You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
A trend toward more conservative and minimally invasive treatment can be observed throughout healthcare. In medicine, historically, when a patient with heart disease required an aortic valve replacement due to calcific degeneration, it was completed with a sternotomy and cardiopulmonary bypass. Today, patients are offered a more conservative option called transcatheter aortic valve replacement, in which the heart is accessed by threading a catheter up to the aorta through the femoral artery. This less invasive strategy enables patients to forego the lengthy hospital stays, potential adverse effects, and rehabilitation process that comes with undergoing open heart surgery.
In dentistry, we are witnessing the same trend toward more conservative and minimally invasive treatment, which includes a paradigm shift toward a more targeted therapeutic approach with indirect restorations. Many of these advances have been facilitated by adhesive dentistry. Adhesive dentistry enables a more defect-driven approach to preparation design. Traditionally, when teeth were prepared for indirect restorations, it required the elimination of caries, erosion, decalcification, etc and then further preparation to create mechanical retention. Crown preparations require substantial removal of tooth structure in order to obtain mechanical retention. For example, Goodacre's conventional molar crown preparation requires an axial wall height of 4 mm.1 Many of the traditional design fundamentals and protocols for crown preparation are aggressive because they were formulated during an era of aqueous-based nonadhesive luting agents that relied exclusively on mechanical retention. However, with advances in adhesive dentistry, dentists are now able to provide indirect restorations with more conservative preparation designs.
Al-Fouzan and colleagues utilized microcomputed tomography to compare the volumetric loss of a traditional crown preparation to that of an onlay.2 According to the results, maxillary first molars lost approximately 50% of their volume for an all-ceramic crown preparation but only 38% of their volume for an all-ceramic onlay. Al-Fouzan and colleagues also found that mandibular first premolar preparations for full ceramic crowns demonstrated 62% volume loss, whereas onlay preparations for the same tooth demonstrated only 35% volume loss. So, why is conserving tooth volume so important? In theory, if a tooth is prepared more conservatively, its death cycle will progress more slowly because there is more remaining tooth structure for the next restoration. For example, the process can begin with a direct restoration, progress to the need for a larger indirect restoration, ultimately require root canal therapy, and then eventually result in the loss of the tooth. Of course, not all restored teeth go through the cycle in its entirety; many only experience one or two phases. Nonetheless, the more conservatively that teeth are prepared, the better their chances of surviving longer in the mouth.
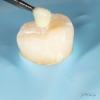
Adhesive dentistry enables a more conservative approach because it affords the possibility of restoring teeth using preparation designs without mechanically retentive features (Figure 1 and Figure 2). The defective tooth structure can be removed, and then the indirect restoration can be adhesively bonded into place. It should be noted, however, that placing an adhesively bonded restoration is arguably more technique sensitive than placing a traditionally luted one and thus presents more opportunity for failure.
Types of Dental Adhesives
Selecting an adhesive agent to use can be overwhelming and confusing. Adhesives can be categorized by either their generation or etching mode.3 The generation method of categorization is a bit misleading because it can lead consumers into believing that adhesives perform better with each generation; however, this is not necessarily the case. For example, some sixth- and fourth-generation adhesives have demonstrated better long-term success rates than many eighth-generation adhesives.
The first- through third-generation adhesives are no longer widely used. Fourth-generation adhesives involve multiple steps in which the etchant, primer, and adhesive are all applied separately. Later, the fifth-generation adhesives were developed, which attempted to simplify the process by combining the primer and adhesive but keeping the etchant separate. The sixth-generation adhesives also attempted to simplify the process but by combining the etchant and primer and keeping the adhesive separate. As attempts at further simplification continued, the seventh-generation adhesives were developed, which are colloquially referred to as "all-in-one" adhesives because they combine the etchant, primer, and adhesive. The eighth and final generation is relatively similar to the seventh generation; however, these adhesives are marketed as being able to be used in the etch-and-rinse, selective-etch, or self-etch modes. Some eighth-generation adhesives are also marketed for use with indirect restorations.
When an adhesive is categorized by its etching mode, it is considered to be either an etch-and-rinse adhesive or a self-etching adhesive. Etch-and-rinse adhesive systems require the use of a separate phosphoric acid etchant that is rinsed away before the adhesive is applied (Figure 3). Etch-and-rinse adhesives are further subcategorized as either three-step (fourth-generation) or two-step (fifth-generation) adhesives. Self-etch adhesives are further subcategorized as either two-step (sixth-generation) or one-step (seventh- and eighth-generation) adhesives.
For dentists to successfully place conservative, nonretentive restorations in the office, familiarity with the different types of adhesives that can be utilized is paramount. The best method for becoming familiar with an adhesive is to carefully review the manufacturer's instructions for use. Answers to questions about the bonding agent, such as whether or not it should be air dried or if multiple layers should be applied, can all be found in the instructions for use. There is no one-size-fits-all approach to applying an adhesive. The process for applying each is unique to the adhesive and carefully investigated by the manufacturer before it is brought to the market.
Clinical Efficacy
Long-term clinical studies and meta-analytical studies of laboratory and clinical data support the efficacy of adhesives. In a 2014 systematic review of randomized and non-randomized clinical trials, Peumans and colleagues evaluated the clinical effectiveness of contemporary adhesives in noncarious cervical lesions.4 Oftentimes, noncarious cervical lesions are used to evaluate the efficacy of adhesives because their preparations lack macromechanical retention and typically involve both the enamel and dentin substrates (Figure 4). Peumans and colleagues found significant differences in the average annual failure rates of adhesives by class except for glass ionomers and mild two-step self-etch adhesives, which demonstrated an average annual failure rate of 2.5%.4 Furthermore, a 13-year randomized controlled clinical trial evaluating a two-step self-etch adhesive in noncarious cervical lesions reported an annual survival rate of 93% when the adhesive was used in self-etch mode.5
The type of adhesive system used as well as the method of application may play critical roles in long-term survival. Simplified seventh-generation adhesives have been shown to have higher failure rates that are statistically significant when compared with fourth- and sixth-generation adhesives. Regarding universal adhesives, research has shown that some have demonstrated annual failure rates of 8.8% and 17.1%.4 That being said, other universal adhesives have performed well in clinical trials. A randomized clinical trial held over the course of 39 months found that CAD/CAM partial-ceramic crowns bonded with a universal adhesive used in selective-etch mode and a conventional resin cement had an approximately 96% survival rate. The survival rate of these restorations was significantly lower when they were placed with a self-adhesive resin cement.6
Conservative Onlays and Overlays
Long-term clinical data has demonstrated that conservative, nonretentive restorations have excellent success rates. These nonretentive restorations are referred to by many names in the literature, including onlays, occlusal onlays, overlays, occlusal veneers, posterior indirect adhesive restorations, and more. Oftentimes, searching the literature on this topic can be difficult because these restorations go by so many names. Malament's research group at Tuft's University recently published a large-scale clinical trial in the Journal of Prosthetic Dentistry evaluating the 10.9-year survival of partial coverage lithium disilicate restorations.7 In the study, the teeth were prepared for a defect-specific restoration, so only defective tooth structure was removed, and the preparations lacked mechanical retention and were adhesively luted. Malament and colleagues reported the overall 10-year survival rate of partial coverage lithium disilicate restorations to be 95.6%, which closely rivals the 96.7% 10-year survival rate of full-coverage lithium disilicate crowns.7
Guess and colleagues conducted a split-mouth clinical study investigating CAD-CAM partial coverage restorations, and the survival rate of the restorations restored with lithium disilicate was 100%.8 Similarly, Edelhoff's research group designed a prospective non-randomized clinical trial involving nonretentive lithium disilicate occlusal onlays, and the mean survival rate of these restorations was 100% over an average observation time of 7.9 years.9
Dentin Bonding
Some dentists express concern regarding the long-term reliability of bonding to dentin versus bonding to enamel. After all, enamel was the first substrate that the dental community learned to bond to when Buonocore pioneered the concept of acid etching enamel in 1955. It was not until years later that techniques for bonding to dentin became solidified.10,11Dentin, which is more structurally complex and has irregularly organized hydroxyapatite crystals and fluid-filled tubules, is a humid substrate that is more challenging to predictably bond to than enamel. However, despite the challenges, dentists can still predictably bond to dentin. Another research group reported a 96.4% survival rate for veneered teeth with 50% dentin exposure when an immediate dentin sealing technique was performed.12 The delivery of conservative non-retentive restorations, such as ceramic onlays, should not be avoided simply because the preparation will involve substantial dentin bonding.
Techniques for Success
Adhesive dentistry requires a meticulous approach. Adhesives are hydrophobic and therefore require a dry environment, so achieving proper isolation should not be overlooked. This is critical during the delivery of a nonretentive restoration because it can more easily become dislodged and swallowed by the patient. Caries-affected dentin can be bonded to, but the restoration will have a considerably weaker bond strength.13 Bonding to caries-affected tooth structure is less predictable because the caries process leads to increased porosity of intertubular dentin, dissolution of apatite crystals, and loss of mineral content. These alterations in dentin may decrease dentin hybridization. Using loupes for magnification may also help to facilitate successful delivery because the operator can more easily determine if the field is contaminated. Although contamination is always a consideration in dentistry, it is a far greater concern when using hydrophobic adhesive materials.
Queries regarding this course may be submitted to authorqueries@broadcastmed.com
About the Author
Melissa Seibert, DMD
Creator and Host
Dental Digest Podcast
US Air Force Dentist
Lackland Air Force Base
San Antonio, Texas
References
1. Goodacre CJ. Designing tooth preparations for optimal success. Dent Clin North Am. 2004;48(2):359-385.
2. Al-Fouzan AF, Tashkandi EA. Volumetric measurements of removed tooth structure associated with various preparation designs. Int J Prosthodont. 2013;26(6):545-548.
3. Sofan E, Sofan A, Palaia G, et al. Classification review of dental adhesive systems: from the IV generation to the universal type. Ann Stomatol (Roma). 2017:8(1):1-17.
4. Peumans M, De Munck J, Mine A, Van Meerbeek B. Clinical effectiveness of contemporary adhesives for the restoration of non-carious cervical lesions. A systematic review. Dent Mater. 2014;30(10):1089-1103.
5. Peumans M, De Munck J, Van Landuyt K, Van Meerbeek B. Thirteen-year randomized controlled clinical trial of a two-step self-etch adhesive in non-carious cervical lesions. Dent Mater.2015;31(3):308-314.
6. Scholz KJ, Tabenski IM, Vogl V, et al. Randomized clinical split-mouth study on the performance of CAD/CAM-partial ceramic crowns luted with a self-adhesive resin cement or a universal adhesive and a conventional resin cement after 39 months. J Dent. 2021;115:103837.
7. Malament KA, Natto ZS, Thompson V, et al. Ten-year survival of pressed, acid-etched e.max lithium disilicate monolithic and bilayered complete-coverage restorations: performance and outcomes as a function of tooth position and age. J Prosthet Dent. 2019;121(5):782-790.
8. Guess PC, Selz CF, Steinhart YN, et al. Prospective clinical split-mouth study of pressed and CAD/CAM all-ceramic partial-coverage restorations: 7-year results. Int J Prosthodont. 2013;26(1):21-25.
9. Edelhoff D, Güth JF, Erdelt K, et al. Clinical performance of occlusal onlays made of lithium disilicate ceramic in patients with severe tooth wear up to 11 years. Dent Mater. 2019;35(9):1319-1330.
10. Van Meerbeek B, Yoshihara K, Van Landuyt K, et al. From Buonocore's pioneering acid-etch technique to self-adhering restoratives. A status perspective of rapidly advancing dental adhesive technology. J Adhes Dent. 2020;22(1):7-34.
11. De Munck J, Mine A, Poitevin A, et al. Meta-analytical review of parameters involved in dentin bonding. J Dent Res. 2012;91(4):351-357.
12. Gresnigt MMM, Braeckmans A, van der Made SAM, Naves LZ. Partial anterior indirect restorations in cases with dentin exposure. Int J Esthet Dent. 2021;16(4):554-569.
13. Isolan CP, Sarkis-Onofre R, Lima GS, Moraes RR. Bonding to sound and caries-affected dentin: a systematic review and meta-analysis. J Adhes Dent. 2018;20(1):7-18.