You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Understanding how the soft and hard tissues of the face change through adolescence, middle adulthood and in later life stages is important in attaining excellent facial and smile cosmetic outcomes. Some dentists may not consider that facial esthetics has much to do with them. However, a substantial body of research has been performed in the past several decades documenting the soft-tissue changes that occur with age and their potential effect on dental interdisciplinary treatment decision making. The influence on orthodontic thinking has been significant, with a focus shifting from treatment plans being based entirely on the occlusal relationships, to the balance of the teeth and smile presentation as well as soft-tissue support and facial appearance. This article presents the concept that the soft-tissue relationships of the face in regard to the underlying hard tissue are now primary determinates of the direction of orthodontic treatment. Growth of the face is an enormously complex function of the skeletal, dental, and soft-tissue growth, with genetic and environmental factors both playing significant roles in the final facial form. The idea that orthodontics and facial esthetics should be considered concurrently is not new but has recently received much attention from orthodontists. With the emphasis on interdisciplinary treatment, the mutual understanding of these principles is beneficial to the overall treatment outcomes.
This article presents pertinent data to practicing clinicians illustrated with two case presentations. This impacts how this knowledge can further improve actual treatments.
The Data
This article presents data that measures profile changes through time in a logical order to illustrate facial changes throughout life. This data will be related to clinical decisions that must be considered in adolescent, adult, and interdisciplinary cases. The first study documents the soft-tissue changes of the resting lips from age 8 to 18. The second study analyzed these same soft-tissue parameters in the group 18 to 42 years of age. The third study is a hard- and soft-tissue analysis of facial changes in the age range 7 to 80 years old. These and similar investigations were based on cephalometric measurements that help gauge profile changes. The final study covers long-term soft-tissue changes of the lips from the frontal dimension.
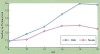
Mammandras1 evaluated the records of 32 untreated patients who represented a cross-sectional sample of ages 8 to 18 years and measured such variables as lip length, lip thickness, and soft-tissue chin thickness. Mammandras found that in women, the upper lip reached its maximum thickness by age 14 and remained the same until 16 years of age, with the lip thinning afterward. In men, maximum lip thickness was attained around age 16 but also began to thin thereafter (Figure 1). The horizontal thickness of the lower lip slowed dramatically but was close to its maximum in both men and women by age 15 (Figure 2). Similar results were attained in a study by Nanda et al2 with mild differences but essentially similar trends.
Does this trend in upper lip thinning level off or continue? What happens to the lower lip during this time? Formby et al3 investigated the same characteristics in a similar population from ages 18 to 42. They reported that in men, the overall profile became straighter and lips more retrusive. Upper lip thickness continued to decrease, while lower lip thickness slightly increased. In women, the profile did not straighten and upper lip thickness decreased, with a slight increase in lower lip thickness (as in the men). In dentistry, it is assumed that growth is finished in the late teen years because height gain ceases at about that time. Formby et al discovered that in men and women, the amount of change of both hard and soft tissues that occurred between ages 25 and 42 were similar to the degree of change occurring between ages 18 and 25. This finding alters the thinking regarding when orthodontic treatment is “finished” and explains many issues of retention that confront clinicians. It also has ramifications in the timing of implant placement.4,5
What happens through mid-adulthood (22 to 45 years) and older? The most comprehensive data available on these age groups were found in research by Behrents6 involving evaluation of patients ages 17 to 83. He determined that virtually all participants had significant skeletal and soft-tissue change. Behrents found that in adults (17 to 41 years), skeletal changes tended to be specific to their original craniofacial patterns. Patients who were Class III grew as Class III, and those who were Class II grew as Class II. These findings may be clinically significant—dentists are rarely surprised when an adolescent who received orthodontic treatment for a Class III malocclusion “relapses” with age into an edge-to-edge bite or a negative overjet. But dentists are surprised when a patient who received treatment for a Class II malocclusion develops an anterior slide occlusal discrepancy at a later time. It may be possible that dentists should expect a slide to develop in the patient with a Class II malocclusion. Behrents also documented substantial soft-tissue changes, reflecting that the upper lip continues to thin and remains a constant pattern throughout life. In addition, Behrents observed a clockwise rotation of the nasolabial complex, resulting in a longer upper lip. This leads to a decrease in incisor display at rest and on smile (Figure 3). This rotation also resulted in a lower nasal tip and more nasal projection (Figure 3). Throughout maturation and aging, the facial profile becomes flatter and greater nasal prominence with a proportionally shorter lower facial height.
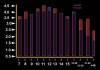
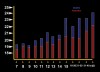
Dickens et al7 had performed direct clinical measurements of numerous frontal soft-tissue characteristics, including incisor at rest and philtrum height in a large sample of more than 1,300 participants and performed a cross-sectional analysis of the data. Figure 4 demonstrates the amount of incisor at rest diminishes with time (first studied by Vig and Brundo8), possibly as a result of the rotation of the nasolabial complex and subsequent inferior positioning of the upper lip, or increase in upper length itself. This decrease was greater in men than women. This fact has definite considerations in both orthodontics and cosmetic dentistry. In orthodontics, intrusion of the upper incisors should be a carefully considered procedure because it may result in hastening the age of the smile. Crown length in the placement of anterior veneers should also be “age-appropriate.” Figure 5 reflects the results of the philtrum measurements, and the researchers discovered that lengthening of the upper lip with age is a definite factor in the reduction in incisor display and subsequent decrease in gingival display on smile (Figure 6).
The aging process in a lifetime results in skeletal changes, such as further vertical maxillary and dentoalveolar development and mandibular length (Figure 7). Soft-tissue changes include reduced upper lip fullness, flatter profile, an increase in nasal projection with lowering of the nasal tip, and a more inferior position of the upper lip.
Case 1
An 11½-year-old girl was referred for treatment of her severe crowding with her dentist expecting a return visit for extractions. The patient’s dentition was severely crowded (Figure 8), with completely blocked-out canines. Her buccal occlusion (Figure 9) was a good Class I with the primary first and second molars still present. Will this patient require extraction to de-crowd the blocked out cuspids, or is this a non-extraction case? The clinician cannot make a decision with this information only. Without further knowledge of the face and smile, the immediate answer is “yes.” This patient was selected for illustrative case presentation for the following reasons: 1) the long-term changes of the face were an important factor in evolving the orthodontic treatment plan; 2) she represents an excellent illustration of how knowledge of the differential hard- and soft-tissue changes that occur during growth and maturation guides the treatment plan; 3) to demonstrate how the principles of soft-tissue growth can be used to the maximum advantage; and 4) emphasize how traditional cephalometric hard-tissue standards for treatment planning has a less significant place in the decision-making process.
In today’s contemporary multi-tiered approach to treatment, the timing of the referral was more than important; it was critical. Her profile (Figure 10) was flat and retrognathic because of her skeletal pattern and lack of dental and skeletal support, coupled with very thin upper and lower vermilion resulting in inadequate lip projection (also termed lack of vermilion display). In addition, she had a short lower facial height. The expected long-term changes expected were further profile flattening and shortening of the facial height. The treatment plan was evolved to address both the dental and facial esthetic needs and aim for an outcome that might improve facial esthetics, as well as offer her face some protection against aging. The first stage of the treatment plan was to take advantage of the prepubertal growth spurt and produce a relative orthopedic change in her growth phase (on average, age 11 to 11½ in girls, 12 to 12½ in boys, but determined by physical findings and history among other aspects). First, growth guidance therapy commenced at age 11 and cervical headgear was chosen because of its downward vector of force, an extrusive effect that not only helps open the deep bite but also increases lower facial height through the extrusion of the posterior teeth. During this phase of her treatment, the author assessed two treatment choices for addressing the dental crowding. First, serial removal of four premolar teeth could be implemented to create space. The crowding could be accommodated, and the resulting profile would not be worsened because the severity of her crowding would have no residual space for incisor retraction on space closure. Second, orthodontic arch expansion with incisor advancement in an anterior direction would have the potential to create enough room to accommodate the rest of the permanent dentition. In comparing her problems with the treatment options, extraction therapy would solve the crowding problem but would not improve lip projection. Given that her profile and lips should flatten with no treatment, incisor advancement has definite advantages because it would address the crowding problem while offering potential improvement in the lack of lip projection.
After approximately 9 months of mandibular growth guidance via headgear treatment, mandibular projection was dramatically improved as was the lower facial height. Exfoliation of the primary teeth was now complete, and the author began the fixed appliance phase of treatment. The resulting leeway space provided sufficient room to de-crowd the arches, along with arch expansion (with an emphasis on anterior expansion). Treatment was completed in the next 14 months, resulting in good occlusion (Figure 11) and dramatic profile improvement (Figure 12).
In today’s contemporary approach to orthodontic treatment, timing often is not dictated by whether all the teeth are “in” but to coincide with the skeletal growth spurt. The author suggests starting from the patient’s outward appearance.
Timing of the referral was one of the critical elements in the success of this patient’s outcome. In contemporary treatment of Class II malocclusion, the correlation between dental eruption and skeletal growth is weak. Thus, treatment must be approached with the dental and skeletal considerations regarded separately. The challenge is to achieve both in one phase if possible or to manage treatment in a reasonable period. The referral timing is much more a result of the patient’s relative skeletal growth status rather than whether the permanent teeth have erupted. In this case, the transitional dentition provided sufficient space to treat her problem without performing permanent tooth extraction. The positive approach to treatment of the face in concert with the dentition is important. Often, the orthodontic plan is designed to solely avoid problems. The amount of crowding in this case represented an opportunity to improve her facial esthetics. In the first case report, had four premolars been removed, the dentition would have been treated nicely to Class I standards; however, her physical appearance in 20 years would be affected. Her facial appearance (Figure 13) verifies this treatment approach was appropriate because the expected soft-tissue changes occurred regardless of treatment.
Case 2
Historically, orthognathic surgery has been an uncomfortable experience because of the use of intermaxillary fixation. This perception has persisted even today. The reality is that rigid fixation appeared in the mid 1980s (which requires no intermaxillary fixation), and the number of patients undergoing elective surgery who have been placed in intermaxillary fixation has been greatly reduced. Other benefits have included the incorporation of esthetic procedures (such as rhinoplasty), which can greatly enhance the esthetic outcome. In addition, dentists have aimed to make orthognathic surgery as acceptable to patients as rhinoplasty or facelift procedures.
This 48-year-old woman (Figure 14) was referred for consultation regarding her Class II malocclusion, with the referring dentist estimating she would most likely be offered both orthodontic and orthognathic surgical options. Her frontal image was characterized by very thin lip vermilion and deep nasal labial folds. Her smile (Figure 15) displayed a narrow transverse smile dimension (excessive buccal corridors) as a result of palatal tipping of the maxillary and mandibular premolars. She had a retrusive and flat profile (Figure 16), slightly inadequate lip projection, a low nasal tip, and a nasal dorsal hump. She had a short chin neck length (the distance from the front of her chin to the reflex point in her neck). The author anticipates that with aging, she will experience further loss of lip support and flattening of her profile with the lower ending of the nasal tip, accenting the dorsal hump and the overall aging characteristics of the profile.
Orthodontic treatment was planned to upright the maxillary incisors (decompensation) and widen the buccal corridors through uprighting of the premolars. The Class II malocclusion was to be corrected through mandibular advancement. Here the author exercised a departure from usual orthognathic planning in which solitary mandibular advancement would correct the malocclusion but would not offer much facial esthetic advantage (if desired by the patient). The patient was given the option of advancing both her maxilla and mandible, coupled with simultaneous rhinoplasty, to provide facial enhancement through support of both the soft tissues of the lips and face. Advancement of both jaws may improve the resting soft tissue through increasing skeletal volume. Moving all the hard tissues forward tightens up the soft tissues of the face.
After treatment completion, facial balance was dramatically better as was lip support (Figure 17). Her smile width was greatly improved (Figure 18) through two mechanisms. First, uprighting of the premolars consumes “negative space” with the premolar crowns. Second, the significant advancement of both dental arches through the bimaxillary advancement brought the wider portion of both arches into the lip drape, also reducing negative space. The final profile was remarkable in its enhancement of her existing profile with its rejuvenative effects of increased chin neck length and refined nasal anatomy (Figure 19).
The change in approach to orthognathic surgery has been dramatic in recent decades. Coupling orthognathic surgery with rhinoplasty and other adjunctive procedures at the same time as a result of rigid internal fixation is possible and not unusual. Orthodontists’ experience in combined procedures started in 1985. Because patients no longer need to have their teeth wired together, nasal intubation during the orthognathic surgery may be changed to oral intubation. This opens the opportunity for simultaneous rhinoplasty to be performed, allowing dentists to produce greatly enhanced esthetic outcomes. Orthognathic surgery used to be considered a drastic procedure, but refinement of surgical efficiency (reducing the length of the procedure) and improvements in pre- and postoperative care has resulted in a comparatively uneventful postoperative recovery. Within 1 week, the patient was fully functional, although she had slight swelling.
Conclusion
Esthetic and cosmetic dentistry has expanded horizons and provided a greater vision than ever before. This requires an expanded diagnostic effort on dentists’ parts—a different direction of diagnosis and treatment planning.
References
1. Mamandras AH. Linear changes of the maxillary and mandibular lips. Am J Orthod Dentofacial Orthop. 1988;94(5):405-410.
2. Nanda RS, Meng H, Kapila S, et al. Growth changes of the soft tissue profile. Angle Orthod. 1990;60(3):177-190.
3. Formby WA, Nanda RS, Currier GF. Longitudinal changes in the adult facial profile, Am J Orthod Dentofacial Orthop. 1994;105(5):464-476.
4. Thilander B, Odman J, Lekholm U. Orthodontic aspects of the use of oral implants in adolescents: a 10-year follow-up study. Eur J Orthod. 2001;23(6):715-731.
5. Bernard JP, Schatz JP, Christou P, et al. Long-term vertical changes of the anterior maxillary teeth adjacent to single implants in young and mature adults. A retrospective study. J Clin Periodontol. 2004;31(11):1024-1028.
6. Behrents RG. Growth in the Aging Craniofacial Skeleton: Craniofacial Growth Series. Ann Arbor, MI: University of Michigan; 1985.
7. Dickens S, Sarver DM, Proffit WR. The dynamics of the maxillary incisor and the upper lip: a cross-sectional study of resting and smile hard tissue characteristics. World J Orthod. 2002;3:313-320.
8. Vig RG, Brundo GC. Kinetics of anterior tooth display. J Prosthet Dent. 1978;39(5):502-504.
About the Author
David M. Sarver, DMD, MS
Adjunct Professor
Department of Orthodontics
University of North Carolina at Chapel Hill School of Dentistry
Chapel Hill, North Carolina
Private Practice
Vestavia Hills, Alabama