You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
When a tooth has been lost, a modern, two-piece, endosteal implant can be placed to facilitate the replacement of the tooth's root and then restored with an implant abutment and crown. There are many factors for clinicians to consider in the design of single tooth implant restorations, including the material that will be used to fabricate the crown, the method by which the crown will be retained, the prosthetic components that will be used, and more. Each option comes with some distinct advantages and disadvantages. Although there are some scenarios in which a particular material or restoration type will generally yield superior results, there are also scenarios in which various approaches could be expected to perform comparably over the long term.
One of the most consequential decisions to be made in the restoration of an implant is the retention/fabrication design of the crown. In general, there are three options for single tooth implant-supported restorations: the cement-retained implant crown (Figure 1 through Figure 4), the screw-retained implant crown (Figure 5 through Figure 10), and a hybrid of the two, which is colloquially referred to as the "screwmentable" implant crown. Whether or not one of these types of restorations offers superior outcomes to the others is a frequently debated topic. This article reviews the current evidence related to the advantages and disadvantages of different types of single tooth implant-supported restorations.
Disambiguation of Retention Terminology
In its earliest forms, the cement-retained implant crown consisted of a stock titanium abutment that was screwed into the implant onto which a fabricated crown was cemented intraorally. Selection of an appropriate stock abutment commonly proved challenging when it came to balancing biologic and esthetic concerns. The use of inappropriately sized stock abutments for cement-retained crowns often led to margins that were far too deep subgingivally, which resulted in the potential for excess subgingival cement and cement-induced peri-implantitis. The modern evolution of the cement-retained implant crown most commonly uses a custom milled abutment with margins placed no deeper than 1 mm. It is hypothesized that the widespread use of custom milled abutments that result in appropriate margins has reduced the incidence of cement-induced peri-implantitis.
The classic version of the screw-retained implant crown is the custom-made screw-retained porcelain-fused-to-metal (PFM) crown that was first introduced to the profession in 1988 by a team from UCLA.1 This design generally relied on an abutment made of a waxing sleeve and a gold alloy base that the technician used to wax up a framework. After casting in gold alloy, feldspathic porcelain was usually layered on top to create the completed crown. The crown and the abutment were integral to each other and delivered as one unit. In recent years, this specific type of screw-retained restoration has fallen out of favor, seemingly as a result of the high cost of gold and the diminishing number of technicians trained in its fabrication.2
Regarding the screwmentable implant crown, there is not a yet a profession-wide consensus on the specifics of its fabrication; however, it does come in a few variants. It is generally agreed that the screwmentable implant crown has a screw access hole in the crown, which is made from a ceramic material that is cemented to an abutment. Although the cementation seems to be most often performed by the technician, some clinicians prefer to cement the crown to the abutment intraorally and then remove it briefly to eliminate the excess cured cement. Either way, the crown-abutment complex functions clinically like a traditional screw-retained crown. The primary differences are that the crown is usually zirconia or lithium disilicate instead of feldspathic porcelain and that it is mated to the abutment with cement. The abutment used in a screwmentable design can be either a stock abutment or a custom-milled abutment.
Ease of Delivery and Retrieval
When choosing a retention method for a single tooth implant restoration, clinicians should consider its impact on delivery and retrieval. The extent to which a restoration is easy to deliver is a relatively subjective concept and may differ based on the experience and preferences of clinicians and the abilities of their technicians. Furthermore, there are factors unique to the design of restorations that may contribute to their ease of deliverability.
Because the prosthetic components of screw-retained implant crowns connect directly to the implant, the delivery process may be more challenging. As a screw-retained implant crown is tried in and out to adjust the occlusion and interproximal contacts, the soft tissue may collapse or prevent complete seating of the implant crown. This can make the delivery process more time-intensive and frustrating for the clinician. Typically, the more subgingivally an implant is located, the more challenging the delivery process is. One means by which the delivery process can be made easier is through the use of a custom healing abutment or, at least, a large-diameter stock healing abutment. This can help to facilitate tissue retraction at the time of delivery.
The ease of delivery of a cement-retained implant crown is largely based on the location of the margins of the abutment. If the margins of the abutment are deeply subgingival, a design which involves other shortcomings that will be discussed later, the delivery process is hardly any easier than that of a screw-retained implant crown. This scenario will still result in the potential for soft tissue to hinder the complete seating of the crown to the abutment. Alternatively, if the abutment margins of a cement-retained implant crown are equigingival or supragingival, try-in and delivery becomes relatively straightforward, and the clinician does not have to be concerned with soft-tissue management or collapse. In essence, it would be an oversimplification to state that cement-retained implant restorations are easier to deliver than screw-retained ones.
The ease of retrieval of an implant crown becomes important in the event that the implant ever succumbs to a biologic or technical complication. With cement-retained implant crowns, removal without risking damage to the abutment or implant usually requires sacrificing the crown. However, implant crowns with screw-retained or screwmentable designs can be removed without sacrificing them. Simply uncovering the screw access channel permits them to be retrieved and subsequently redelivered when indicated.
Risk of Complications
The passage of time has enabled implants to be better understood and brought forward the understanding that they are not a perfect solution. Like all restorations, they too can experience complications and require follow-up and maintenance. Even with material improvements and advances in the designs of modern implants, research has shown that approximately 25% of implant-supported restorations exhibit prosthetic complications at 5 years.3
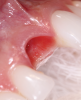
Peri-Implantitis
One example of a biologic complication that most practitioners are aware of is peri-implantitis. Peri-implantitis is to implants what periodontitis is to a natural tooth. It is a disease process that results in the loss of soft tissue and bone around an implant. Peri-implantitis, which has been reported to be the most common biologic complication associated with implant restorations as well as one of the most serious complications in implant dentistry, is challenging to treat. 4,5 Part of what makes it such an insidious disease process is that it is not self-limiting. Treatment for peri-implantitis is commonly described as "unpredictable." Although there are numerous approaches to treatment, no one intervention has consistently shown superiority over a combination of interventions. The treatment of peri-implantitis may involve mechanical debridement, implantoplasty, laser therapy, the use of chemical agents, and surgical interventions. Removal of the implant crown makes the treatment of peri-implantitis easier because the clinician has better access to the implant itself.
Screw Loosening
A common technical complication that implants succumb to is loosening of the prosthetic screw. Screw loosening is estimated to occur in approximately 7% to 12% of implants; therefore, it is important that clinicians who deliver implants have the knowledge base to recognize and treat the issue.6 Many cases of screw loosening can likely be traced back to inappropriate use of a torque wrench. According to Jemt and colleagues, screw loosening is the most common problem to arise within the first year of implant restoration,7,8 and Lee and colleagues reported that screw loosening is least common in the premolar region and most common in the molar region.6 When a prosthetic screw loosens, it can give rise to localized inflammation and screw or abutment fractures, and in some cases, the implant crown may become dislodged and the patient may swallow or aspirate it.9
Interestingly, although screw-retained restorations are easier to retrieve in the event that the screw becomes loose, research has indicated that the occurrence of screw-loosening is more common in screw-retained implant crowns.6 The possible reasons for this have not been fully flushed out; however, one likely factor is the presence of heavy interproximal contact, which results in the screw-retained restoration being fully torqued but incompletely seated on the implant. The extent of this may be minor and undetectable on radiographs. As the heavy contact places orthodontic-like forces on the adjacent natural tooth, it moves over time, diminishing the preload established in the screw and causing it to loosen.
Loss of Interproximal Contact
The loss of an interproximal contact between a single tooth implant restoration and a natural tooth has been reported to occur in 34% to 66% of cases and may occur as early as 3 months after delivery.10 It is slightly more common for this gap to occur on the mesial contact, in the mandible, and in smaller teeth.10-13 In addition to being a hygiene nuisance to the patient, open contacts can result in everything from unsightly black triangles to gingival inflammation, peri-implantitis, caries, attachment loss and more.
If a contact does open between an implant crown and an adjacent tooth, the clinician has the opportunity to add more restorative material to the interproximal contact. One means by which this can be accomplished is to bond composite resin to the ceramic crown to add to the contact. In some scenarios in which the implant crown can be retrieved, the abutment can be separated from the crown in a porcelain furnace and more porcelain can be added to the interproximal area to recreate a contact. This is accomplished by placing the cemented implant restoration in a furnace for 5 minutes at a holding temperature of 350°C under no vacuum.14 Alternatively, the implant crown may be replaced with a new one or a restoration may be placed on the adjacent tooth. Orthodontics may also be a viable option to reconcile the open contact. Because prevention is key to avoid the need for such treatment, patients receiving implant restorations should be encouraged to use some sort of retention device or occlusal guard. This will slow down the process that leads to open contacts. In the anterior maxilla, continued movement of the natural dentition adjacent to implants commonly leads to the implant crowns appearing to shorten over time.
Risk of Failure
In a 2014 systematic review that evaluated the risk of failure of cement-retained and screw-retained implant crowns, the authors reported that there was no statistically significant difference between the failure rates of the reconstruction types.8 It should, however, be noted that the metric of implant failure cannot be equated to implant success. Wittneben and colleagues also noted that although the failure rate of cemented reconstructions was not influenced by the choice of a specific cement, cement type did influence loss of retention. The different types of cements evaluated were eugenol or phosphate-based cements, resins, and glass ionomer cements. This finding is interesting because retained resin-based cements have been implicated in implant failure because laboratory data has suggested that they may be cytotoxic.15
Restorative and Prosthetic Considerations
For screw-retained and screwmentable implant crowns, the ability to effectively conceal the screw access channel may be of concern, particularly if the access channel is in the anterior esthetic zone. An implant reconstruction may be considered an esthetic failure if the screw access channel is positioned on the facial surface of the crown. If the necessary implant position and angulation will result in a reconstruction with a screw access channel positioned on the facial surface of the implant crown, a cement-retained implant crown with a custom abutment may be the best solution. Alternatively, there are more recently developed systems of prosthetic components that enable implant crown designs with angulated screw channels to correct for facial positioning of the access.
Angulated screw channel solutions provide clinicians with the opportunity to reposition the screw access hole (Figure 11). Traditionally, the access hole of an implant crown had to be 0° from the long access of the implant crown. Angulated screws enable the access hole to be positioned as far as 25° from the long access.16 In one retrospective study, the researchers found that screw-retained implant restorations with angulated screw channels demonstrated a success rate of 94%.17 This success rate may be strikingly similar to that of implant crowns that do not utilize angulated screw channels.18
The ability to design implant crowns with angulated screw channels may give clinicians the opportunity to make every anterior implant crown screw-retained if they so choose. Nonetheless, a potential complication associated with angulated screw channel solutions may be a risk of future screw loosening or debonding of the crown resulting from the relatively short abutments they employ. In addition, the nature of the gear system utilized to torque down the screws used in angulated screw channel solutions may result in a loss of torque transmission to the screw. Although there is variability in the literature on this topic, this outcome ultimately causes the screw to receive less preload, which can make it more vulnerable to loosening. Angulations beyond 15° may be the most vulnerable.19
There is, however, a dearth of clinical research evaluating the success and survival of the various angulated screw systems, and their success is likely to vary based on the designs of their manufacturers. Additional challenges may present over time for clinicians because these systems require an entirely unique driver that is less common in practice, and that may not be evident from records or radiographs.
Conclusion
The success and survival of single tooth implant reconstructions, whether cement-retained, screw-retained, or screwmentable, is largely dependent on the design of the restoration, the material selection, the knowledge and skill of the clinician and technician, and case-specific factors. There is not one type of implant-supported restoration that is superior to all of the others in all clinical scenarios. Clinicians and technicians should be mindful in selecting the most appropriate restoration for each case based on the needs of the site being treated and the desires of the patient.
Queries regarding this course may be submitted to authorqueries@conexiant.com
About the Authors
Melissa Seibert, DMD, MS
Diplomate
American Board of General Dentistry
Creator and Host
Dental Digest Podcast
US Air Force Dentist
Langley Air Force Base
Hampton, Virginia
Clinical Instructor
Creighton University
School of Dentistry
Omaha, Nebraska
Todd R. Schoenbaum, DDS, MS
Professor of Restorative Sciences
Coordinator of Clinical Education in Implant Dentistry
Dental College of Georgia
Augusta University
Augusta, Georgia
References
1. Lewis S, Beumer III J, Hornburg W, Moy P. The" UCLA" abutment. Int J of Oral Maxillofac Implants. 1988;3(3):183-189.
2. Schoenbaum TR, Papaspyridakos P, Kim YK, et al. Clinician preferences for single-unit implant restoration designs and materials: a survey of the membership of the Pacific Coast Society for Prosthodontics. J Prosthet Dent. 2023;S0022-3913(23)00116-6.
3. Pjetursson B, Asgeirsson A, Zwahlen M, Sailer I. Improvements in implant dentistry over the last decade: comparison of survival and complication rates in older and newer publications. Int J Oral Maxillofac Implants. 2014;29(Suppl):308-324.
4. Jung RE, Pjetursson BE, Glauser R, et al. A systematic review of the 5-year survival and complication rates of implant-supported single crowns. Clin Oral Implants Res.2008;19(2):119-130.
5. Rokaya D, Srimaneepong V, Wisitrasameewon W, et al. Peri-implantitis update: risk indicators, diagnosis, and treatment. Eur J Dent.2020;14(4):672-682.
6. Lee KY, Shin KS, Jung JH, et al. Clinical study on screw loosening in dental implant prostheses: a 6-year retrospective study. J Korean Assoc Oral Maxillofac Surg. 2020;46(2):133-142.
7. Jemt T, Laney WR, Harris D, et al. Osseointegrated implants for single tooth replacement: a 1-year report from a multicenter prospective study. Int J Oral Maxillofac Implants. 1991;6(1):29-36.
8. Wittneben JG, Millen C, Brägger U. Clinical performance of screw- versus cement-retained fixed implant-supported reconstructions--a systematic review. Int J Oral Maxillofac Implants.2014;29(Suppl):84-98.
9. Zarb GA, Schmitt A. The longitudinal clinical effectiveness of osseointegrated dental implants: the Toronto study. Part III: problems and complications encountered. J Prosthet Dent.1990;64(2):185-194.
10. Greenstein G, Carpentieri J, Cavallaro J. Open contacts adjacent to dental implant restorations: etiology, incidence, consequences, and correction. J Am Dent Assoc. 2016;147(1):28-34.
11. Byun SJ, Heo SM, Ahn SG, Chang M. Analysis of proximal contact loss between implant-supported fixed dental prostheses and adjacent teeth in relation to influential factors and effects. a cross-sectional study. Clin Oral Implants Res. 2015;26(6):709-714.
12. Varthis S, Randi A, Tarnow DP. Prevalence of interproximal open contacts between single-implant restorations and adjacent teeth. Int J Oral Maxillofac Implants.2016;31(5):1089-1092.
13. Varthis S, Tarnow DP, Randi A. Interproximal open contacts between implant restorations and adjacent teeth. Prevalence - causes - possible solutions. J Prosthodont. 2019;28(2):e806-e810.
14. Saponaro PC, Heshmati RH, Lee DJ. Using a porcelain furnace to debond cement-retained implant crown from the abutment after screw fracture: a clinical report. J Prosthodont.2015;24(3):239-242.
15. Diemer F, Stark H, Helfgen EH, et al. In vitro cytotoxicity of different dental resin-cements on human cell lines. J Mater Sci Mater Med. 2021;32(1):4.
16. Rasaie V, Abduo J, Falahchai M. Clinical and laboratory outcomes of angled screw channel implant prostheses: a systematic review. Eur J Dent. 2022;16(3):488-499.
17. Rella E, De Angelis P, Damis G, et al. The application of angulated screw-channels in metal-free, implant-supported restorations: a retrospective survival analysis. Materials (Basel). 2021;14(22):7006.
18. De Angelis P, Gasparini G, Camodeca F, et al. Technical and biological complications of screw-retained (CAD/CAM) monolithic and partial veneer zirconia for fixed dental prostheses on posterior implants using a digital workflow: a 3-year cross-sectional retrospective study. Biomed Res Int.2021:5581435.
19. Opler R, Wadhwani C, Chung KH. The effect of screwdriver angle variation on the off-axis implant abutment system and hexalobular screw. J Prosthet Dent.2020;123(3):524-528.