You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
There are approximately 37 million people over the age of 65 currently living in the United States today; this number is projected to increase to 48 million by 2050.1 In the senior population of those 60 years or older, 25 are existing without any natural teeth.2 This aging populace is subject to a higher incidence of oral diseases and conditions as a result of the general unavailability of community water fluoridation, fluoride products, and dental insurance during its lifetime.3 This group demonstrates a higher consumption of prescription and over-the-counter medications that negatively affect the flow of saliva, which contains antimicrobial components and minerals that protect and remineralize teeth.1 These are but a few factors involved in the increasing tooth loss of the senior citizen population in America.
The dental literature of the last two decades is rife with articles and clinical cases detailing the processes of restoring diseased teeth and creating cosmetic smiles. Lacking, however, are current articles describing new and improved techniques for treating edentulous patients. Demographic trends indicate the necessity for complete denture treatment plans; practitioners' inclination to seek chair time maximization has resulted in modified approaches to complete denture cases. Fit, function, comfort, esthetics, and retention are the overall goals of every dental practitioner for their restorations. In this way, all types of dental prosthetic cases are similar: the dental impression must be perfected as it is critical to stable prosthesis fabrication.
The complete denture impression serves as a negative registration of the entire border and denture-bearing areas of the edentulous mouth.4 This is one of the most important steps in the complete denture process and yet is commonly taken for granted by clinicians. The goal for practitioners is to manipulate the impression surface and the peripheral rolls of the complete dentures so that support, retention, and stability of the dentures are maximized.
Complete denture impressions can be classified into preliminary impression and final impression groups that work together in the prosthetic fabrication process. The initial impression resembles the basic overall design for the complete denture and serves as the template for the final impression, recording the borders and base area without distortion. In both stages, impression accuracy and the ability of the material to replicate the detail of the clinical oral environment are of the utmost importance in ensuring a clinically accurate and seamless prosthetic/oral interface.
Impression Methods and Treatment Planning
Accurate impressions of the edentulous arch aid in the delivery of a stable, retentive, and comfortable complete denture.5 The final impression for complete dentures should capture the vestibule through border molding followed by impressioning the edentulous arch.6,7 The choice of final impression method should be considered in the treatment-planning phase of complete dentures; as with most dental procedures, choices in the beginning of the treatment often affect the end result of the denture case. The ideal impression requires embracing all of the edentulous areas to be used by the denture and depicting a replica of at-rest tissues without any over compression or displacement.4 Pressures exerted on tissues during the final impression can affect the quality of fit of the complete denture; impressions made with little or no pressure will result in a positive adaptation of the denture.8-10
Various methods and materials are considered commonplace for making complete denture impressions and have been documented in dental literature since the 1940s. These include: the selective pressure technique that provides for displacement of tissues in certain areas; the mucostatic/non-pressure impression technique that adheres to the principle of impressioning in an undistorted and nonstressed state; and the functional impression technique, where the muscular tissues that may interfere with denture stability can be identified and their functional movements accommodated for to provide better border seal and improved retention.11-13 These methods rely on the manipulation of the pressure exerted on the oral mucosa-namely soft tissues and underlying cortical bone-to improve clinical results. The load and location of pressure induced during impressioning is important and, if controlled, allows for a more retentive prosthesis.14
Final impressions of complete dentures are required to establish development of the peripheral contours to accommodate normal muscular function and to ensure peripheral adaptation without allowing air penetration between the denture base and the mucous membrane.19
Research and clinical results indicate a need to control pressure during edentulous impressioning, and certain oral areas require adapted techniques for success. Denture-supporting soft tissues are composed of firm, keratinized mucosa that will safely withstand the pressure resulting from the normal function of a denture;however, the thinner, non-keratinized alveolar mucosa will not tolerate functional loading of a prosthesis.16,17 The palate, residual ridges, and areas of easily displaced gingiva are areas of the edentulous mouth requiring little pressure, whereas increased pressure is needed in the border seal area of the denture, against the retromylohyoidfossa, and on the buccal shelf.18 Treatment planning by selecting the appropriate impressioning method for individual patients should be based on the diagnosis of the basal seat and border tissues.4
Often, the contraction of a muscle near its insertion can displace a denture, necessitating the need for a groove to accommodate such contractions. Clinical evidence of interfering muscle regions affecting denture stability often is difficult to detect in some patients; a record of the unique aspects of the patient's labial and buccal anatomy in the final impression is required to allow normal muscle activity without dislodging the denture during function.19
To combat potential problems unique to the functional impression technique, dental practitioners should use an accurate custom tray or tray alternative and use an effective material and border-molding technique. Several dynamic or functional impression methods are available to minimize unwanted pressures inherent in edentulous impressioning. Additionally, impression pressures can be controlled by material selection.20
Impression Material Selection
Viscosity and rheological flow characteristics are important properties to consider when selecting a material for complete denture cases. A direct relationship between the viscosity of impression materials and the pressure exerted on the oralmucosa has been recorded in the literature within the last 5 years. Studies at the University of Maryland in conjunction with the United States Naval Academy published in 2002 and 2006 indicate that low viscosity, light-body polyvinylsiloxanes and polysulfide materials produce the least pressure, where as medium-body polyvinyls and irreversible hydrocolloids exert the highest pressures on both the maxillary and mandibular arches.4,21 Furthermore, data from these studies showed that time vs pressure is linear for low-viscosity materials, resulting in stable set times and greater ease of use for light-body materials. Conversely, impressions made using high-viscosity materials result in pressure levels rising quickly, necessitating tray seating within 30 seconds after loading the tray to accommodate for quicker set times.Therefore, the use of light-body polyvinyl siloxane or polysulfide materials is recommended for minimum pressure and production of accurate impressions of minimally displaced mucosa.
Hydrophilic properties also are important considerations in material selection. When impression materials flow and meet moisture in the oral cavity, hydrophilicity becomes a critical factor in working time sand an important parameter in producing accurate casts in the dental laboratory.22 Polyvinyl materialsare known for their highly hydrophilic characteristics-another attribute to support their use in edentulous impressioning.
The Significance of Border Molding
The border molding process allows for close adaptation of a custom tray to the vestibule, which provides proper flange extension; it is a demanding procedure that establishes impression parameters to ensure favorable extensions for the final dentures.23,24 The objective of this part of the edentulous impression procedure is to customize the impression tray for each patient while providing a necessary seal on the peripheral edges without displacing the alveolar mucosa.
Errors common in border molding are the under-application of border-molding materials and the use of a tray that overextends, resulting in tissue impingement.25 It is important to seat the impression tray before impressing to evaluate the proximity to the border structures; the optimal relationship is 1 mm to 2 mm short of the borders, except in the posterior extension of the maxillary tray,where the vibrating line should be the end point. Despite these common errors and the time-consuming nature of the process, border molding is prevalent in the prosthodontic community; a 2003 survey of members of the American College of Prosthodontists indicated that 88% of respondents reported always using the border-molding technique before the final impression.26
Material selection is an important aspect in the success of border molding and the use of heavy-body, higher-viscosity, polyvinyl siloxanes has demonstrated rewards not evident in the application of traditional modeling compounds, such as: ease and accuracy of mixture; increased infection control; proper isolation to selected areas; reduction of material waste; and lack of the need for auxiliary equipment, which decreases procedure time.24
Saving time has become a deep desire of dental practitioners. From treatment planning and material selection to scheduling, the dental team is consistently finding new ways to reduce chair time, which pleases patients who dread denture treatments that typically take at least three if not five or six visits. The conventional complete denture process involves two distinct clinical sections for functional impressioning and jaw registration.27
The following clinical case outlines the fabrication of a new, replacement maxillary denture and its corresponding modified functional impression-taking technique. A unique approach was used to minimize chair time for a highly phobic dental patient by allowing a first try-in of the full set-up of denture teeth in the second visit without sacrificing prosthetic precision.
Clinical Case
A 74-year-old woman presented with a chief complaint of a worn, stained,ill-fitting maxillary complete denture that she felt had minimal esthetic value (Figure 1). The optimal treatment plan consisted of a new, complete set of removable dentures but was not accepted by the patient due to financial constraints. The patient opted for a new maxillary denture with plans to replace the mandibular prosthesis at a later time.
The patient underwent a complete medical history review and oral cancer screening, both of which resulted in no barriers to treatment. The patient's dental phobia was taken into consideration when treatment planning this case. A modified functional impression technique was planned for the final impression, which was the initial step in treatment. A large factor in choosing this particular technique was the on-site location of a dental laboratory that allowed for convenient, expedient model fabrication and articulation. The close proximity of laboratory to the operatory eliminated the need for shipping and return delivery of the denture in its various stages of completion, thus saving the patient and clinicians multiple appointments.
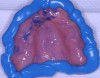
While the patient was viewing the CAESY Education Systems (Vancouver, WA) denture module on DVD in the operatory for consent and educational purposes, the mandibular denture was taken from the patient and impressed using an alginate alternative with an automix delivery system (AlgiNot, Kerr Corporation, Orange,CA) (Figure 2). After the 2-minute, 45-second set time recommended by the manufacturer, the denture was removed from the impression to reveal an accurate replica of the lower denture (Figure 3). The mandibular denture impression was disinfected with antimicrobial spray and walked to the dental laboratory, where it was poured up with yellow stone (Denstone® Golden, Heraeus Kulzer, Armonk, NY) by the laboratory technician to provide an occlusal reference and opposing model for the maxillary prosthesis. The lower denture was given back to the patient at this point in time and she was informed verbally of the next stepsin the procedure involving the use of her existing upper denture as a custom impression tray (Figure 4).
The upper denture was examined intraorally for purposes of detecting any over extensions into the peripheral border and to ensure the proper posterior dam position in relation to the vibrating line. This was necessary to evaluate the spacing needed to accommodate the proper border-molding technique in this modified functional impression-taking procedure. A slight overextension was detected on the left, distal peripheral area near the hamular notch and was removed and trimmed chair side to make room for the subsequent border molding. The denture was placed back in the mouth and was reevaluated for fit. Then the denture was removed and dried, followed by an application of polyvinyl impression adhesive to the tissue-bearing surfaces and peripheral borders on the denture (Figure 5). This liberal use of material ensured proper adhesion of the border molding material. A polyvinyl adhesive was needed to correspond with the chosen polyvinyl impression material.
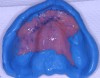
The patient's tissues were freed of excess saliva while the impression material (Take 1 Fast Set Tray Material, Kerr Corporation) was placed on the denture borders chairside (Figure 6). The denture was placed to begin the modified functional impression process and the standard border-molding adjustments to capture the details of the mu cco-buccal folds. After the 4-minute set time recommended by the manufacturer, the denture was removed and the impression was checked for insufficiencies (Figure 7). Once the border mold was deemed acceptable, a low-viscosity impression material (Take 1® Fast Set Wash Material, Kerr Corporation) was extruded onto the palatal area of the denture/tray to finely capture the necessary details of the edentulous mucosa (Figure 8 and Figure 9). A fluid, low-viscosity material is optimal for achieving this result and minimizing unwanted pressure on the maxilla. Again,the standard border-molding techniques were observed to ensure proper integration with the high-viscosity impression material and properly control the impression accuracy. The recommended 4-minute intraoral set-time was observed.
The maxillary denture impression was disinfected with antimicrobial spray and walked to the dental laboratory, where it was poured up with yellow stone (Denstone Golden) by the laboratory technician (Figure 10). The case was articulated with the occlusal pin set to replicate centric relation and centric occlusion (Figure 11). The laboratory technician made silicone putty molds (Extrude XP, Kerr Corporation) of the incisal edges of the upper denture. The articulated models were visually examined to ensure proper vertical dimension (Figure 12 and Figure 13). Subsequently, the impression material in the maxillary denture was removed and the denture was cleaned and lightly polished. It was returned immediately to the office, while the patient was waiting in the operatory, to be used as a temporary denture while the final case was completed. The patient was consulted as to preferences regarding teeth shade and shape. VITA Physiodens (Vident, Brea, CA) in Shade A2 were selected for this patient in the attempt to achieve natural-looking, age-appropriate dentition. The patient was dismissed and scheduled to return in 2 weeks for a functional try-in of the new denture.
The laboratory then fabricated a light-cured, stabilized base plate on which anterior and posterior teeth were set using the silicone putty mold made previously and waxed up to final contour and delivered to the office. The upper denture was tried in and a visual examination was performed to certify function, esthetics, phonetics, and patient/clinician satisfaction (Figure 14). The denture was sent back to the laboratory for final processing with the Ivocap Denture System (Ivoclar Vivadent North America, Amherst, NY). The prosthesis was trimmed and polished to high luster to prepare for final insertion (Figure 15). Additionally, Massachusetts requires denture labeling with a patient identifier (wearer's name, driver's license number, or Social Security Number, etc) for forensic purposes, and this was exacted according to state law.28
Conclusion
Because each patient as his or her own specific muscular activity and oral characteristics, the functional impression technique is widely used in today's practice of dentistry. The modified functional edentulous impressioning technique featured in this article allowed for the precise capture of important intraoral landmarks, such as the hamular notch, peripheral folds, and incisive papilla, along with centric relation and centric occlusion, in one standard office visit. This adapted technique eliminated the need for preliminary impressions, base plate and occlusal rims, and bite registration, which are practiced as part of traditional denture fabrication. This method also eliminated multiple visits, which can be sources of anxiety and frustration for many patients and clinicians.
Acknowledgement
The authors would like to thank Jennifer Towers for her work on this article.
References
1. US Census Bureau. Facts for Features. CB05-FF.07-2;2005. Available at : Accessed July 13, 2007.
2. US Center for Disease Control Web site.Oral Health for Older Americans-Resource Library Fact Sheet. Oral Health Resources;2006: 1-4. Available at:http://www.cdc.gov/OralHealth/factsheets/adult-older.htm. Accessed July 13,2007.
3. Vargas CM, Kramarow EA, Yellowitz JA.The Oral Health of Older Americans. PDF-285K. Aging Trends, No. 3. Hyattsville, MD: National Center for Health Statistics, 2001.Available at: http://www.cdc.gov/nchs/data/ahcd/agingtrends/03oral.pdf.Accessed July 13, 2007.
4. Al-Ahmad A, Masri R, Driscoll CF, et al. Pressure generated on a simulated mandibular oral analog by impression materials in custom trays of differentdesign. J Prosthodont. 2006;15(2):95-101.
5. Halperin AR. Mastering the Art of Complete Dentures. Chicago, IL:Quintessence;1988:31-34.
6. Davis DM. Developing an analogue for the maxillary denture-bearingarea. In: Zarb GA, Bolender CL, Carlsson GE,et al, eds. Boucher's Prosthodontic Treatment for Edentulous Patients. 11th ed. St. Louis, MO,Mosby, 1997:141-161.
7. Smutko GE. Making edentulous impressions. In: Winkler S, ed. Essentials of Complete Denture Prosthodontics. 2nd ed. Chicago, IL: Year Book Medical Pub; 1988:88-102.
8. Heartwell CM. Complete denture impressions. In: Syllabus of Complete Dentures. 2nd ed. Philadelphia, Pa:Lea and Febiger; 1974:157-184.
9. Zarb GA, Bolender CL, Hickey JL, et al.Biologic considerations for mandibular impressions. In: Boucher's Prosthodontics Treatment for Edentulous Patients. 10th ed. St Louis, MI:Mosby; 1990:194-223.
10. Collett HA. Final impressions for complete dentures. J Prosthet Dent. 1970; 23(3) :250-264.
11. Boucher CO. Impressions for complete dentures. J Am Dent Assoc. 1943; 30 :14-25.
12. Tryde G, Olsson K, Jensen SA, et al.Dynamic impression methods. J Prosthet Dent. 1965; 15(6) :1023-1034.
13. Page H. Mucostatics: A practical comparison. Tic. 1947:2-10.
14. Freeman SP. Impressions for completedentures. J Am Dent Assoc.1969;79(5):1173-1178.
15. Suenaga K, Sato T, Nishigawa G, et al.Relationship between size of complete foundation area and resorption ofalveolar ridge in the edentulous mandible. JOral Rehabil. 1997;24(4):315-319.
16. Jacobson TE, Krol AJ. A contemporary review of the factors involved in complete dentures. Part II: stability. J Prosthet Dent. 1983;49(2):165-172.
17. Jacobson TE, Krol AJ. A contemporary review of the factors involved in complete dentures. Part III: support. J Prosthet Dent. 1983;49(3):306-313.
28. Frank RP. Analysis of pressures produced during maxillary edentulous impression procedures. J Prosthet Dent.1969; 22(4) :400-413.
19. Malachias A, Paranhos Hde F, da Silva CH,et al. Modified functional impression technique for complete dentures. Braz Dent J. 2005;16(2):135-139.
20. Frank RP. Controlling pressures during complete denture impressions. Dent Clin North Am. 1970; 14(3) :453-470.
21. Masri R, Driscoll C, Burkhardt J, et al.Pressure generated on a simulated oral analog by impression materials in customtrays of different designs. J Prosthodont. 2002;11(3):155-160.
22. Kugel G, Klettke T, Goldberg JA, et al.Investigation of a new approach to measuring contact angles for hydrophilic impression materials. J Prosthodont.2007;16(2):84-92.
23. Felton DA, Cooper LF, Scurria MS.Predictable impression procedures for complete dentures. Dent Clin North Am . 1996;40(1):39-51.
24. Chaffee NR, Cooper LF, Felton DA. A technique for border molding edentulous impressions using vinyl polysiloxanematerial. J Prosthodont.1999;8(2):129-134.
25. Zarb GA, Bolender CL, Carlsson GE. Boucher's Prosthodontics Treatment for Edentulous Patients. 11th ed. St Louis, Mosby, 1997:141-182.
26. Petrie CS, Walker MP, Williams K. Asurvey of US prosthodontists and dental schools on the current materials and methods for final impressions for complete denture prosthodontics. J Prosthodont. 2005;14(4):253-262.
27. Utz K, Muller F, Kettner N, et al. Functional impression and jaw registration: a single session procedure for the construction of complete dentures. J OralRehab. 2004;31(6):554-561.
28. Collins D. The Dentist's Role in Forensic Identification: The Release of Dental Records & Radiographs, and Denture Labeling. American Dental Association Council on Dental Practice. 2004:1-14. Available at: www.ada.org/prof/prac/disaster/recover/volunteering_forensic.pdf.
About the Authors
Ronald Perry, DMD, MS, Director and Associate Clinical Professor, Gavel Center for Restorative Dental Research, Tufts University School of Dental Medicine, Boston, Massachusetts
John Orfanidis, Research Associate, Laboratory Technician, Orfan Dental Laboratories, Inc, Walpole, Massachusetts
Gerard Kugel, DMD, MS, PhD, Associate Dean for Research, Professor, Tufts University School of Dental Medicine, Boston, Massachusetts