You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Since its introduction to dental literature in 2003,1 the All-on-4® (Nobel Biocare, www.nobelbiocare.com) treatment concept has proven to be a predictable2,3 and cost-effective4 method used for full-arch dental implant rehabilitation. True adherence to this manner of treatment involves restoring an arch with at least 4 dental implants, the distal of which are tilted up to 45 degrees, and immediately loading a screw-retained provisional prosthesis.5 Various articles have documented both short- and long-term success rates for All-on-4–style treatment, with dental implant and prosthetic survival rates consistently exceeding 98%.1-12 While these studies document the success rates for this treatment concept and others discuss variations on surgical design to accommodate specific anatomic situations,13-16 few studies examine complications associated with the procedure beyond standard infections or mechanical fracture of the prosthesis.1-20
Accordingly, the purpose of this article is to present obstacles and complications that may be encountered before, during, and after All-on-4–style treatment and how to manage them. The author draws on his experiences with treating more than 500 arches and more than 2000 dental implants using All-on-4–style treatment.
Presurgical Complications
Teeth Exfoliating With Initial Impressions
Many patients requiring All-on-4–style treatment have extremely compromised teeth that may be unintentionally removed during the initial impression process. This is typically due to severely decayed teeth or extremely mobile teeth secondary to advanced periodontal disease (Figure 1). Such situations must be recognized and these patients advised of the potential for tooth loss during the impression process.
When encountering teeth that have been exfoliated with impressions, the author typically cleans the exfoliated tooth and adjusts the length of the root so that the tooth may be temporarily bonded back into place using composite resin in a Maryland-bridge fashion. Occlusion is adjusted on the bonded tooth so that it makes no contact with opposing teeth.
On some occasions, the author has bonded patients’ natural exfoliated teeth to their existing removable partial prostheses. In select cases in which no adjacent teeth or removable prostheses are available for bonding of an exfoliated tooth, the author has used a transitional mini dental implant with a chairside-fabricated temporary crown as in interim restoration prior to the patient’s surgical procedure.
Intrasurgical Complications
Arterial Disruptions During Mucogingival Flap Reflection
Following the administration of local anesthesia, the first step in All-on-4–style treatment is full-thickness mucogingival flap reflection. Depending on anatomic variability, vasculature such as the greater palatine artery or sublingual artery, or various branches thereof, may be disrupted. Should this occur, excessive hemorrhaging may obscure visibility of the surgical field in addition to becoming a hazard for the patient.
Initial treatment in these situations involves administration of local anesthetic with at least 1:100,000 epinephrine.21 In most cases, the vasoconstrictor effect of epinephrine is enough to stop the hemorrhaging. Should the vasoconstrictor fail to alleviate the problem, an electrosurgical generator or laser with a coagulation setting may be applied to the source of hemorrhage. A third option for containing the bleed is to use a resorbable suture to tie off the vessel posterior to the site of hemorrhage (Figure 2).
Exposed Nerves
In cases of severe mandibular atrophy, supracrestal exposure of the mental foramen or inferior alveolar nerve (Figure 3) may be possible.8,22 When encountered, these situations require special consideration for incision design, mucogingival flap reflection, bone reduction, dental implant placement, soft-tissue reduction, and suturing. With exposed nerve tissue, each of these steps has the potential for causing damage.
When faced with an exposed inferior alveolar nerve, the author has placed dehydrated human amnion-chorion membrane (DHACM) directly onto the nerve fibers based on the positive outcomes that have been reported with DHACM nerve wraps around the prostatic neurovascular bundle in prostatectomy surgeries.23 In 4 cases of DHACM that the author used inferior alveolar nerve wraps, patients reported no adverse outcomes, such as permanent or transient anesthesia, paresthesia, hypoesthesia, or dysesthesia.
Pneumatized Maxillary Sinus Extending Below Bone Reduction Plane
It is well established that maxillary sinus pneumatization may occur following posterior maxillary tooth loss.24 In select cases, pneumatization of the maxillary sinus may extend beyond the anticipated horizontal plane of bone reduction required for All-on-4–style treatment (Figure 4). Failure to adequately reduce bone in these areas may lead to restorations of inadequate thickness that are at increased risk for fracture.25 Conversely, standard bone reduction in these areas may lead to significant damage to the Schneiderian membrane.
To overcome this complication, the author carefully reduces the residual maxillary crestal bone until crestal exposure of the Schneiderian membrane is achieved (Figure 5). On crestal visualization of the Schneiderian membrane, the author uses curettes to lift the membrane apically from the anticipated plane of bone reduction (Figure 6). The maxillary bone is then reduced apically, and the process is repeated until the desired amount of bone reduction is achieved. When performed in this manner, the Schneiderian membrane remains intact while crestal areas of reduced maxillary bone will have openings of varying degrees depending on the amount of bone reduction (Figure 7). The author does not augment these openings with bone graft and simply closes the surgical site with primary closures of thick mucogingival flaps. To date, patients receiving treatment from the author in this fashion have had no adverse outcomes (Figure 8).
Hemorrhage From Osseous Nutrient Canals
All-on-4–style treatment typically involves reduction of alveolar and/or basal bone (Figure 9) to achieve adequate restorative space for both the interim and final prostheses.25-27 During reduction of this bone, exposure of intraosseous nutrient canals28,29 may lead to hemorrhaging that may obscure visualization of the surgical field. If left uncontrolled, hemorrhaging from nutrient canals can become significant, resulting in excessive blood loss. It is not uncommon to encounter multiple concurrently hemorrhaging intraosseous nutrient canals, especially during mandibular bone reduction.
When faced with this situation, the author uses the blunt end of a handheld instrument, such as a Woodson instrument (Figure 10), to put heavy pressure on bone directly adjacent to the bleeding nutrient canal. This pressure typically deforms the adjacent bone to a point at which it occludes the hemorrhaging. The author has encountered hundreds of hemorrhaging intraosseous nutrient canals and has never had this technique fail to achieve the desired results.
Accessory Mental Foramina
The prevalence of accessory mental foramina is well documented in dental literature with findings from 2.7% to 13% (Figure 11).30-32 Accessory mental foramina pose a particular obstacle for All-on-4–style treatment because the mental foramen is the landmark used to determine the posterior limits of tilted implant placement (Figure 12).9 The presence of accessory mental foramina often requires more mesial placement of dental implants, thus limiting the anterior-posterior spread of the All-on-4–style prosthesis. Furthermore, in cases in which accessory mental foramina are located superior to the main mental foramen,30 the amount of bone reduction may be compromised, increasing the risk for prosthetic fracture.25 Presurgical cone-beam computed tomography (CBCT) scans and radiographs for proposed All-on-4–style surgeries should be scrutinized for accessory mental foramina (Figure 13). Notably, dental literature has shown that even with careful evaluation of CBCT scans, it is not possible to identify 100% of accessory mental foramina cases.31 As such, care should be taken during mucogingival flap reflection to search for this anatomic anomaly.
When encountering accessory mental foramina, the author has performed modifications to bone reduction and/or more mesial placement of posterior dental implants; on a few occasions, he has carefully dissected the nerve from the accessory mental foramen and relocated it to a more distal position. To date, the author has had no adverse outcomes in patients, such as permanent or transient anesthesia, paresthesia, hypoesthesia, or dysesthesia, resulting from this technique.
Sublingual Artery Insertion in the Anterior Mandible
Because All-on-4–style treatment in the mandible requires dental implant placement anterior to the mental foramina, special consideration should be given to the vasculature in this region. A number of articles have reported potentially life-threatening complications when dental implant placement has damaged vasculature in the anterior mandible. A 2015 literature review33 on immediate or immediate postoperative bleeding complications in implant dentistry noted that the most common cause of bleeding complications was damage to the sublingual artery. Although this literature review noted an absence of fatalities, advanced airway management by intubation was needed in 41% of patients and tracheostomy was required in 47% of patients. Certainly, avoidance of the sublingual artery during implant placement in the anterior mandible is paramount.
Cadaveric34,35 and CBCT36 assessments of vascular supply to the anterior mandible have found that lingual foramina for insertion of the sublingual artery most commonly occurs in the midline of the mandible. While the location of sublingual artery insertion in the anterior mandible is typically beyond the depth of bone reduction required for most All-on-4–style surgeries, it may be encountered in cases of severely resorbed mandibles. Furthermore, while dental implant placement is typically not required in the mandibular midline for All-on-4–style treatment, it is occasionally necessary to place a dental implant in this location. When faced with this situation, the author has modified the total amount of bone reduction in the anterior mandible to allow for safe placement of a dental implant that avoids vascular impingement while still enabling adequate prosthesis thickness.
Inadequate Bone Density
Multiple studies indicate that a high degree of primary implant stability is a prerequisite for the successful immediate loading of dental implants37,38 and that high insertion torque values are correlated to high primary implant stability.39-42 Insertion torque and primary implant stability have proven to be substantially dependent on bone density with denser bone producing a more favorable situation.42 In cases of inadequate bone density, or “soft bone,” some authors have recommended underpreparing dental implant osteotomies to achieve improved implant stability.7,9 Although this technique is effective in many cases, select instances arise in which underpreparing the bone still results in low initial torque values.
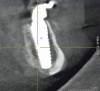
When such instances occur, whether in the mandible or maxilla, the author first attempts to place a larger-diameter implant of the same length as the implant that failed to achieve high initial torque value. Should this adjustment prove ineffective, a longer implant of a larger diameter is then used. In the maxilla, the longer implant may engage the vomer or lateral piriform rims to achieve apical stability.13 In the mandible, the author achieves primary implant stability by engaging the cortical bone at the inferior border of the mandible with the apical portion of the dental implant (Figure 14 and Figure 15).
Removal of Dental Implants
All-on-4–style treatment sometimes requires the removal of previously placed dental implants (Figure 16 and Figure 17). Although some of these implants may have biologic complications such as peri-implantitis that may ease the removal process, most previously placed implants requiring explantation by the author have been firmly osseointegrated. Previously placed dental implants are not typically suitable for All-on-4–style surgeries because the platforms were placed to a level in accordance with the natural teeth. Although this is perfectly suitable when natural teeth are present, these platform positions are too coronal for All-on-4–style treatment. Furthermore, previously placed dental implants preclude the ability for adequate bone reduction. In the author’s experience, using previously placed dental implants for All-on-4–style treatment often results in restorations of inadequate thickness that have a propensity for fracture due to the coronal position of the platforms and the lack of bone reduction. As such, the author routinely removes previously placed dental implants when performing All-on-4–style treatment.
Dental implant removal for All-on-4–style surgery is particularly concerning because of the need for immediately loading a prosthesis. Dental implants requiring removal are typically the same diameter as the implants intended for use in the All-on-4–style surgery. If the implants can be removed with a high-torque dental implant retrieval tool (Figure 18), bone is preserved and a dental implant of at least the same diameter and length can be used for the All-on-4–style treatment. Should the implant retrieval tool fail to explant the previously placed dental implant, trephination is required. The bone loss subsequent to trephination of a dental implant may eliminate the possibility of placing a new implant and thus compromise immediate loading of a transitional prosthesis. As has been reported by others,43-45 the author has had a high degree of success in removing previously placed dental implants with high-torque retrieval tools. In cases in which trephination was required, the author has replaced the previously existing implants with new implants of both wider and longer dimensions.
Postsurgical Complications
Fracture of Provisional Restorations
Postsurgical biologic complications following All-on-4–style dental implant surgery are rare.1-12 The most common postsurgical complication following this surgery noted in the dental literature is fracture of the provisional restoration, with rates from 4.17% to 41%.46-48 Fractures of provisional All-on-4–style restorations during healing are concerning, because they eliminate cross-arch stabilization and disrupt stress distribution patterns. Furthermore, fractures of these prostheses are unsettling to patients because they impair masticatory function and marginalize esthetics. The most common causes of fractured All-on-4–style provisional restorations are prostheses of inadequate thickness due to under-reduced bone, processing errors, or improper occlusal adjustment.46 In some cases, however, fractures may occur because acrylic and polymethyl methacrylate materials are inadequate for extended periods of heavy occlusal use.
To reduce the incidence of postsurgical fracture of All-on-4–style provisional restorations, the author reinforces transitional prostheses with 1-mm-diameter interplaited steel wire (Figure 19 and Figure 20) based on the findings of research by Yamaguchi et al,49 Li et al,50 and others.51-53 Upon incorporating this reinforcement technique for All-on-4–style provisional restorations, the rates of fracture for the author’s provisional restorations decreased from 16.14% to 4.17%.46
Conclusion
Although All-on-4–style full-arch dental implant procedures have one of the highest success rates of any treatment in dental literature, the technique is also among the most difficult and can be fraught with obstacles. With careful planning and knowledge of potential pitfalls associated with performing the procedure, clinicians can incorporate All-on-4–style dental implant treatment into their practices with a high degree of confidence and less stress.
Disclosure
The author had no disclosures to report.
About the Author
Dan Holtzclaw, DDS, MS Consultant Faculty, US Navy Postgraduate Dental School, Department of Periodontics, Bethesda, Maryland; Private Practice, Austin, Texas
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Malo P, Rangert B, Nobre M. “All-On-Four” immediate-function concept with Brånemark System implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5 suppl 1:2-9.
2. Malo P, Nobre M, Lopes A. The rehabilitation of completely edentulous maxillae with different degrees of resorption with four or more immediately loaded implants: a 5-year retrospective study and a new classification. Eur J Oral Implantol. 2011;4(3):227-243.
3. Malo P, de Araujo Nobre M, Lopes A, et al. “All-on-4” immediate-function concept for completely edentulous maxillae: a clinical report on the medium (3 years) and long-term (5 years) outcomes. Clin Impl Dent Rel Res. 2012;14 suppl 1:e139-e150.
4. Babbush CA, Kanawati A, Kotsakis GA, Hinrichs JE. Patient-related and financial outcomes analysis of conventional full-arch rehabilitation versus the All-on-4 concept: a cohort study. Implant Dent. 2014;23(2):218-224.
5. Malo P, Araujo Nobre MD, Lopes A, Rodrigues R. Double full-arch versus single full-arch, four implant-supported rehabilitations: a retrospective, 5-year cohort study. J Prosthodont. 2015;24(4):263-270.
6. Malo P, de Araujo Nobre M, Lopes A, et al. A longitudinal study of the survival of All-on-4 implants in the mandible with up to 10 years of follow-up. J Am Dent Assoc. 2011;142(3):310-320.
7. Agliardi E, Panigatti S, Clerico M, et al. Immediate rehabilitation of the edentulous jaws with full fixed prostheses supported by four implants: interim results of a single cohort prospective study. Clin Oral Implants Res. 2010;21(5):459-465.
8. Butura CC, Galindo DF, Jensen OT. Mandibular all-on-four therapy using angled implants: a three-year clinical study of 857 implants in 219 jaws. Dent Clin North Am. 2011;55(4):795-811.
9. Babbush CA, Kutsko GT, Brokloff J. The all-on-four immediate function treatment concept with NobelActive implants: a retrospective study. J Oral Implantol. 2011;37(4):431-445.
10. Balshi TJ, Wolfinger GJ, Slauch RW, Balshi SF. A retrospective analysis of 800 Brånemark System implants following the All-on-Four™ protocol. J Prosthodont. 2014;23(2):83-88.
11. Malo P, Nobre Mde A, Lopes A. Immediate rehabilitation of completely edentulous arches with a four-implant prosthesis concept in difficult conditions: an open cohort study with a mean follow-up of 2 years. Int J Oral Maxillofac Implants. 2012;27(5):1177-1190.
12. Holtzclaw D, Toscano N, Yang J. A retrospective analysis of patients treated with the All-on-4 treatment concept using a variety of different dental implant systems. J Implant Adv Clin Dent. 2015;7(5):11-18.
13. Jensen OT, Adams MW, Butura C, Galindo DF. Maxillary V-4: Four implant treatment for maxillary atrophy with dental implants fixed apically at the vomer-nasal crest, lateral pyriform rim, and zygoma for immediate function. Report on 44 patients followed from 1 to 3 years. J Prosthet Dent. 2015;114(6):810-817.
14. Jensen OT, Adams MW. All-on-4 treatment of highly atrophic mandible with mandibular V-4: report of 2 cases. J Oral Maxillofac Surg. 2009;67(7):1503-1509.
15. Jensen OT, Adams MW. Secondary stabilization of maxillary m-4 treatment with unstable implants for immediate function: biomechanical considerations and report of 10 cases after 1 year in function. Int J Oral Maxillofac Implants. 2014;29(2):e232-e240.
16. Jensen OT, Adams MW. The maxillary M-4: a technical and biomechanical note for all-on-4 management of severe maxillary atrophy—report of 3 cases. J Oral Maxillofac Surg. 2009;67(8):1739-1744.
17. Jensen OT, Cottam JR, Ringeman JL, et al. Angled dental implant placement into the vomer/nasal crest of atrophic maxillae for All-on-Four immediate function: a 2-year clinical study of 100 consecutive patients. Int J Oral Maxillofac Implants. 2014;29(1):e30-e35.
18. Drago C. Cantilever lengths and anterior-posterior spreads of interim, acrylic resin, full-arch screw-retained prostheses and their relationship to prosthetic complications. J Prosthodont. 2016; doi: 10.1111/jopr.12426.
19. Zhao X, Di P, Lin Y, et al. Implanting the edentulous jaws with “All-on-4” immediate reconstruction: a preliminary clinical observation. Beijing Da Xue Xue Bao. 2014;46(5):720-726.
20. Tallarico M, Canullo L, Pisano M, et al. An up to 7-year retrospective analysis of biologic and technical complications with the All-on-4 concept. J Oral Implantol. 2015; Epub ahead of print.
21. Moore P, Doll B, Delie R, et al. Hemostatic and anesthetic efficacy of 4% articaine HCl with 1:200,000 epinephrine and 4% articaine HCl with 1:100,000 epinephrine when administered intraorally for periodontal surgery. J Periodontol. 2007;78(2):247-253.
22. Ben Hadj Hassine M, Bucci P, Gasparro R, et al. Safe approach in “All-on-four” technique: a case report. Ann Stomatol (Roma). 2015;5(4):142-145.
23. Patel VR, Samavedi S, Bates AS, et al. Dehydrated human amnion/chorion membrane allograft nerve wrap around the prostatic neurovascular bundle accelerates early return to continence and potency following robot-assisted radical prostatectomy: propensity score-matched analysis. Eur Urol. 2015;67(6):977-980.
24. Tolstunov L, Thai D, Arellano L. Implant-guided volumetric analysis of edentulous maxillary bone with cone-beam computerized tomography scan. Maxillary sinus pneumatization classification. J Oral Implantol. 2012;38(4):377-390.
25. Holtzclaw D, Telles R. Analysis of fractures in All-On-4 provisional restorations using a standardized classification system. J Implant Adv Clin Dent. 2015;7(7):17-25.
26. Jensen OT, Adams MW, Cottam JR, et al. The All-on-4 shelf: maxilla. J Oral Maxillofac Surg. 2010;68(10):2520-2527.
27. Jensen OT, Adams MW, Cottam JR, et al. The All-on-4 shelf: maxilla [comment]. J Oral Maxillofac Surg. 2011;69(1):175-181.
28. Ogawa A, Fukuta Y, Nakasato H, Nakasato S. Cone beam computed tomographic evaluation of nutrient canals and foramina in the anterior region of the mandible. Surg Radiol Anat. 2016; Epub ahead of print.
29. Kawashima Y, Sekiya K, Sasaki Y, et al. Computed tomography findings of mandibular nutrient canals. Implant Dent. 2015;24(4):458-463.
30. Han SS, Hwang JJ, Jeong HG. Accessory mental foramina associated with neurovascular bundle in Korean population. Surg Radiol Anat. 2016; Epub ahead of print.
31. Muinelo-Lorenzo J, Suarez-Quintanilla JA, Fernandez-Alonso A, et al. Anatomical characteristics and visibility of mental foramen and accessory mental foramen: panoramic radiography vs. cone beam CT. Med Oral Patol Oral Cir Bucal. 2015;20(6):e707-e714.
32. Voljevica A, Talovic E, Hasanovic A. Morphological and morphometric analysis of the shape, position, number and size of mental foramen on human mandibles. Acta Med Acad. 2015;44(1):31-38.
33. Balaguer-Marti JC, Penarrocha-Oltra D, Balaguer-Martinez J, Penarrocha-Diago M. Immediate bleeding complications in dental implants: a systematic review. Med Oral Patol Oral Cir Bucal. 2015;20(2):e231-e238.
34. Liang X, Jacobs R, Lambrichts I, Vandewalle G. Lingual foramina on the mandibular midline revisited: a macroanatomical study. Clin Anat. 2007;20(3):246-251.
35. Fujita S, Ide Y, Abe S. Variations of vascular distribution in the mandibular anterior lingual region: a high risk of vascular injury during implant surgery. Implant Dent. 2012;21(4):259-264.
36. Tagaya A, Matsuda Y, Nakajima K, et al. Assessment of the blood supply to the lingual surface of the mandible for reduction of bleeding during implant surgery. Clin Oral Implants Res. 2009;20(4):351-355.
37. Esposito M, Grusovin MG, Willings M, et al. Interventions for replacing missing teeth: different times for loading dental implants. Cochrane Database Syst Rev. 2007;(2):CD003878.
38. Esposito M, Grusovin MG, Coulthard P, Worthington HV. Different loading strategies of dental implants: a Cochrane systematic review of randomized controlled clinical trials. Eur J Oral Implantol. 2008;1(4):259-276.
39. Trisi P, Berardi D, Paolantonio M, et al. Primary stability, insertion torque, and bone density of conical implants with internal hexagon: is there a relationship? J Craniofac Surg. 2013;24(3):841-844.
40. Schnitman PA, Hwang JW. To immediately load, expose, or submerge in partial edentulism: a study of primary stability and treatment outcome. Int J Oral Maxillofac Implants. 2011;26(4):850-859.
41. Heschl A, Payer M, Platzer S, et al. Immediate rehabilitation of the edentulous mandible with screw type implants: results after up to 10 years of clinical function. Clin Oral Implants Res. 2012:23(10):1217-1223.
42. Salimov F, Tatli U, Kürkçü M, et al. Evaluation of relationship between preoperative bone density values derived from cone beam computed tomography and implant stability parameters: a clinical study. Clin Oral Implants Res. 2014;25(9):1016-1021.
43. Anitua E, Murias-Freijo A, Piñas L, et al. Nontraumatic implant explantation: a biomechanical and biological analysis in sheep tibia. J Oral Implantol. 2016;42(1):3-11.
44. Anitua E, Orive G. A new approach for atraumatic implant explantation and immediate implant installation. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113(3):e19-e25.
45. Stajčić Z, Stojčev Stajčić LJ, Kalanović M, et al. Removal of dental implants: review of five different techniques. Int J Oral Maxillofac Surg. 2016;45(5):641-648.
46. Holtzclaw D. The effects of reinforcement on the fracture rates of provisional All-on-4 restorations: a retrospective report of 257 cases involving 1182 dental implants. J Implant Adv Clin Dent. 2016;8(3):31-37.
47. Francetti L, Agliardi E, Testori T, et al. Immediate rehabilitation of the mandible with fixed full prosthesis supported by axial and tilted implants: interim results of a single cohort prospective study. Clin Implant Dent Relat Res. 2008;10(4):255-263.
48. Pomares C. A retrospective study of edentulous patients rehabilitated according to the ‘all-on-four’ or the ‘all-on-six’ immediate function concept using flapless computer-guided implant surgery. Eur J Oral Implantol. 2010;3(2):155-163.
49. Yamaguchi K, Ishiura Y, Tanaka S, Baba K. Influence of the rigidity of a provisional restoration supported on four immediately loaded implants in the edentulous maxilla on biomechanical bone-implant interactions under simulated bruxism conditions: a three-dimensional finite element analysis. Int J Prosthodont. 2014;27(5):442-450.
50. Li BB, Xu JB, Cui HY, et al. In vitro evaluation of the flexural properties of All-on-Four provisional fixed denture base resin partially reinforced with fibers. Dent Mater J. 2016;35(2):264-269.
51. Kostoulas IE, Kavoura VT, Frangou MJ, Polyzois GL. The effect of length parameter on the repair strength of acrylic resin using fibers or metal wires. Gen Dent. 2008;56(1):51-55.
52. Heidari B, Firouz F, Izadi A, et al. Flexural strength of cold and heat cure acrylic resins reinforced with different materials. J Dent (Tehran). 2015;12(5):316-323.
53. Polyzois GL, Andreopoulos AG, Lagouvardos PE. Acrylic resin denture repair with adhesive resin and metal wires: effects on strength parameters. J Prosthet Dent. 1996;75(4):381-387.