You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
A dilemma faced by many clinicians is how and when to choose between conventional and surgical re-treatment. Modern endodontic therapy can achieve success predictably. But even when initial nonsurgical root canal treatment is performed to the highest standard of care, the need for re-treatment can occur. The reasons for treatment failure can be multivalent. The most common reason for true endodontic failure is the presence of microorganisms. Procedural errors such as root perforations, separated instruments, missed canals, and anatomical difficulties (eg, calcified canals or root dilacerations) are also among the factors influencing the endodontic prognosis, and understanding these factors is essential for endodontic treatment planning.1,2
This article provides guidelines and criteria to consider when planning endodontic re-treatment versus surgical endodontics or extraction and subsequent placement of an implant.
Failure of Root Canal Therapy
Persistent Infection
Many re-treatments are performed because periapical pathology develops or persists after routine root canal therapy. It has been shown that the presence of bacteria within the root canal system at the time of obturation has a negative influence on the endodontic outcome.3 After biomechanical cleaning, bacteria may persist not only within the root canal system but also in the apical regions of roots, at the apical foramen, or within a periapical lesion, which leads to endodontic failure.4,5 The presence of bacteria in the periapical tissue does not imply periapical infection. The occurrence of bacteria in the periradicular tissue depends on a critical amount of bacteria within the root canal.6 In necrotic teeth with periapical pathology, bacterial flora become more complex, containing different species and a larger number of bacteria. Eliminating these microorganisms and healing become more difficult.
The nature of the apical periodontitis can influence the prognosis.7 Extraradicular infection may be found in symptomatic abscessed lesions, periapical actinomycosis, or infected radicular cysts. Most endodontic periapical lesions are inflammatory and not of infectious origin or of neoplastic nature. Approximately 80% of endodontic periradicular lesions can heal satisfactorily after proper root canal therapy. However, the size of the periapical lesions (>5 mm) appears to be a negative factor for the prognosis.8,9
The incidence of periapical cysts among all inflammatory periapical lesions is approximately 15% to 20%.10-12 Pocket cysts are connected to the root apex and the root canal; true cysts are separate and not attached. Neither type of cyst can be diagnosed clinically.10,12 Other than periapical granuloma or pocket cysts, true cysts, extraradicular infections, reaction to foreign bodies, or residual cholesterol crystals might not heal after conventional treatment. In that instance, surgery is indicated.3,10
Recurrent Infection
Even a previously completely debrided root canal system might be subject to reinfection. Most common causes are leaky restorations, ill-fitting crowns, or broken fillings as well as recurrent decay. The importance of an intact restoration after root canal therapy with regard to success and survival rates of endodontic therapy has been shown in several retrospective studies.1,13
Loss of endodontically treated teeth is caused by multiple types of failure, mainly prosthetic failure (59.4%) and periodontal failure (32%), but less frequently by endodontic failure (8.6%).14 After exposure of debrided and obturated root canal systems to artificial and natural saliva, significant coronal dye and bacterial leakage could be demonstrated. Dye penetration of teeth that were exposed to artificial saliva in vitro showed significant leakage after 3 days.15 In another study, all teeth that were sealed in vivo with temporary filling material and subsequently exposed to the oral cavity demonstrated leakage to dye penetration after extraction.16 Bacteria in natural saliva needed <30 days to repopulate the entire length of root canals obturated by lateral and vertical compaction.17 Coronal microleakage must be considered as an important possibility of endodontic failure. The significance of an intact coronal seal must be emphasized not only during obturation and for the final restoration, but also for temporary fillings.
In instances where coronal microleakage is obvious or suspected, a conventional re-treatment approach should be attempted at first to eliminate persistent or recurrent infection.
Inadequate Cleaning and Shaping
A clinician’s primary concern is to thoroughly clean the root canal system during root canal therapy. Advancements in endodontic instruments and techniques have improved the quality of biomechanical cleaning of root canals. New nickel-titanium rotary file systems and irrigation solutions have helped to clean canals faster and more predictably. These flexible and tapered files help to shape canals so that they are more centered and round.
In the course of cleaning and shaping the root canal system, the initial apical size of a canal dictates the final shaping size. It has been suggested to finalize the mechanical cleaning by enlarging the apical portion by 3 International Standards Organization (ISO) file sizes.18 The initial apical size is most commonly determined by gauging consecutively larger size files until 1 binds at the canal terminus. The accuracy of this measurement depends on the root canal morphology. Severe curvatures and irregular canal walls or canal shape limit the ability of the clinician to accurately determine the initial apical size. The purpose of apical enlargement, besides creating a space for obturation, is the mechanical debridement of remnant pulp tissue and infected dentin. Especially in infected necrotic and re-treatment cases, mechanical disinfection, in addition to chemical debridement, should be of concern to the clinician.
Many morphologic studies have shown that root canals are not round and have a wide range of diameters within the canal walls.19 In most roots, the canal diameter decreases apically, and the canal becomes rounder. The minor diameter of the apical constriction is about 270 µm to 330 µm. In other words, the first binding file should be size 25 to 35 (ISO).
Also, studies on apical cross sections (1-5 mm) revealed that most teeth have long oval canals and a buccolingual dimension that is wider than the mesiodistal dimension.19-21 In upper premolars and mesiobuccal canals of upper molars, the buccolingual diameter of the canal could be at least 2 times larger than the mesiodistal canal diameter.22
Taking into account morphology and bacterial contamination, an ideal preparation should be a maximal apical size, retaining the original shape of the canal. However, enlarging the apical terminus without excessively weakening the root dentin is challenging, considering the size of the minor diameter of the apical constriction (about 270-330 µm) and the original oval shape. The limitation on instrumentation may prevent an optimal result.22-25
Missed Canals
After removing the existing restoration and decay, an access opening to the root canals should be established. The pulp floor should be carefully inspected to locate all calcified or missed canals. Radiographically and clinically calcified canals may appear to be completely obliterated; however, histological canal space always exists.26 These missed or untreated canals contain necrotic tissue and bacteria contributing to the chronic symptoms and nonhealing periapical lesions.27 Knowledge of morphology, correct interpretation of radiographs, and careful examination under a microscope can help clinicians recognize anatomical variations, improving treatment quality of all canals.
Clinical Complications
Various procedural errors can happen during the treatment of the root canal system. Maximum effort should be made to prevent or correct such errors. Generally clinicians believe that procedural errors cause failure of the root canal treatment. Procedural errors often delay the progress of therapy or, in some situations, make it impossible to complete the course of treatment. Several studies have shown that factors such as underfilling, overfilling, root perforations, separated instruments, and ledge formations negatively affect the prognosis of root canal therapy. Separated instruments, ledge formations, or root perforations may prevent thorough cleaning and shaping of the canal system. Filling material extruded into the periapical tissue may induce inflammation including a foreign body reaction despite a clinical absence of pain.28
Decision Making in Failed Root Canal Therapy
The treatment options for root canal treated teeth with a questionable outcome include a regular follow-up, conventional re-treatment, surgical re-treatment, or a combination of conventional and surgical re-treatment. Every treatment plan should be created individually, and several questions should be asked before making a decision. It is not necessary to re-treat because of an unsatisfactory appearance on the radiograph only. If the patient is asymptomatic, no new restoration is planned, and the periapical condition could be healing or scar tissue, a regular follow-up might be advised. However, it is important to understand the factors responsible for the failure of the initial therapy to select the necessary treatment.
Modern endodontic surgery has evolved into endodontic microsurgery. With proper inclusion and exclusion criteria and facilitating up-to-date techniques such as the use of the dental microscope, ultrasonic root-end preparation, and the application of biologically compliant and stable filling materials (eg, mineral trioxide aggregate [MTA] or Super-EBA), the outcome of healing has become highly predictable. According to studies on endodontic microsurgery that followed these principles, the possible clinical success rate is around 90%.29
However, periradicular surgery, no matter how sophisticated or advanced, is not a substitute for conventional re-treatment. If the coronal and apical access is feasible through the current restoration and the canal space is accessible, maximum effort should be made for a conventional re-treatment. If an original treatment is inadequate (eg, shows poor obturation or missed canals) or the root canal system is contaminated by exposure to the intraoral environment, conventional re-treatment should be the treatment of choice.
Conventional vs Surgical Re-treatment
Two randomized controlled trials are available comparing conventional and surgical re-treatment. In the first study, the difference in success rate was not statistically significant after 1 year.29,30 The second trial showed a significantly (P<.05) higher healing rate for root-end surgery after 1 year but no difference after 4 years.31
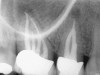
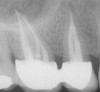
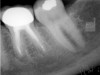
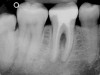
When a decision between a conventional and a surgical re-treatment needs to be made, clinicians should evaluate whether the existing condition necessitates damaging a successful restoration to gain orthograde access to the root canal system and if the restoration is intact or can be removed at all. Disassembly may not be reasonably safe and could lead to a nonrestorable situation. In some cases, it might be better to either access the root canal system through the restoration or more conservatively to consider surgical re-treatment. However, if a restoration is lost or coronal leakage exists, the restoration should be removed to clean out all sources of infection and to prevent a possible route of entry for bacteria into the root canal system. It is key to consider conventional re-treatment first in the case of existing leakage (Cases 1 and 2).
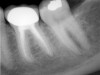
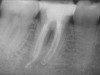
The quality of the obturation should be evaluated radiographically before treatment. Based on the authors’ experience, it is recommended to take multiple angulation radiographs to get maximum information on the root morphology and the previous treatment. The filling material may look dense or show voids. There may be signs of perforations, ledges, separated instruments, infected lateral canals, or internal or external resorption. The location of perforations can dictate the suggested treatment. Zipping or perforations at the apical level more likely cannot be repaired from inside the root canal system. If there are separated instruments or foreign objects, their location within the canal system dictates whether to retrieve or bypass the instrument. Clinicians must be familiar with techniques, instruments, and microscope use. If a separated object is beyond the canal curvature, conventional removal is not advised, but a surgical approach is preferred (Case 3).
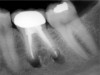
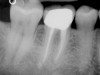
The number of previously treated canals might suggest a missed canal (Case 4). In Case 4, conventional re-treatment is indicated to eradicate bacteria and tissue remnants. The apical extension of the filling can appear too short or too long. When an overfilling is obvious, surgical treatment is often the successful approach if the condition of the root canal treatment cannot be significantly improved by conventional re-treatment. The suggested working length for teeth with periapical lesions is ≤1 mm from the radiographic apex, with the obturation material confined to the root canal space. Ending at or short of the apical constriction results in the most favorable histological condition.28 If patency cannot be achieved or transportations or ledges are present, the chances to clean out infection properly are minimized (Case 5).
Extraction Indications
An extraction of the tooth should be considered in cases of prosthetic failure, vertical or horizontal root fractures, severe periodontitis, severe mobility, or an insufficient tooth structure. Also, a poor prognosis of the overall treatment plan can necessitate extraction.
If an existing restoration has to be removed, it should be carefully assessed before treatment if the tooth is restorable at all. This includes assessing the amount of remaining tooth structure, possible fractures, the clinical crown-to-root ratio, and the periodontal condition. A total of 4.0 mm of biological width and restorative finish line with sufficient ferrule to enhance the resistance to root fracture should be given.32 If this cannot be established, even with crown lengthening or with orthodontic extrusion, the tooth is subject to extraction.
Conclusion
The key factors to consider are whether the fill of the root canal can be improved, it is likely that a canal was missed, the crown is leaking, access to the root canal system is possible, and the disassembly is reasonably safe. If all of these concerns are considered, the correct treatment choice can be made with the correct equipment available and the proper skills and experience. Conventional re-treatment should be the first treatment choice, except when a canal cannot be completely negotiated because of an apical or coronal obstruction or a re-treatment attempt has already failed. Conventional re-treatment is less invasive in most cases. Surgical treatment often can be performed after conventional re-treatment as the next step in treatment (Figure 6).
References
1. Salehrabi R, Rotstein I. Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study. J Endod. 2004;30:846-850.
2. Lin LM, Skribner JE, Gaengler P. Factors associated with endodontic treatment failures. J Endod. 1992;18:625-627.
3. Nair PN. Apical periodontitis: a dynamic encounter between root canal infection and host response. Periodontol 2000. 1997;13:121-148.
4. Nair PN, Sjögren U, Figdor D, et al. Persistent periapical radiolucencies of root-filled human teeth, failed endodontic treatments, and periapical scars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:617-627.
5. Ramachandran Nair PN. Light and electron microscopic studies of root canal flora and periapical lesions. J Endod. 1987;13:29-39.
6. Dahlen G. Microbiology and treatment of dental abscesses and periodontal-endodontic lesions. Periodontology 2000. 2002;28:206-239.
7. Sundqvist G. Taxonomy, ecology, and pathogenicity of the root canal flora. Oral Surg Oral Med Oral Pathol. 1994;78:522-530.
8. Strindberg LZ. The dependence of the results of pulp therapy on certain factors. An analytic study based on the radiographic and clinical follow-up examinations. Acta Odontol Scand. 1956;14:1-174.
9. Sundqvist G, Figdor D, Persson S, et al. Microbiologic analysis of teeth with failed endodontic treatment and the outcome of conservative retreatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:86-93.
10. Simon JH. Incidence of periapical cysts in relation to the root canal. J Endod. 1980;6:845-848.
11. Lin LM, Pascon EA, Skribner J, et al. Clinical, radiographic, and histopathological study of endodontic treatment failures. Oral Surg Oral Med Oral Pathol. 1991;71:603-611.
12. Ramachandran Nair PN, Pajarola G, Schroeder HE. Types and incidence of human periapical lesions obtained with extracted teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996:81:93-102.
13. Ray HA, Trope M. Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int Endod J. 1995;28:12-18.
14. Vire DE. Failure of endodontically treated teeth: classification and evaluation. J Endod. 1991;17:338-342.
15. Swanson K, Madison S. An evaluation of coronal microleakage in endodontically treated teeth. Part I. Time periods. J Endod. 1987;13:56-59.
16. Madison S, Wilcox LR. An evaluation of coronal microleakage in endodontically treated teeth. Part III. In vivo study. J Endod. 1988;14:455-458.
17. Torabinejad M, Ung B, Kettering JD. In vitro bacterial penetration of coronally unsealed endodontically treated teeth. J Endod. 1990;16:566-569.
18. Grossman LI. Endodontic Practice. 10th ed. Philadelphia, Pa: Lea & Febiger; 1981.
19. Kerekes K, Tronstad L. Morphometric observations on the root canals of human molars. J Endod. 1977;3:114-118
20. Gani O, Visvisian C. Apical canal diameter in the first upper molar at various ages. J Endod. 1999;25:689-691.
21. Jou YT, Karabucak B, Levin J, et al. Endodontic working width: current concepts and techniques. Dent Clin North Am. 2004;48:323-335.
22. Wu MK, R’oris A, Barkis D, et al. Prevalence and extent of long oval canals in the apical third. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:739-743.
23. Siqueira JF Jr. Endodontic infections: concepts, paradigms, and perspectives. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:281-293.
24. Kuttler Y. Microscopic investigation of root apexes. J Am Dent Assoc. 1955;50:544-552.
25. Love RM. Clinical management of infected root canal dentin. Pract Periodontics Aesthet Dent. 1996;8:581-584.
26. Kuyk JK, Walton RE. Comparison of the radiographic appearance of root canal size to its actual diameter. J Endod. 1990;16:528-533.
27. Wayman BE, Murata SM, Almeida RJ, et al. A bacteriological and histological evaluation of 58 periapical lesions. J Endod.1992;18:152-155.
28. Ricucci D, Langeland K. Apical limit of root canal instrumentation and obturation, part 2. A histological study. Int Endod J. 1998;31:394-409.
29. Rubinstein RA, Kim S. Long-term follow-up of cases considered healed one year after apical microsurgery. J Endod 2002;28:378-383.
30. Danin J, Stromberg T, Forsgren H, et al. Clinical management of nonhealing periradicular pathosis. Surgery versus endodontic retreatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:213-217.
31. Kvist T, Reit C. Results of endodontic retreatment: a randomized clinical study comparing surgical and nonsurgical procedures. J Endod. 1999;25:814-817.
32. Wagenberg BD. Surgical tooth lengthening: biologic variables and esthetic concerns. J Esthet Dent. 1998;10:30-36.
33. Friedman S, Stabholz A. Endodontic retreatment—case selection and technique. Part 1: Criteria for case selection. J Endod.1986;12:28-33.
AUTHORS
Bekir Karabucak, DMD, MS
Assistant Professor
Frank Setzer, DDS
Postgraduate Candidate
Department of Endodontics
University of Pennsylvania School of Dental Medicine
Philadelphia, Pennsylvania