You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Purpose of Liners
Historically, liners have been used to protect the pulp. Although many materials have been used to do this, calcium hydroxide continues to be the liner of choice for direct and indirect pulp capping because of the belief that it can stimulate the formation of reparative dentin.2-4
However, calcium hydroxide has the drawback of being readily soluble and having low compressive strength. Because of the poor mechanical properties of calcium hydroxide, its use is restricted to areas not critical to the support of the restorations. Additionally, other pulp capping techniques are being used, like cohesive hybridization.5
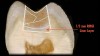
With the technological advances in dental materials, modern adhesive dentistry is using liners for additional purposes. Although bonded composite restorative filling materials have improved dramatically, they still have 1 major drawback: they contract or shrink during polymerization from about 2.0% to 3.5%. This creates 2 problems. The first problem is that the contraction forces can disrupt the union between the restoration, bonded layer, and tooth (Figure 1), forming a gap that can be colonized by bacteria and cause irritation to the pulp and possibly stimulate recurrent decay.6,7 A liner with strong adhesion characteristics, good mechanical integrity, and a lower modulus of elasticity (more elastic) may be used to counteract this shrinkage. This substrate can become a buffer and absorb some of the contraction stress, diminishing the gap formation and microleakage8,9 (Figure 2).
The second major consequence of polymerization shrinkage is the cusp deflection, or deformation, especially in cavities with a high “C” factor,9,10 which is believed to be one of the causes of postoperative sensitivity, especially related to chewing.11 Because of their low modulus of elasticity and dentin adhesion, liners can be used to counterbalance the cusp deformation (Figure 3).
Liner Materials
In modern adhesive dentistry, using a cavity liner appropriately can minimize some of the most troublesome problems with direct posterior composites. This leads to the question: What is the best material for this purpose? Although there are several materials that can be used as liners, only 2 types of materials—low viscosity (flowable) composites and light-cured resinmodified glass ionomers (RMGIs)—will be discussed in this article. Both materials provide predictable adhesion to tooth structure and restorative materials, strength, flexibility, and reliability.8,9
With regard to adhesion, the liner must not allow the polymerization contraction forces to create a de-bonding, or gap, between itself and the tooth or composite interface. Flowable composites attain their adhesion by a resin bonding agent, whereas RMGI liners are selfadhesive and do not require an additional bonding step. Table 1 shows that the combination of flowable composites and a bonding system provides predictable adhesion, but high polymerization shrinkage. RMGI has low shrinkage, but it also has lower adhesion than the flowable composites.

Another desirable characteristic of modern liners is a low modulus of elasticity, which allows these materials to act as a stress-absorbing buffer for the polymerization contraction forces of a restorative composite, decreasing the chances of gap formation, cuspal deformation, postoperative pain, and recurrent decay. RMGI materials have a low modulus of elasticity (Table 1). They also have a dual-setting reaction—a light-activated, methacrylate cross-linking reaction, and a slower, delayed, acid-base reaction that gives RMGIs an additional period of maximum flexibility12 to absorb stress from the adjacent shrinking composite. As the RMGI matures, through the acid-base reaction, it builds enough strength to support the restoration. RMGIs can also compensate for their polymerization shrinkage by their controlled hygroscopic expansion,13 which occurs after full polymerization in a humid environment. Flowable composites’ modulus of elasticity is considerably higher than RMGIs’ (Table 1), making them less effective at counteracting the shrinkage of the restorative materials. Also, the higher polymerization shrinkage makes them less effective than RMGIs in preventing cusp deformation.9
Flowable resin composites have a higher adhesion to dentin (Table 1), but a bonding system is required to achieve the adhesion. If the liner is going to be placed under deep dentin, the acid conditioning required for the,bonding system may cause sensitivity. RMGIs are self-adhesive and do not require an additional conditioner or adhesive to achieve an acceptable adhesion to dentin.
Two additional characteristics of RMGIs are fluoride release and coefficient of thermal expansion. Fluoride release is very valuable.14-16 Released fluoride ions have been shown to be incorporated into tooth structure,14,17 thus strengthening it. It also has been shown that lost fluoride ions can be recharged into the RMGIs from external sources such as fluoride gels, dentifrices, and fluoridated water, so that these “smart” materials act as fluoride reservoirs.18 This may not be of any clinical value unless the RMGI is exposed to the oral environment as in the “open sandwich” technique. The benefit of RMGIs in preventing secondary demineralization also has been reported in a number of studies.19,20 Additionally, RMGI liners such as Vitrebond, 3M, or Fuji Liner LC, GC America Inc.,have been shown to provide considerable antimicrobial activity.21,22
Second, RMGIs feature a coefficient of thermal expansion that is similar to a natural tooth. This means that RMGIs and teeth expand and contract at a similar rate at varied temperatures, decreasing the potential for microleakage.12,13,23
Clinically, RMGIs and flowable composites have shown superior performance when compared with composite restorations without a liner. The literature indicates good but inconsistent results with low-viscosity composite liners. For example, Unlu24 showed better results using a low viscosity composite liner under a condensable composite, than when using no liner. Swift25 reported a decrease in microleakage using an intermediate low-viscosity resin, and Turner26 showed no difference in results with or without a composite liner. Montes8 reported that a layer of low-viscosity resin liner significantly improved the marginal quality with a self-etch bonding system but had no effect with a total-etch system.
On the other hand, the literature also shows good, consistent results when using light-cured RMGIs as a liner. Tolidis12 demonstrated reduced volumetric polymerization contraction under a variety of light-cured composites when a RMGI liner was used. Powell23 compared the clinical performance of a composite with and without an RMGI liner and found 100% retention of the RMGI-lined restorations (in this case Vitrebond), and 76% retention for those not lined with a RMGI. Alomari9 compared in vitro cusp deflection between composite liners and Vitrebond RMGI liners and found the restorations with RMGI liners performed better than low-viscosity resin liners. Aboushala27 compared in vitro microleakage of composite restorations without liners and with GI liners and concluded that the application of light-cured GI liners up to the cavosurface margin inhibited microleakage. Miller28 came to a similar conclusion. Based on the provided information, the protocol for a deep class I or class II composite resin restoration may benefit by including the use of an RMGI liner.
Clinical Application
The use of RMGI under deep and high “C” factor cavities on class I and class II composite restorations makes sense for several reasons. Although some clinical studies have shown that under ideal clinical conditions postoperative sensitivity can be controlled with technique alone, under normal clinical conditions, the author’s experience has shown that the use of RMGI liners dramatically decreases sensitivity regardless of the bonding system used.29-31 Clinical use of RMGIs has several advantages. It is less technique-sensitive than many bonding systems, which decreases the chance of sensitivity caused by incorrect bonding. It decreases gap formation and cusp deformation caused by polymerization shrinkage, and also, in this era of conservative dentin removal, fluoride release has an antimicrobial activity that reinforces dentin. By using RMGI and a layering technique, the effects of composite shrinkage can be decreased (Figure 4).
Experienced clinicians are familiar with the advantages of using flowable composite to fill the first 1 mm of the proximal box. When the margin of the restoration is on enamel, flowable composite may be the most desirable material because of its ease of use.32 When the margin is on dentin or cementum, filling the first 1 mm with a RMGI using the sandwich technique (Figure 5) may dramatically decrease the chances of microleakage and decay.28,29,33,34 When the RMGI needs to be extended to the cavosurface margin, a restorative grade RMGI should be used because of its higher compressive strength.
Conclusion
Although improvement has occurred in the field of dental adhesives and composites, problems with composite restorations still exist. The most serious problem is polymerization shrinkage, which causes gap formation and cusp deflection. Both of these problems show clinically as postoperative sensitivity and pain. Based on the review of available articles, it appears that the use of liners is still desirable because liners may help overcome these problems. Both flowable resin composites and RMGIs have a lower modulus of elasticity than restorative composites, which may counteract some of the polymerization shrinkage of the restorative composites. Because of the low viscosity of RMGIs and flowable resin composites, they can wet the tooth better than restorative composites and decrease the chances of gaps. RMGI liners appear to perform better than flowable resin composites because of their physical properties.
Additionally, placing the self-adhesive RMGI liner on the areas of deep dentin can protect this sensitive dentin from the strong conditioners needed for the subsequent bonding procedure. From the clinician’s standpoint, overcoming these problems translates into less postoperative sensitivity.
Disclosure
Dr Sumita Mitra is corporate scientist in the 3M ESPE Dental Products Laboratory and is in charge of new materials/products research and development.
References
1. Anusavice KJ, Phillips RW. Phillips’ Science of Dental Materials. 11th ed. Philadelphia: WB Saunders Co; 2003:459.
2. Aschheim KW, Dale BG. Esthetic Dentistry: A Clinical Approach to Techniques and Materials. 2nd ed. St. Louis: Mosby;2001:74.
3. Barthel CR, Rosenkranz B, Levenberg A, et al. Pulp capping of carious exposures: treatment outcome after 5 and 10 years: a retrospective study. J of Endod. 2000;26:525-528.
4. Bergenholtz G, Spangberg L. Controversies in endodontics. Crit Rev Oral Biol Med. 2004;15:99-114.
5. Cox CF, Suzuki S. Re-evaluating pulp protection: calciumhydroxide vs. cohesive hybridization. J Am Dent Assoc. 1994;125:823-831.
6. Leinfelder K. Posterior composite resins: the materials and their clinical performance. J Am Dent Assoc. 1995;126:663-664, 667-668, 671-672.
7. Davidson CL, de Gee AJ, Feilzer A. The competition between the composite-dentin bond strength and the polymerization contraction stress. J Dent Res. 1984;63:1396-1399.
8. Montes MA, deGoes MF, Ambrosano GM, et al. The effect of collagen removal and the use of a low-viscosity resin liner on marginal adaptation of resin composite restorations with margins in dentin. Oper Dent. 2003;28:378-387.
9. Alomari QD, Reinhart JW, Boyer DB. Effect of liners on cusp deflection and gap formation in composite restorations. Oper Dent. 2001;26:406-411.
10. McCullock AJ, Smith BG. In vitro studies of cuspal movement produced by adhesive restorative materials. Br Dent J. 1986;161:405-409.
11. Carvalho RM, Pereira JC, Yoshiyama M, et al. Review of polymerization contraction: the influence of stress development versus stress relief. Oper Dent. 1996;21:17-24.
12. Tolidis K, Nobecourt A, Randall RC. Effect of a resin-modified glass ionomer liner on volumetric polymerization shrinkage of various composites. Dent Mater. 1998;14:417-423.
13. Leinfelder KF, Freedman G, Pakroo J. Postoperative sensitivity: bonded cavity liners revisited. Dent Today. 2001;20:82-87.
14. Mitra SB. In vitro fluoride release from a light-cured glassionomer liner/base. J Dent Res. 1991;70:75-78.
15. Strickland S, Retief DH, Russell CM. Shear bond strengths to dentin and fluoride release from fluoride-containing liners. Am J Dent. 1990;3:259-263.
16. Momoi Y, McCabe JF. Fluoride release from light-activated glass ionomer restorative cements. Dent Mater. 1993;9:151-154.
17. Mukai M, Ikeda M, Yanagihara T, et al. Fluoride uptake in human dentine from glass-ionomer cement in vivo. Arch Oral Biol. 1993;38:1093-1098.
18. Forsten L. Fluoride release and uptake by glass ionomers and related materials and its clinical effect. Biomaterials. 1998;19:503-508.
19. Donly KJ, Segura A, Kanellis M, et al. Clinical performance and caries inhibition of resin-modified glass ionomer cement and amalgam restorations. J Am Dent Assoc. 1999;130:1459-1466.
20. McComb D, Erickson RL, Maxymiw WG, et al. A clinical comparison of glass ionomer, resin-modified glass ionomer and resin composite restorations in the treatment of cervical caries in xerostomic head and neck radiation patients. Oper Dent. 2002;27:430-437.
21. Scherer W, Lippman N, Kaim J, et al. Antimicrobial properties of VLC liners. J Esthet Dent. 1990;2:31-32.
22. Palenik CJ, Behnen MJ, Setcos JC, et al. Inhibition of microbial adherence and growth by various glass ionomers in vitro. Dent Mater. 1992;8:16-20.
23. Powell LV, Johnson GH, Gordon GE. Factors associated with clinical success of cervical abrasions/erosion restorations. Oper Dent. 1995;20:7-13.
24. Unlu N, Krakaya S, Özer F, et al. Reducing microleakage in composite resin restorations: an in vitro study. Eur J Prosthodont Rest Dent. 2003;11:171-175.
25. Swift EJ Jr, Triolo PT Jr, Barkmeier WW, et al. Effect of low-viscosity resin on the performance of dental adhesives. Am J Dent. 1996;9:100-104.
26. Turner EW, Shook LW, Owens BM. Microleakage of flowable composite resin when utilized as liners in Class II posterior composite resin restorations. J Tenn Dent Assoc. 2002;82:23-26.
27. Aboushala A, Kugel G, Hurley E. Class II composite resin restorations using glass-ionomer liners: microleakage studies. J Clin Pediatr Dent. 1996;21:67-70.
28. Miller MB, Castellanos IR, Vargas MA. Effect of restorative materials on microleakage of Class II composites. J Esthet Dent. 1996;8: 107-113.
29. Crag RG. Restorative Dental Materials. 10th ed. St. Louis, MO: Mosby – Year Book, Inc; 1997:200.
30. Clinical Research Newsletter. 1999;23:1.
31. Perdigao J, Geraldeli S, Hodges JS. Total-etch versus selfetch adhesives: effect on postoperative sensitivity. J Am Dent Assoc. 2003; 134:1621-1629.
32. Moon PC, Tabassian MS, Culbreath TE. Flow characteristics and film thickness of flowable resin composites. Oper Dent. 2002;27:248-253.
33. Hewlett ER, Mount GJ. Glass ionomers in contemporary restorative dentistry—a clinical update. J Calif Dent Assoc. 2003;31:483-492.
34. Itota T, Nakabo S, Iwai Y, Konishi N, et al. Inhibition of artificial secondary caries by fluoride-releasing adhesives on root dentin. J Oral Rehabil. 2002;29:523-527.
About the Authors
Jose-Luis Ruiz, DDS, FAGD, Clinical Instructor, Division of Primary Oral Health, University of Southern California School of Dentistry, Los Angeles, California
Sumita Mitra, PhD, Corporate Scientist, 3M ESPE Dental Laboratory, St. Paul, Minnesota