, Maki K. Association of feeding behavior with jaw bone metabolism and tongue pressure. Jpn Dent Sci Rev. 2018;54(4):174-182.
40. Richter S, Eliasson ST. Erosive and mechanical tooth wear in Viking age Icelanders. Dent J (Basel). 2017;5(3):E24.
41. Friedman JW. The prophylactic extraction of third molars: a public health hazard. Am J Public Health. 2007;97(9):1554-1559.
42. Alexander SA, Askari M, Lewis P. The premature loss of primary first molars: space loss to molar occlusal relationships and facial patterns. Angle Orthod. 2015;85(2):218-223.
43. Tunison W, Flores-Mir C, ElBadrawy H, et al. Dental arch space changes following premature loss of primary first molars: a systematic review. Pediatr Dent. 2008;30(4):297-302.
44. Owen DG. The incidence and nature of space closure following the premature extraction of deciduous teeth: a literature study. Am J Orthod. 1971;59(1):37-49.
45. Qudeimat MA, Fayle SA. The longevity of space maintainers: a retrospective study. Pediatr Dent. 1998;20(4):267-272.
46. Myrlund R, Dubland M, Keski-Nisula K, Kerosuo H. One year treatment effects of the eruption guidance appliance in 7- to 8-year-old children: a randomized clinical trial. Eur J Orthod. 2015;37(2):128-134.
47. Bergersen EO. The eruption guidance myofunctional appliances: how it works, how to use it. Funct Orthod. 1984;1(3):28-35.