You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Developmental disturbances of dentition encompass a broad range of disorders and affect its size, shape, structure, number, and growth.1 Pediatric dental patients with any of these developmental disturbances present with challenging esthetic, functional, and psychological needs.1,2 Ectodermal dysplasia (ED) has been well documented in the dental literature,1-3 which shows an incidence of about 7 per 10,000 live births.4,5 The condition is marked by a developmental deficiency of hair, sweat glands, nails, teeth, and other ectodermal structures.1-4 Hypodontia is the second most common complication and affects approximately 80% of patients.6-8 As a result of hypodontia, or anodontia, the alveolar bone is hypoplastic and the alveolus does not develop; however, normal growth occurs in the jaws and face.3,7
All of the above contribute to reduced occlusal vertical dimension (OVD).2,8 Therefore, removable prosthodontics is required for the growing child and has been reported to be the most common form of prosthodontic intervention.3 This is generally comprised of conventional complete dentures, complete overdentures, or partial dentures.1-3,8 It has been recommended that the earliest age for prosthodontic intervention should be 2 to 3 years.2,4 It is well accepted that at these ages, children benefit from dental and psychological treatments.1,2,8,9
Complete dentures have been used successfully in numerous patients with ED.10-20 However, few reports have actually addressed the principles and guidelines of this therapeutic modality when applied to growing children. The child’s face and jaws are constantly growing and undergoing changes in dentition. Fabrication techniques for complete dentures in children are distinct from adults and require special attention. It is necessary to simplify the technique of fabricating complete dentures in children to promote better cooperation and ensure them a positive dental experience. A simplified method may encourage more dentists to treat these patients’ conditions. All these factors should be considered during fabrication in order to provide a prosthesis that is not only functional but also esthetic and age appropriate. The following guidelines can be incorporated in the fabrication of complete denture prosthesis for a growing child.
Complete Denture Principles in Children
Diagnostic Impressions
Making preliminary diagnostic impressions in a child can be challenging due to limited mouth opening and developing swallowing mechanisms.21 The smallest stock tray is usually needed. Previous reports have involved materials, such as type 2 impression compound (cake)14 and irreversible hydrocolloid.15,18 It has been recommended to make the mandibular impression and then the maxillary impression in order to decrease anxiety in a child.21 The authors suggest using irreversible hydrocolloid material mixed to a higher viscosity; this will not only help prevent aspiration of the impression material but also facilitate patients’ comfort because it sets faster. Accurate impressions with proper anatomic extensions are needed to fabricate a good custom tray, which will eventually help make a superior final impression.
Final Impressions
Different impression materials such as irreversible hydrocolloid,14 polysulfide rubber base,15 and vinyl polysiloxane16,18 have been described in the literature. The authors favor vinyl siloxane or polyether for border molding and as an impression material because these materials are cleaner and have the required accuracy, better working time, and a fast setting time.22 Some clinicians have used border molding techniques, using a warm green stick compound prior to making the final impression.14,15 Due to insufficient evidence, it can be argued that this technique has limited advantages for a child because of the requisite time, patient discomfort related to the procedure, and potential risk of thermal injury. All of these factors outweigh the advantages of this procedure. Furthermore, there will be a future need for a reline or remake of the prothesis to accommodate jaw growth.1,2
Jaw Relation Records
Obtaining accurate jaw relation records in a child is important and challenging. Heat-processed record bases are recommended because they provide superior stability, confirmation of the final retention, and easier adjustment of occlusion performed in the laboratory.23,24 Obtaining jaw relation records may be a challenge in overdenture patients who have any existing teeth underneath the record base. Reducing these teeth below the anticipated occlusal plane may be required in conjunction with elective endodontic therapy.8 A heat-processed base can aid in this procedure by allowing it to be trimmed to a minimal thickness while maintaining its strength.
The OVD in these patients is most often collapsed and needs to be restored to a clinically acceptable position.1,2 In a long-term follow-up of these patients, no temporomandibular joint disorder complications resulted from increasing the OVD.1 Conventional methods of analysis using esthetics, phonetics, freeway space, and swallowing have been suggested.1,25
Different materials have been used for centric relation records, such as impression compound and zinc oxide eugenol paste.14,15 It is desirable to use a fast-setting material to obtain this record in a child due to the limited attention span and cooperation. The authors recommend the use of a silicone-based material in children because of its simplicity of use and a faster setting time.22 Some clinicians have advocated using facebow transfer and protrusive records.15,16 Because of insufficient evidence, it can be argued that this procedure is unnecessary for pediatric dentures due to its limited advantages; furthermore, the procedure is cumbersome for the child. Making an inaccurate record may jeopardize the final outcome. An accurate centric relation record will suffice generally.
Teeth Selection and Teeth Arrangement
The anterior teeth selection process for a pediatric complete denture is critical for making the prosthesis appear as natural as possible. Pediatric denture teeth molds should be used rather than filing adult denture teeth to match the size of the primary teeth.16 This will ensure a proper esthetic result to match the patient’s age. Sometimes adult incisor teeth can be incorporated to simulate a mixed dentition. A technique of preparing customized primary teeth using casts from a child with normal dentate has also been described.14 Appropriate posterior teeth molds are selected based on the arch size and space availability. The denture teeth are set using the clinician’s choice of occlusal scheme. Lingualized and bilateral balanced occlusion schemes have been reported in the literature.15,16 There is no valid evidence to show if one specific occlusal scheme is superior. The authors recommend a monoplane occlusion due to its simplicity and freedom of mandibular movement for the growing child.
Considerations in teeth arrangement include arranging the teeth to harmonize with the patient’s age, face, and oral cavity. Lip projection is an important consideration in patients with ED because they often have protuberant lips.3,4,15-18 The record base should not be excessively thick in the labial flange region, and the arrangement of denture teeth should not increase lip projection. Spacing in the primary and mixed dentition is reported to be common in children.26-29 Attention must be paid to incorporating this spacing to make the prosthesis look natural and age appropriate. Failure to do so will make the child look much older, promote a sense of “being abnormal,” and may attract attention to the prosthesis. Incorporating an orthodontic arch wire in the denture prosthesis to simulate a “normal” appearance has also been advocated.30
Delivery and Follow-Up
If heat-processed bases were used, the delivery appointment is simplified because the fit would have been verified at the jaw relation appointment and the occlusion refined in the laboratory on the remount casts. Therefore, a clinical remount procedure is unnecessary. Any pressure spots can be rechecked using a thin layer of pressure-indicating paste, and the occlusion can be reconfirmed with a thin sheet of articulating paper. The parent and child should be educated about the changes in enunciation, mastication, and swallowing. The patient should be encouraged to use denture adhesives especially for the mandibular denture because its retention is generally insufficient due to the underdeveloped alveolar ridges. The child should be scheduled for an immediate follow-up 24 hours postoperatively and at 1 week. For subsequent postoperative visits, the clinician and parents should arrange for intervals of 3, 4, or 6 months.14-16 Delivering one denture at a time has been advocated to allow the child to adjust to each prosthesis.14 The clinician should be prepared for additional appointments and adjustments if this option is chosen.
Complications and Management
Caries: Overdenture patients with existing abutment teeth underneath the dentures need closer monitoring because of oral hygiene issues and dental caries risk.1 Use of topical fluoride and the dentures themselves as fluoride carriers have been recommended.31,32 The authors recommend prescribing a 0.4% stannous fluoride gel as an anticaries agent for overdenture pediatric patients. Patients and parents should be cautioned to avoid the swallowing of excess fluoride.
Tissue changes: Periodontal disease has not been reported as a complication of the abutment teeth.1 However, “dead spaces,” or the space beneath an ill-fitting denture and growing tissues, have been reported to cause inflammatory hyperplasia and epulis formation.1 Depending on the severity, this can be managed surgically and pharmaceutically. After treating the tissues, new dentures should be fabricated. The existing dentures will require a tissue conditioning material in the interim to restore tissue health. The patient should be encouraged to maintain proper oral hygiene.
Denture complications: Routine denture complications, such as wear of teeth and fracture of the base and teeth, can also occur in pediatric dentures.1 Of particular importance is the fracture of the mandibular denture at the midline due to its shape to accommodate the narrow anterior mandibular ridge. The acrylic resin in this region needs to be thick enough to resist fractures. The child’s dentures will need to be revised periodically to accommodate changes in growth or eruption of occasional abutment teeth. Based on a long-term follow-up of pediatric complete denture patients for 2 to 25 years, Vergo recommends relining a denture every 2 to 4 years and making a new denture every 4 to 6 years.1 These are broad guidelines, and clinicians should base their decisions on each patient.
Other Options for the Future
Parents of these patients should be educated about the future possibilities for dental implant placement, with the eventual goal of obtaining an implant-supported prosthesis. The literature is clear about the long-term success of dental implants in children.33-35 Various implant-based options shown to be successful in fully grown adult edentulous patients with ED range from overdentures,33,34,36 to complete fixed prostheses,2,33,35,37 to complete fixed prostheses using zygomatic implants.5,38
Application of Complete Denture Principles
The following case report shows the systematic application of the above-mentioned principles. A 5-year-old male who had received a diagnosis of hereditary hypohidrotic ED was presented by his mother, who stated that she wanted his teeth to appear normal for school (Figure 1 and Figure 2). On clinical and radiographic examinations, it was noted that the patient had anodontia in the mandible, only two erupted primary incisors in the maxilla, and three developing tooth buds in the maxillary anterior region. Alveolar bone was significantly deficient (Figure 3). The erupted maxillary incisors had the characteristic cone shape (Figure 4). The patient presented with a knife-edge shaped mandibular residual ridge and significant xerostomia (Figure 5). After evaluating the patient’s financial, social, and oral status, the authors developed a treatment plan that involved fabrication of maxillary and mandibular complete dentures. It was decided to perform endodontic therapy on the two maxillary incisors and reduce them to the gingival level for their use as overdenture abutments. The root canals were filled with silver amalgam up to 3 mm inside the canal space (Figure 6).
The prosthodontic treatment appointments incorporated all of the principles discussed in this article and consisted of the following:
1. Diagnostic impressions were created using irreversible hydrocolloid impression material employing the smallest stock tray. Custom trays were fabricated in autopolymerizing resin.
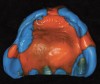
2. Using a heavy-body vinyl polysiloxane material for border molding and light-body vinyl polysiloxane material for the tissue surface, maxillary and mandibular final impressions were made without any complications (Figure 7 and Figure 8).
3. Heat-processed bases were fabricated on the master casts (Figure 9 and Figure 10). The bases were tried in the mouth and closely adapted to the tissues using pressure-indicating paste and acrylic burs. The maxillary base exhibited excellent retention and stability while the mandibular base had moderate retention and good stability. Occlusal rims were fabricated chairside, and the appropriate OVD was determined. A fox plane was used to confirm the occlusal plane, and the centric jaw relation was recorded using a silicone-based bite registration material.
4. Remount casts were poured into the heat-processed bases, and the casts were mounted on a semi-adjustable articulator. Pediatric mold denture teeth (Bambino Teeth®, Major Prodotti Dentari, www.majordental.com) were chosen, and the teeth were arranged incorporating minor spacing to simulate the natural dentition of a 5-year-old child (Figure 11). The trial bases were tried in the patient’s mouth. Esthetics, OVD, and centric relation records were confirmed. The patient and his mother evaluated and approved the teeth setup.
5. The dentures were fabricated in heat-processed acrylic resin. The dentures were placed on the mounted casts on the articulator. Occlusion was refined, and the dentures were finished and polished. The dentures were delivered to the patient, and pressure spots were rechecked and adjusted using pressure-indicating paste (Figure 12).
The patient and his mother were educated about the maintenance and follow-up of the prosthesis. The mother was instructed to have her child initially wear it a few hours a day to adjust to the new prosthesis. The mother was told to use 0.4% topical stannous fluoride on the remaining two maxillary anterior teeth, employing the denture as a fluoride carrier. Denture adhesive was also suggested. Recall appointments were scheduled for 24-hour, 1-week, and 3-month intervals. At a 3-month recall, the patient’s mother reported his excellent acclimatization to the prosthesis and improvements in his mastication, speech, and social attitude. The patient and his mother were pleased with the outcome of the prosthesis (Figure 13 through Figure 15).
Summary
Complete dentures are a simple, inexpensive, and reversible prosthodontic option. This clinical report analyzed the literature for complete denture principles and techniques in children and supports a simplified yet scientific approach in adopting these principles. There is a lack of evidence of one technique being superior; thus, a simplified approach is necessary. This will perhaps encourage more dentists to treat these patients. The principles described in this article can assist the clinician in using this simple therapeutic option to provide esthetic, functional, and psychological benefits for children and thus contribute to their overall development and well being.
References
1. Vergo TJ Jr. Prosthodontics for pediatric patients with congenital/developmental orofacial anomalies: a long-term follow-up. J Prosthet Dent. 2001;86(4):342-347.
2. Hickey AJ, Vergo TJ Jr. Prosthetic treatments for patients with ectodermal dysplasia. J Prosthet Dent. 2001;86(4):364-368.
3. Pigno MA, Blackman RB, Cronin RJ Jr, et al. Prosthodontic management of ectodermal dysplasia: a review of the literature. J Prosthet Dent. 1996;76(5):541-545.
4. National Foundation for Ectodermal Dysplasias Web site. http://www.nfed.org. Accessed April 27, 2009.
5. Balshi TJ, Wolfinger GJ. Treatment of congenital ectodermal dysplasia with zygomatic implants: a case report. Int J Oral Maxillofac Implants. 2002;17(2):277-281.
6. Holbrook KA. Structural abnormalities of the epidermally derived appendages in skin from patients with ectodermal dysplasia: insight into developmental errors. Birth Defects Orig Artic Ser. 1988;24(2):15-44.
7. Martin JW, Tselios N, Chambers MS. Treatment strategy for patients with ectodermal dysplasia: a case report. J Clin Pediatr Dent. 2005;29(2):113-118.
8. Hickey AJ, Salter M. Prosthodontic and psychological factors in treating patients with congenital and craniofacial defects. J Prosthet Dent. 2006;95(5):392-396.
9. Macgregor FC. Social and psychological implications of dentofacial disfigurement. Angle Orthod. 1970;40(3):231-233.
10. Hickey A, Vergo TJ Jr. Prosthodontic consideration in the treatment of patients with maxillary and mandibular deficiencies. J Prosthet Dent. 1991;66(5):645-649.
11. Bolender CL, Law DB, Austin LB. Prosthodontic treatment of ectodermal dysplasia: a case report. J Prosthet Dent. 1964;14(2):317-325.
12. Cruz R, Almeida M, Balassiano D, et al. Dental treatment of hydrotic hereditary ectodermal dysplasia. J Pedod. 1981;5(4):333-344.
13. Boj JR, Duran von Arx J, Cortada M, et al. Dentures for a 3-year old child with ectodermal dysplasia: case report. Am J Dent. 1993;6(3):165-167.
14. Ramos V, Giebink DL, Fisher JG, et al. Complete dentures for a child with hypohidrotic ectodermal dysplasia: a clinical report. J Prosthet Dent. 1995;74(4):329-331.
15. Bonilla ED, Guerra L, Luna O. Overdenture prosthesis for oral rehabilitation of hypohidrotic ectodermal dysplasia: a case report. Quintessence Int. 1997;28(10):657-665.
16. NaBadalung DP. Prosthodontic rehabilitation of an anhidrotic ectodermal dysplasia patient: a clinical report. J Prosthet Dent. 1999;81(5):499-502.
17. Paschos E, Huth KC, Hickel R. Clinical management of hypohidrotic ectodermal dysplasia with anodontia: case report. J Clin Pediatr Dent. 2002;27(1):5-8.
18. Tarjan I, Gabris K, Rozsa N. Early prosthetic treatment of patients with ectodermal dysplasia: a clinical report. J Prosthet Dent. 2005;93(5):419-424.
19. Vieira KA, Teixeira MS, Guirado CG, et al. Prosthodontic treatment of hypohidrotic ectodermal dysplasia with complete anodontia: case report. Quintessence Int. 2007;38(1):75-80.
20. Açikgöz A, Kademoglu O, Elekdag-Türk S, et al. Hypohidrotic ectodermal dysplasia with true anodontia of the primary dentition. Quintessence Int. 2007;38(10):853-858.
21. Kaakko T, Horn MT, Weinstein P, et al. The influence of sequence of impressions on children’s anxiety and discomfort. Pediatr Dent. 2003;25(4):357-364.
22. Anusavice KJ. Phillips’ Science of Dental Materials. 10th ed. Philadelphia, PA: Saunders; 2002:157-168.
23. Brewer AA. Prosthodontic research in progress at the school of aerospace medicine. J Prosthet Dent. 1963;13:49-69.
24. Jacob RF, Yen TW. Processed record bases for the edentulous maxillofacial patient. J Prosthet Dent. 1991;65(5):680-685.
25. Turrell AJ. Clinical assessment of vertical dimension. J Prosthet Dent. 1972;28(3):238-245.
26. el-Nofely A, Sadek L, Soliman N. Spacing in the human deciduous dentition in relation to tooth size and dental arch size. Arch Oral Biol. 1989;34(6):437-441.
27. Lux CJ, Dücker B, Pritsch M, et al. Space conditions and prevalence of anterior spacing and crowding among nine-year-old schoolchildren. J Orthod. 2008;35(1):33-42.
28. da Silva LP, Gleiser R. Occlusal development between primary and mixed dentitions: a 5-year longitudinal study. J Dent Child (Chic). 2008;75(3):287-294.
29. Janiszewska-Olszowska J, Stepien P, Syrynska M. Spacing in deciduous dentition of Polish children in relation to tooth size and dental arch dimensions. Arch Oral Biol. 2009;54(5):397-402.
30. Cronin RJ Jr, Oesterle LJ. Implant use in growing patients. Treatment planning concerns. Dent Clin North Am. 1998;42(1):1-34.
31. Toolson LB, Smith DE. A five-year longitudinal study of patients treated with overdentures. J Prosthet Dent. 1983;49(6):749-756.
32. Toolson LB, Taylor TD. A 10-year report of a longitudinal recall of overdenture patients. J Prosthet Dent. 1989;62(2):179-181.
33. Guckes AD, Scurria MS, King TS, et al. Prospective clinical trial of dental implants in persons with ectodermal dysplasia. J Prosthet Dent. 2002;88(1):21-25.
34. Kearns G, Sharma A, Perrott D, et al. Placement of endosseous implants in children and adolescents with hereditary ectodermal dysplasia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88(1):5-10.
35. Sweeney IP, Ferguson JW, Heggie AA, et al. Treatment outcomes for adolescent ectodermal dysplasia patients treated with dental implants. Int J Paediatr Dent. 2005;15(4):241-248.
36. Guckes AD, McCarthy GR, Brahim J. Use of endosseous implants in a 3-year-old child with ectodermal dysplasia: case report and 5-year follow-up. Pediatr Dent. 1997;19(4):282-285.
37. Lypka M, Yarmand D, Burstein J, et al. Dental implant reconstruction in a patient with ectodermal dysplasia using multiple bone grafting techniques. J Oral Maxillofac Surg. 2008;66(6):1241-1244.
38. Peñarrocha-Diago M, Uribe-Origone R, Rambla-Ferrer J, et al. Fixed rehabilitation of a patient with hypohidrotic ectodermal dysplasia using zygomatic implants. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98(2):161-165.
About the Authors
Avinash S. Bidra, BDS, MS, FACP, Assistant Professor and Maxillofacial Prosthodontist, Department of Prosthodontics, University of Texas Health Science Center, San Antonio, Texas
Jack W. Martin, DDS, MS, Professor and Program Director, Section of Maxillofacial Prosthodontics and Dental Oncology, University of Texas, MD Anderson Cancer Center, Houston, Texas
Elizabeth Feldman, DMD, MS, Staff Maxillofacial Prosthodontist, MD Anderson Cancer Center, Orlando, Florida