You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
An understanding of anti-plaque mouthrinses must first involve comprehension of the dental plaque biofilm, especially the maturation sequence from an initially healthy to later harmful colonization of bacteria that contributes to the development of caries and periodontal disease.
Dental Plaque Biofilm
Many bacterial species normally freely floating in saliva can attach themselves to dental, gingival, and mucosal surfaces. When bacteria cluster together and attach to the gingival areas, a condition is created that can become a prerequisite for periodontal disease. A biofilm begins to form and the microbes undergo genotypic and phenotypic changes. The early colonizing bacteria of a newly forming biofilm are not periopathogenic and are considered beneficial in their association with gingival health. After attachment, the bacteria multiply and form micro-colonies that may expand and coalesce and are held together in a protective glue-like matrix, forming a dental plaque biofilm.1 This protective matrix is difficult to penetrate, reducing the effect of antimicrobial agents on biofilms.2 Dental plaque is an intricate biofilm in which many types of bacteria co-exist in a highly organized ecosystem where different communities are dependent on each other and communicate through signaling mechanisms. When these bacteria colonize the dental plaque biofilm, they release chemical signals that indicate to other species of bacteria that conditions are now favorable for them to become attached to the biofilm. The biofilm continues to grow in a predictable sequence of bacterial species. Biofilm associated bacteria are more resistant to antimicrobials compared to freely floating bacteria. Late colonizers, especially bacterial rods and filamentous organisms that become aggregated on the biofilm later in the process, are periodontal pathogens, capable of causing periodontitis. Figure 1 illustrates biofilm formation on a tooth surface. An undisturbed biofilm will advance from the supragingival to the subgingival region, potentially leading to gingivitis and periodontitis. Control of the plaque biofilm in the supragingival stage of its development is highly desirable if gingival health is to be maintained.
Reservoirs of pathogenic bacteria exist throughout the oral cavity, especially on the surface of the tongue and around the tonsils. Streams of bacteria propagate from these reservoirs and are transported to the tooth and gingival surfaces via saliva. Mechanical oral hygiene typically focuses on the dental and gingival areas, which constitute only about 20% of the total surface area of the oral cavity. The remaining 80% forms a reservoir of organisms that recolonizes recently cleaned surfaces. Supplementing mechanical plaque control with effective anti-plaque mouthrinses is a way of controlling this bacterial challenge by reaching the sites undisturbed by traditional brushing and interproximal cleaning techniques. Studies have shown that using an antimicrobial mouthrinse significantly reduces both salivary3 and mucosal4 levels of bacteria. Including an anti-plaque mouthrinse in daily oral hygiene procedures will help to reduce the total oral bacterial burden.
The healthy gingival sulcus is neither sterile nor devoid of bacteria. It is primarily populated with the non-pathogenic early biofilm colonizing species of bacteria.
As an undisturbed biofilm progresses from a health-associated to a disease-inducing state, it becomes apparent that the most important reason for repetitive daily home care—brushing, flossing, and rinsing multiple times per day—is related to the manner in which it develops. Every time the biofilm has been adequately disrupted, the same non-disease–causing bacteria are always the initial colonizers. Forcing the biofilm to start over as often as possible keeps the disease-causing periodontal pathogens floating freely in the oral cavity where they cannot cause caries or periodontal disease. The primary reason for repetitive home care is to make the biofilm start over and over.
Therapeutic Mouthrinses
Mouthrinses are available as over-the-counter (OTC) or prescription-only products and are categorized as either "cosmetic" or "therapeutic." Cosmetic mouthrinses do not reduce plaque or gingivitis but may claim to act as mouth or breath fresheners. These claims are not typically supported by scientific evidence. The Food and Drug Administration requires randomized controlled clinical trials for mouthrinses that claim therapeutic benefits in reducing levels of plaque and gingivitis. The therapeutic class of oral mouthrinses includes those containing essential oil compounds, cetylpyridinium chloride (CPC), chlorhexidine, and delmopinol.
Essential Oils
Essential oils have been used in mouthrinses for many years, dating back to the 19th century. The first over-the-counter mouthwash sold in the United States contained four essential oils: thymol, menthol, eucalyptol, and methyl salicylate (oil of wintergreen). The original formulation had a 26.9% alcohol content, and newer formulations have 21.6% alcohol. The antimicrobial activity is derived from the fixed combination of essential oils, not from the alcohol, which makes a very minor contribution to the antimicrobial activity. A 30-second rinse, twice daily, penetrates biofilm, providing a significant antimicrobial effect on supragingival biofilm.
Clinical trials have demonstrated plaque reductions of 13.8% to 56.3%, and gingivitis reductions of 14% to 35.9% when using essential oils.5-11 A study involving flossing and brushing with the mouthrinse showed an additional 15.8% reduction in interproximal gingivitis compared to a reduction of only 7.7% in the flossing and brushing group not using the mouthrinse.10
Mouthrinses with essential oils have been used by millions of consumers since their introduction more than 100 years ago and this formulation remains one of the most commonly available and used OTC therapeutic mouthrinses today.12
Cetylpyridinium Chloride
Cetylpyridinium chloride (CPC) is a cationic surface-active agent with widespread antimicrobial activity, involving the rapid destruction of Gram-positive pathogens and yeasts. CPC is found in many mouthrinses, including those with therapeutic benefits and those with only cosmetic claims. A recent meta-analysis from a systematic review supported the plaque- and gingivitis-inhibiting effect of CPC-containing mouthrinses. It concluded that CPC rinses, when used as adjuncts to oral hygiene, provide a small but significant additional benefit in reducing both plaque and gingival inflammation.13
The formulation of CPC ingredients includes solubilizers, preservatives, stabilizers, coloring agents, etc. The specific formulations can have a considerable impact on the bioavailability of the CPC. Increased proven bioavailability correlates with a higher probability of effectiveness, extending anti-plaque activity and reducing gingivitis.
The formulations of CPC rinses with the ADA Seal of Acceptance, which have demonstrated efficacy, are a different type of antimicrobial with a similar effect as the essential oils in reducing plaque and preventing gingivitis. Because it does not contain alcohol, it is an appropriate alternative for patients for whom alcohol-containing rinses are either not preferred or medically contraindicated.
Chlorhexidine Gluconate
Chlorhexidine gluconate has been used as a medical and surgical disinfectant since the 1940s. In 1970 it was found to be effective for use within the oral cavity.14 This prescription-only mouthrinse was originally formulated with alcohol (approximately 11.6%) but now alcohol-free formulations are available. Patients undergoing treatment for alcoholism, pregnant or nursing women, diabetics, or those who choose to avoid alcohol for cultural or religious reasons may prefer the alcohol-free formulations.
Chlorhexidine gluconate binds via adsorption to the many surfaces within the oral cavity, as well as the pellicle and saliva. This may explain its persistence in the oral cavity (substantivity) and its mode of action. Based on the concentration of chlorhexidine, the bactericidal or bacteriostatic effects will compromise bacteria attaching to the oral surfaces and may be more effective as a plaque preventive agent, rather than a plaque removal agent.15
Chlorhexidine gluconate is considered to be the gold standard16 for bacterial reduction and plaque control in the management of gingivitis. Prescription mouthrinses that contain chlorhexidine gluconate are available in therapeutically equivalent formulations that contain either 11.6% alcohol or no alcohol.
While chlorhexidine gluconate is an extremely effective mouthrinse, it has some side effects. Teeth, dental restorations, and the dorsum of the tongue are affected by chlorhexidine gluconate staining and some dental patients experience taste alterations and nausea. Addy has explained staining in terms of a reaction between chromogens found in foods and beverages and the tooth-bound chlorhexidine gluconate. Avoidance of these foods and beverages during treatment with chlorhexidine gluconate, especially soon after its application, should reduce the degree of stain formation.17
Delmopinol
The most recent and novel entry into the oral mouthrinse category is delmopinol hydrochloride. With a unique surfactant mechanism of action, delmopinol inhibits bacterial adhesion to tooth and mucosal surfaces, and also inhibits cohesion between the bacterial cells themselves. Mouthrinses containing delmopinol prevent bacteria from synthesizing the sticky glucan polysaccharide compounds that cause the adhesion to tooth and gum surfaces, and to the other bacterial cells nearby, and disrupt existing dental plaque biofilm colonies. When there are existing plaque colonies, the cohesive forces between the bacteria are reduced by delmopinol, which makes removal by mechanical means much easier. This formulation has a very low alcohol content (1.5%) and is indicated for all patients—especially those prone to significant plaque accumulation and chronic gingivitis. It is utilized as an adjunct to normal brushing, flossing, and other mechanical means of dental plaque biofilm removal. Research clearly indicates that delmopinol disrupts Streptococcus mutans and other cariogenic bacteria, as well as periodontal pathogens (Figure 2). This is very beneficial in terms of restricting development of caries and periodontal disease. Delmopinol usage results in less staining than chlorhexidine and the modest amount of staining is easily removed by professional methods and by patients' home care efforts. Clinical trials have shown that delmopinol 0.2% rinses reduced plaque by 9.3% to 35%, bleeding on probing by 18% to 36%, and gingivitis by 18%.18-20
A chart presenting summary data of clinical trials of the four anti-plaque agents demonstrates reductions of plaque, bleeding upon probing and gingivitis. All agents show significant efficacy and benefit for the patient's periodontal health (Table 1).
The formation of dental plaque biofilm starts supragingivally. If it is not controlled adequately, it proliferates in a subgingival direction into the sulcus. A proactive approach using therapeutic mouthrinses is most beneficial when plaque is found at the supragingival stage.
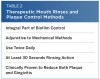
Mouthrinses are an integral part of daily biofilm control. All oral mouthrinses discussed are used as adjuncts to mechanical hygiene methods that include toothbrushing, flossing, and interdental cleaning (Table 2). All rinses should be used twice daily, for 30 seconds, and they all have been shown in clinical trials to reduce both plaque and gingivitis.5-11 The reason some patients progress to periodontitis and others do not is dependent on many factors including the immuno-inflammatory response, bacterial load, and genetic predisposition. Even large amounts of biofilm will not cause a progression from gingivitis to periodontitis in those who are not genetically predisposed.
Although gingivitis—with its redness, bleeding, and swelling of the gingiva—may be one of the most common diseases, it often does not receive the attention it deserves. It is important to control this condition in the early stages to reduce the progression of gingivitis to periodontitis. If a diagnosis of periodontitis occurs, it should be managed by both the provider and the patient with daily home care efforts and professional care from the dental team at three month intervals.
A large body of research indicates associations between oral and overall health.21 There have been associations established between periodontal disease and atherosclerosis, cardiovascular disease, and diabetes.22-26 Controlling the oral contribution to the total inflammatory burden and reducing the bacterial load, particularly the level of periodontal pathogens, helps achieve the goal of establishing and maintaining oral and general health.
Conclusion
Mechanical biofilm control is by no means the only answer to achieving gingival health. The addition of chemical agents to daily oral healthcare routines results in greater reductions in plaque and gingival inflammation. Attention to collateral concerns in restoring and maintaining gingival health include:
Patients who are unable to maintain adequate levels of plaque and gingivitis control can benefit from the supplementary use of any of the oral mouthrinses outlined in this article.
It is important that patients understand that use of anti-plaque/anti-gingivitis agents is not a panacea for good oral hygiene but should be used adjunctively to mechanical hygiene procedures.
Encourage patient compliance by recommending use of a well-designed toothbrush and adherence to proper biofilm control techniques.
Recommending adjunctive biofilm control measures is necessary for most patients.
Individual patient factors should be considered in determining the best method for biofilm control.
Mouthrinses are a necessary part of a daily home care regimen for the oral and general health of patients. Therapeutic mouthrinses are impactful beyond the oral areas available to mechanical biofilm control methods. This distinction makes mouthrinses essential players in the reduction of plaque and gingivitis that ultimately leads to beneficial oral health.
Disclosure
The author has received an honorarium from Sunstar Americas, Inc.
References
1. Listgarten MA. Formation of dental plaque and other oral biofilms. In: Newman HN, Wilson M, eds. Dental Plaque Revisited: Oral Biofilms in Health and Disease. Cardiff: BioLine; 1999:187-210.
2. Larsen T, Fiehn NE. Resistance of Streptococcus sanguis biofilms to antimicrobial agents. APMIS. 1996;104(4):280-284.
3. DePaola LG, Minah GE, Overholser CD, et al. Effect of an antiseptic mouthrinse on salivary microbiota. Am J Dent. 1996;9(3):93-95.
4. Fine DH, Furgang D, Sinatra K, et al. In vivo antimicrobial effectiveness of an essential oil-containing mouth rinse 12 h after a single use and 14 days' use. J Clin Periodontol. 2005;32(4):335-340.
5. Overholser CD, Meiller TF, DePaola LG, et al. Comparative effects of 2 chemotherapeutic mouthrinses on the development of supragingival dental plaque and gingivitis. J Clin Periodontol. 1990;17(8):575-579.
6. Lamster IB, Alfano MC, Seiger MC, Gordon JM. The effect of Listerine Antiseptic on reduction of existing plaque and gingivitis. Clin Prev Dent. 1983;5:12-16.
7. Gordon JM, Lamster IB, Sieger MC. Efficacy of Listerine antiseptic in inhibiting the development of plaque and gingivitis. J Clin Periodontol. 1985;12(8):697-704.
8. DePaola LG, Overholser CD, Meiller TF, et al. Chemotherapeutic inhibition of supragingival dental plaque and gingivitis development. J Clin Periodontol. 1989;16(5):311-315.
9. Charles CH, Sharma NC, Galustians HJ, et al. Comparative efficacy of an antiseptic mouthrinse and an antiplaque/antigingivitis dentifrice. A six-month clinical trial. J Am Dent Assoc. 2001;132(5):670-675.
10. Sharma N, Charles CH, Lynch MC, et al. Adjunctive benefit of an essential oil-containing mouthrinse in reducing plaque and gingivitis in patients who brush and floss regularly: a six-month study. J Am Dent Assoc. 2004;135(4):496-504.
11. Charles CH, Mostler KM, Bartels LL, Mankodi SM. Comparative antiplaque and antigingivitis effectiveness of a chlorhexidine and an essential oil mouthrinse: 6-month clinical trial. J Clin Periodontol. 2004;31(10):878-884.
12. Axelsson P. Preventive Materials, Methods and Programs. Vol. 4. Surrey, UK: Quintessence Publishing Inc.; 2004:184.
13. Haps S, Slot DE, Berchier CE, Van der Weijden GA. The effect of cetylpyridinium chloride-containing mouth rinses as adjuncts to toothbrushing on plaque and parameters of gingival inflammation: a systematic review. Int J Dent Hyg. 2008;6(4):290-303.
14. Löe H, Schiott CR. The effect of mouthrinses and topical application of chlorhexidine on the development of dental plaque and gingivitis in man. J Periodontal Res. 1970;5(2):79-83.
15. Jenkins S, Addy M, Wade W. The mechanism of action of chlorhexidine. A study of plaque growth on enamel inserts in vivo. J Clin Periodontol. 1988:15(7):415-424.
16. Jones CG. Chlorhexidine: is it still the gold standard? In: Addy M, Moran JM, eds. Toothpaste, mouth rinse and other topical remedies in periodontics. Periodontol 2000. 1997;15:55-62.
17. Addy M, Moran J. Chemical supragingival plaque control. In: Lindhe J, Lang NP, Karring T, eds. Clinical Periodontology and Implant Dentistry. 5th ed. Oxford: Blackwell Publishing, Ltd.; 2008:734-765.
18. Claydon N, Hunter L, Moran J, et al. A 6-month home-usage trial of 0.1% and 0.2% delmopinol mouthwashes (I). Effects on plaque, gingivitis, supragingival calculus and tooth staining. J Clin Periodontol. 1996;23(3 Pt 1):220-228.
19. Lang NP, Hase JC, Grassi M, et al. Plaque formation and gingivitis after supervised mouthrinsing with 0.2% delmopinol hydrochloride, 0.2% chlorhexidine digluconate and placebo for 6 months. Oral Dis. 1998;4(2):105-113.
20. Hase JC, Attstrom R, Edwardsson S, et al. 6-month use of 0.2% delmopinol hydrochloride in comparison with 0.2% chlorhexidine digluconate and placebo. (I). Effect on plaque formation and gingivitis. J Clin Periodontol. 1998;25(9):746-753.
21. Genco RJ. Current view of the risk factors for periodontal diseases. J Periodontol. 1996;67:1041-1049.
22. Scannapieco FA, Bush RB, Paju S. Associations between periodontal disease and risk for atherosclerosis, cardiovascular disease, and stroke. A systematic review. Ann Periodontol. 2003;8:38–53.
23. Meurman JH, Sanz M, Janket SJ. Oral health, atherosclerosis and cardiovascular disease. Crit Rev Oral Biol Med. 2004;15:403–413.
24. Khader YS, Albashaireh ZS, Alomari MA. Periodontal diseases and the risk of coronary heart and cerebrovascular diseases: a meta-analysis. J Periodontol. 2004;75:1046–1053.
25. Vettore MV. Periodontal disease and cardiovascular disease. Evid Based Dent 2004;5( ):69.
26. Elwood J. Critical appraisal of epidemiological studies and clinical trials. New York, NY: Oxford University Press; 1998.
About the Author
Richard H. Nagelberg, DDS
Private Practice
Plymouth Meeting, Pennsylvania