You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Introduction
The plaque biofilm that forms on all hard and soft oral tissues in the oral cavity is reported to be the primary etiological agent for periodontal diseases.1-4 Procedures and devices have been designed for an efficacious plaque biofilm control, with the objective to mechanically disrupt its adherence to the tooth or gingival surface and/or to prevent its formation itself.1,5 Oral health care professionals recommend a daily dental plaque biofilm control that may consist of mechanical and chemical procedures.5-8 Substantial evidence shows that mechanical and/or chemical plaque biofilm control leads to reduction in prevalence and severity of gingival inflammation.6-8 Even though the complementary use of chemotherapeutic agents has been used, clinical evidence demonstrates that oral mechanical hygiene is fundamental to prevent and control caries and periodontal disease.9-11 More specifically toothbrushing remains the primary method for controlling supra-gingival accumulations.9,11 Although use of a toothbrush with dentifrice is an effective means for removing plaque biofilm on many tooth surfaces, it cannot completely clean the interdental surfaces when used exclusively.12
In populations that use toothbrushing alone, the proximal surfaces of posterior teeth are the predominant sites of residual plaque biofilm. Gingivitis and periodontitis are more pronounced in interproximal areas than on oral or facial aspects in patients who are prone to periodontal disease.9 Additionally, periodontal disease is recognized to progress faster interdentally.13 Good interdental oral hygiene requires a device that can adequately reach the interproximal area.14,15 Different types of products are designed to achieve this, such as floss, woodsticks, rubber-tip simulators, interdental brushes, and single-tufted brushes.5,6,12,15,16 Interdental brushes are advised for patients with type II interdental embrasures or embrasures having fifty percent of papillary fill, or rather half the embrasure space is open.15-17 These are small, specially designed brushes with soft nylon filaments twisted into a fine stainless steel wire and mimicking a miniaturized bottle-brush.5,6,15-17
Dental flossing is useful in cleaning interproximal surfaces of teeth with few adverse consequences,18 especially in type I interdental embrasures wherein the interdental space is filled with gingival papilla.17,18The improved interproximal gingival health when supplementing conventional toothbrushing with flossing has been ascribed to the ability of the floss to have improved access to the interdental sulcular area. However, flossing may not effectively clean wide interdental spaces, root surfaces, or concavities.15,16 To make the dental floss effective in such conditions, Gomes et al.19have recently presented a modification to the flossing technique and called it the ‘Knotted Floss Technique' (KFt). In their modification, a knot was tied in the floss at any distance in the middle third of the floss length enabling an increase in the effective width of the floss. This has enabled modified floss to be used in embrasures wider than those recommended for regular finger flossing. The modified floss was inserted past the interdental contact point by the regular finger flossing technique in the non-knotted area. The knotted area was engaged through the embrasure by a ‘to and fro movement' against the interdental tooth surface.19 It has been reported in a randomized-control-crossover study, that the KFt is as safe and as effective an oral hygiene method for reducing plaque biofilm, inflammation and bleeding when compared to conventional finger flossing (CFt) in type I gingival embrasures.18 However, this clinical evaluation of the KFt was not carried out in type II gingival embrasures and was not compared with interdental brushing (IBt) in such embrasures.
To assess the efficacy of interdental cleaning methods, one has to consider two points of references. One being the theoretical efficacy of the method based upon the clinical evidence, while the second being the practical efficacy, influenced by the acceptability of the method to clients and therefore their compliance.20 The purpose of this study was to compare the changes in scores of plaque biofilm accumulation, gingival inflammation, gingival bleeding and gingival trauma in patients who all used CFt, KFt, and IBt for 6 weeks each in type II gingival embrasures. Patients' acceptability of the techniques was also evaluated.
Methods
Study Design
For this 22-week, triple-phase, examiner-blind, randomized crossover clinical trial, a sample size of sixty individuals who were eighteen years and above were selected from among the outpatients of the Department of Periodontology and Oral Implantology at the Uttaranchal Dental and Medical Research Institute. A pilot study involving a convenience sample of six participants was conducted to determine the sample size for the main study. The sample size was calculated with a power of 80% and a confidence level of 95%, as per the criteria of Chow et al.21 The pilot study was used to verify that a ‘washout' phase of 2 weeks in-between any two treatment phases was sufficiently long, to rule out any carryover effect of the previous treatment procedure into the phase of the next treatment. Data obtained from pilot study was also used to measure the intra- and inter-examiner reliability. The inclusion criteria that were employed for selection of participants is described in Figure 1. The criteria were designed such that a cohort was selected that were without any confounding factors for plaque biofilm accumulation and gingival inflammation. For example, habitual unilateral mastication usually leads to accumulation of plaque and calculus on the contralateral side.24 The trial was conducted as per the guidelines in the Handbook for Good Clinical Practice.25 The research protocol was approved by the Institutional Ethics Committee of Uttaranchal Dental and Medical Research Institute, Dehradun, certificate No IEC/PA- 001/2017 (April 20, 2017).
Prior to their enrollment, each volunteer received written and verbal instructions on the three test techniques, namely CFt, KFt ,and IBt (Figure 2). Investigators AG and MS demonstrated to the volunteers all three techniques on models, for half-hour session, for three consecutive days. Each educational session consisted of not more than ten participants per investigator. On the fourth day, if AG and MS were both satisfied with the volunteer's proficiency in demonstrating each of the three interdental cleansing technique on models, an informed consent was taken and the volunteer was enrolled as a participant into the 22-week, three-phase crossover, single- (examiner) blind study protocol. If either of AG or MS were not satisfied with any volunteer's ability to perform the techniques as instructed, then that participant had to attend another educational session of a half hour and was evaluated again on the subsequent day. Thereafter, if either of AG or MS was unsatisfied with the ability of the volunteer to perform any one of the three techniques of interdental cleansing, then he/she was not enrolled into the study protocol and no further educational sessions were conducted.
Investigator AG randomly placed all participants into one of three groups by a draw of lots. Twenty lots were each inscribed as "CFt-KFt-IBt", "KFt-IBt-CFt" and "IBt-CFt-KFt." After a participant chose a lot, that lot was discarded from the bowl of lots, thus ensuring a linear decrease in available lots with enrollment of each participant. Only AG was responsible for this allocation and coding of participants to respective treatment groups, the other three investigators were blinded to the assignments.
Each group participated in three treatment phases of 6 weeks each, with a 2-week washout phase in-between any two treatment phases. The "CFt-KFt-IBt" group performed CFt in first phase, followed by KFt and IBt in the second and third treatment phase respectively. The "KFt-IBt-CFt" group performed KFt, IBt, and CFt in the first, second, and third treatment phase respectively; while the "IBt-CFt-KFt" group performed IBt, CFt, KFt, in their first, second, and third treatment phases respectively. The study design flow chart is shown in Figure 3.
At the baseline appointment for each treatment phase, every participant was given their assigned interdental cleansing products by AG. Participants assigned to conventional flossing received forty-six pieces of waxed floss (Reach; Johnson & Johnson, Mumbai, IND) 15 centimeters in length each piece, equally divided in two bags. Participants assigned to knotted flossing aid received the same except that every floss thread had a simple knot at around the middle of the strand. Each participant assigned to the interdental brush cleansing regimen received eight units of narrow size interdental brushes (Thermoseal; ICPA Health Products Ltd, East Mumbai, IND) instead of the pieces of floss. Participants were to use the respective interdental cleansing aids in the evening after dinner. Floss strands were to be discarded after a single session of use, while the interdental brush was reused for 6-7 sessions. Interdental brushes were to be rinsed in running water and placed in the interdental brush sleeve in an upright position. All participant received a sample of toothbrush (Oral B Allrounder Soft; Proctor and Gamble India Ltd.) and dentifrice (Colgate Strong Teeth; Colgate-Palmolive Ltd, Mumbai, IND) at the start of each treatment phase. Participants were instructed to brush their teeth twice a day in their customary manner and were cautioned not to use any other oral hygiene aid except for the assigned interdental cleaning device once a day. The first and second treatment phase were each followed by a ‘washout period.' During the washout period, the participants were instructed to perform normal oral hygiene practices of toothbrushing with dentifrice and refrain from using any floss, interdental brush, or any additional aid for plaque biofilm control.
Clinical Evaluations
Clinical evaluations of all participants were done at baseline, 3 weeks, and 6 weeks of each treatment phase. Both adjacent teeth and gingiva at test sites were scored for the Rustogi Modification of Navy Plaque Index (RMNPI),26 Lobene's Modified Gingival Index (MGI),27 and Barnett's Modified Papillary Bleeding Index (MPBI).28 The sequencing of examination was specifically chosen as plaque index, gingival index, and bleeding index, to avoid the possibility that the plaque biofilm would be removed during the recording of the other two indices.29,30 A disclosing agent (AlphaPlac; DPI Inc, Mumbai, IND) for plaque biofilm was applied gently using a cotton pledget to visually identify plaque biofilm. Gingival trauma (GT) was assessed by the method described by Carter-Hanson et al.29 as the presence or absence of signs of trauma in the marginal and papillary gingiva of adjacent teeth. The facial and lingual surfaces were examined visually for gingival lacerations. Presence of laceration, floss cut, or demarcation line/indentation at the site were scored as one, while a score of zero was recorded when there was absence of any signs of trauma. The score per participant was obtained by totaling all scores and dividing by number of sites examined.18,29
The indices were recorded by investigators AR and DP. To establish the intra- and inter-rater reliability, at least nine volunteers, selected at random from the out-patient clinic were examined at three weekly intervals throughout the study. Data recorded from the pilot study was also included for this purpose. Scores recorded from these volunteers and those of the pilot study were not included in the main study. The study schedule was distributed, so not more than six participants reported for examination on any given day of the week. AR and DP were blinded regarding the technique the participant was using.
Compliance
A compliance diary was also given to each participant at the baseline appointment of each treatment phase and was assessed at the end of each phase by AG and at end of all three treatment phases by AG & MS. The participants were instructed to record each interdental cleaning experience in this diary and any other event he/she felt was significant. A patient satisfaction questionnaire was answered by every participant at the end of the third and final treatment phase. Compliance or non-compliance by the participant was empirically established by calculating the amount of any unused portion of interdental cleaning product and by the entries in the diary. MS contacted the participants after completion of the study to verify any unusual entries in the compliance diary or to ascertain the reasons of excess unused floss returned to the department if any.
Data Analysis
Data was recorded by AR and DP into coded case sheets per participant, which was later decoded by AG. The data were entered into an Excel sheet (MS Office 2010) and then analyzed using SPSS® software version 17.0 (SPSS; Chicago, IL, USA). Gender-wise distributions were compared and the mean age was calculated. Since the sequencing of the treatment during the three phases of a crossover study has the potential to affect the comparison of scores between test and comparator groups, a 3-factor analysis of variance (ANOVA) was conducted to examine the effects of sequence of treatment phase and the possibility of any ‘carry-over' of the effects of first treatment phase into the second and third phase, despite the 2-week ‘washout' phase in between. The scores recorded during use of the CFt from all three groups were tabulated together for respective index at different time-points and the means and standard deviation calculated. Similarly, the scores of KFt and IBt were tabulated and means calculated for the observed indices at different time-points.
The mean differences of scores at respective time intervals of each of the index scored were compared between the three interdental cleansing techniques by using the analysis of variance (ANOVA) and the paired sample test. Also, a statistical analysis by paired t-test was done of scores recorded between time-points of 3 weeks versus baseline, 6 weeks versus baseline, 6 weeks versus 3 weeks of the respective index within the same treatment technique. This determined the improvement/worsening/no effect of respective scores of plaque biofilm, gingival inflammation, gingival bleeding, and gingival trauma over different time intervals while using the same interdental cleaning technique. All results were examined for statistical significance at pvalue ≤0.05. Participant responses to the end-study questionnaire were aggregated and analyzed on a percentage scale to compare preferences between each technique.
Results
An inter-examiner reproducibility for exact agreement with κ=0.77 ± 0.08 (SE) was observed for readings made between AR and DP, indicating an excellent level of agreement. An intra-examiner reproducibility for exact agreement with κ=0.83 ± 0.05 (SE) and 0.81 ± 0.08 (SE) for replicating the readings was recorded by AR and DP respectively, also indicating an excellent level of agreement.
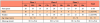
Data gathered from two participants was not included because they did not complete the third treatment phase, as they moved out of the country for employment. All clinical data was based on that recorded with the participants (n=58) who had completed all the treatment phases of study and no data has been included of the participants that withdrew from the study before completion. The age and gender distribution of the participants is shown in Table I.
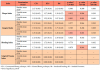
Mean scores at baseline, 3 weeks, and 6 weeks for RMNPI, MGI, MPBI, and GT for the respective treatment groups and the differences when the scores were compared between a pair of groups are shown in Table II. Baseline scores for the first three indices were statistically similar. The mean RMNPI scores of KFt and IBt group were significantly lesser than the CFt scores at 3 weeks and 6 weeks. The mean MGI scores of KFt and IBt group were statistically lower than CFt scores at 6 weeks. The mean MPBI scores recorded at 6 weeks in the IBt group was statistically lower than the respective mean score in the CFt group. There was no statistically significant difference between the mean scores of KFt group and IBt at respective time-points of the study for any of the indices studied.
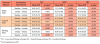
Within the same treatment group, the mean scores were compared to observe any improvement/worsening in scores (Table III). The mean scores of the CFt, KFt, and IBt group for the RMNPI, MGI, MPBI, were statistically lesser at 3 weeks when compared to baseline and statistically lesser at 6 weeks when compared to baseline. The scores of KFt and IBt group for all three above indices were statistically lesser at 6 weeks when compared to respective 3-weeks scores.
No incidence of gingival laceration or floss cut was reported nor observed during the period of study, when using any of the three interdental cleaning aids.
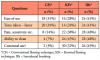
Percentage of replies and preferences by the participants to the patient questionnaire are shown in Table IV. Only two of the participants that completed the study stated that the CFt was better than the other two techniques in its ability to clean, and only one participant preferred to continue using the CFt as a future oral hygiene regimen. Of the remainder of the participants, they equally preferred between the KFt and IBt for its ability to clean the interdental embrasure and for willingness to continue using the technique for their oral hygiene regimen in future.
Discussion
In this three-phase crossover study, a ‘washout' phase of 2 weeks in-between any two treatment phases was used to rule out any carryover effect of the previous treatment procedure into the phase of the next treatment. In previous crossover studies, Carter-Hanson et al.29 used a 2-week washout period when comparing a floss holding device to conventional finger-flossing procedure, while Torkzaban et al.31 used a 7-day washout period when comparing a brushing and flossing sequence. In this study, the 2-week washout phase ensured parity in baseline clinical measurements prior to starting each treatment phase. Moreover, it was mandatory that the same inclusion and exclusion criteria applied to all volunteers at the start of each treatment phase.
Toothbrushing (up to twice daily) was shown to significantly improve gingival heath. However, it has been reported that brushing alone may remove less than 60% of overall plaque biofilm at each episode of self-cleaning.32 In a systematic review, Worthington et al.11 has stated that home use of any one of interdental cleaning devices like dental floss, interdental brushes, tooth-cleaning sticks, or oral irrigators, utilized in conjunction with toothbrushing is effective in reducing gingivitis, and even scores of plaque biofilm accumulation. In a recent, representative, cross-sectional study of adults in the United States aged >30years, it was discovered that self-care that included interdental cleaning was associated with less periodontal disease, decreased coronal and interproximal caries, and fewer missing teeth.33 A higher frequency of interdental cleaning (4 to 7 times per week) was associated with significantly lesser interproximal periodontal disease as compared to lower-frequency use of interdental cleansing (1 to 3 times per week) and non-users.33 However, investigators have reported a reluctance by the general public to routinely use interdental cleaning aids.29,34 Hence, there is a need for an alternative product or procedure for interdental cleaning, which can increase acceptability and compliance amongst the intended user.18,29 One such new procedure is the KFt.19 Results from this study have revealed a similar ability of the KFt as compared to IBt with respect to decreasing scores of plaque biofilm accumulation and gingival inflammation in type II interdental embrasures. Both techniques were superior to CFt at the same test-sites. Patient preference was high with the KFt and IBt and low with CFt. None of the three techniques tested resulted in any gingival trauma.
All participants performed regular toothbrushing with dentifrice for their daily oral hygiene, in addition to the assigned interdental cleaning technique. Hence, the changes in scores obtained with the use of any of the interdental cleaning techniques are not the result of the exclusive use of the interdental technique but when used in addition to toothbrushing. Use of interdental cleansing aids as an adjunct to toothbrushing has been recommended in multiple previous reports.11,18,31,33
There is only one other study in the literature that has evaluated the KFt. In that two-phase, single-blinded, clinical trial, it was reported that KFt was a safe and effective inter-dental cleaning technique for reducing plaque biofilm accumulation, gingival inflammation, and bleeding.18 The decreases in scores of plaque biofilm and gingival inflammation were similar to those when CFt was used, over a 6-week test phase of each technique. Similarly, in 2011, Imai and Hatzimanolakis35 conducted an examiner-blinded, randomized, 12-week, split-mouth clinical trial to compare the efficacy of IBt and CFt in the reduction of scores of gingival bleeding and plaque biofilm accumulation at type I embrasure sites in 30 volunteers. They inserted a color-coded probe to determine the best-fitting interdental brush for these proximal sites. Though no statistical differences were reported between the IBt and CFt for plaque scores, use of the IBt demonstrated statistically significant reductions in bleeding. Both the above studies were specifically carried out in participants with type I interdental embrasures. Therefore, the participants had intact interdental papillae, which limited the participants' and examiner's visibility of the disclosed plaque biofilm on interproximal tooth and root surfaces.
The current study was undertaken in type II gingival embrasures where interdental brushes are usually recommended over dental floss as an interdental cleaning aid.15,17 All the test techniques, namely CFt, KFt, and IBt, demonstrated significant reductions in scores of plaque biofilm accumulation and gingivitis. However, KFt and IBt were each statistically better than CFt in demonstrating these benefits of reduction in gingival inflammation and plaque biofilm accumulation. Hence, a modification in the flossing technique can result in similar efficacy in reduction of scores of plaque biofilm accumulation and gingival inflammation as IBt in type II embrasures.
Interdental brushes are known to be effective in removing plaque biofilm as far as 2-2.5 mm below the gingival margin.12 The consensus statement from the European Federation of Periodontology 2015 workshop states that "cleaning with interdental brushes is the most effective method for interproximal plaque biofilm removal, consistently associated with more plaque biofilm removal than flossing or woodsticks."36 The adjunctive use of interdental brushes has been shown to achieve significant improvements in clinical parameters such as scores of plaque biofilm, gingival bleeding, and sulcus probing depth, when compared to brushing alone.11 In a review of interdental cleaning aids by Sälzer et al., the interdental brush was shown to more effectively demonstrate reductions in interdental plaque biofilm and bleeding, especially in participants with clinical attachment loss, and thus, open embrasure areas.37
The superiority of interdental brushes was thought to be due to higher efficacy of plaque biofilm removal and high patient acceptance, as well as ease of use.35,36 In a randomized controlled clinical trial, Jackson et al.38 demonstrated that by interdental cleaning, especially with IBt, patients with chronic periodontitis were able to improve clinical periodontal outcomes and reduce the clinical signs of disease and inflammation over a 12-week period. Since their participants were recruited from a periodontal waiting list, they were likely to have open embrasures, meaning type II or III embrasures. A similar efficacy in reducing gingival outcomes was shown in the current study on type II embrasures. Because the bristles of an appropriately sized interdental brush are able to disrupt the interdental oral biofilm, especially in the concave tooth and root anatomy of premolars and molars, it has been argued that IBt can more effectively remove plaque biofilm from the invaginated axial cervical tooth surfaces as compared to CFt.35 Gomes et al.19 theorized that the increased cross-sectional width of the floss at the knot area can also disrupt the plaque biofilm accumulation in similar anatomical areas. These findings were also demonstrated in this study, as the KFt and IBt showed similar disruption of the interproximal oral biofilm which was sufficient to cause a shift in the equilibrium towards gingival health.
Participants' compliance with interproximal oral self-care is associated with their perceptions of ease of use and motivation. Lack of client compliance and/or the manual complexity of oral hygiene technique can be directly or indirectly responsible for lack of efficacy.37 Imai and Hatzimanolakis reported that an interdental brush, if properly chosen for its fit in the interdental embrasure, is easy to use, is well accepted by clients, and may positively influence daily interproximal self-care compliance.39 In the present study, nearly the same number of participants preferred the KFt and IBt for its cleaning ability of food impacted in the embrasure and would prefer to continue using either of these techniques in the future. When using IBt, it is necessary to choose the size of device according to the papillary fill. Choice of an oversized device can result in a risk of gingival trauma and papillary recession. Thus, it can be argued that a client who is adopting adjunctive use of IBt for self-care will need to use a combination of different sized devices for different types of embrasures. Results from this study have shown that the KFt is as effective as IBt in type II embrasures. Findings from a previously published study have demonstrated the efficacy of KFt to be similar to CFt in type I embrasures.18 Moreover, since the KFt entails only a small home-made modification in cheap and easily available dental floss, long-term use of the KFt is much less expensive than the use of IBt that has been used in previous studies.13,35,38
In a study on 26 dentate participants, Renton-Harper et al.40 demonstrated that the use of an instructional video using a ‘‘watch-and-follow'' program was beneficial in improving the efficacy of plaque biofilm removal with an electric toothbrush. They suggested the importance of such education techniques for improving results of other forms of mechanical tooth cleaning.40 It is easier to motivate participants with a high level of education as compared to participants with low education and low literacy levels.41 In the present study, the interventional techniques were demonstrated to the volunteers and only those who showed proficiency in the techniques were enrolled. They possessed a minimum education of higher secondary school certification and were able to satisfactorily understand oral hygiene education sessions. In a study by Segelnick, it was shown that after repeated, intensive one-on-one instructions, most participants demonstrated effective dental flossing technique.42 This could be the reason that no participant in the present study reported any episode of gingival trauma. It is therefore recommended that like any inter-proximal oral hygiene technique, recommendations of the KFt should include a demonstration of the proper technique.
Limitations and Future Research
Age, sex, economic status, frequency of visits to the dentist, smoking, and alcohol consumption have been considered as potential confounding factors in any study of periodontitis, including gingivitis.43,44 Though smokers were excluded from the cohort of this study, the selection criteria did not exclude volunteers based on any of other confounding factors. The choice of test area (upper or lower arches, left or right sides) did not affect the selection of participants nor criteria of being only left-handed (LH) or right-handed individuals (RH). All the participants in this study happened to be RH, which was observed when they completed their medical health histories and participated in the oral hygiene instruction sessions. Kadkhodazadeh et al. reported that LH individuals have lower plaque biofilm scores in the right quadrants and RH individuals have lower plaque biofilm indices in the left quadrants.45 Right handed individuals have been reported to have lower oral hygiene scores and a lower incidence of caries, possibly because of their better manual dexterity and brushing efficiency.46 These confounding variables may not necessarily have affected results of this study, as these variables were common during all intervention phases of the crossover study.18,29 However in a crossover study on flossing, Torkzaban et al. reported a significant influence of gender on scores of plaque biofilm and gingival bleeding.31 Future studies will need a larger sample size such that all confounding variables of periodontal disease are identified during sampling, and include a variety of socioeconomic groups as well as groups with different kinds of eating habits.43
Participants who were enrolled into this study were given instructions in interdental cleaning techniques and were thus well-motivated in diligently performing the procedure as required. It is debatable whether the favorable results in the efficacy of the three test techniques were achieved by cognitive behavioral intervention, or by the Hawthorne effect.5 This limitation may be diminished in a long-term study. Hujoel et al. advised against the extrapolation of results obtained from studies with professionally supervised flossing to typical floss users, since unsupervised self-flossers did not show any significant reduction in incidence of interdental caries.47 Since the participants were not directly supervised during the flossing procedure per se, it cannot be considered as supervised oral hygiene. Their compliance was ascertained not only by entries in their diary but also by the amount of interdental hygiene aids remaining in the supply kit at the end of the study. For ethical reasons, individuals with severe inflammatory gingival disease needing urgent professional care were excluded from the sample population. Since severely inflamed gingival tissues are more prone to injury, it is possible that such individuals would have had more cases of papillary gingival trauma while using interdental hygiene aids.
Ranganathan et al.48 and Sedgwick49 have recommended to look at the statistical and clinical significance independently. The statistical significance of the data was analyzed with a p-value of ≤0.05. The clinical significance reflects the extent of change, whether the change makes a real difference to an individual's life, how long the effects last, consumer acceptability, cost-effectiveness, and ease of implementation.48,49 Even though the KFt conforms to the latter three factors, its efficacy (as well as that of other interdental cleaning aids) necessitates a regular use by a well-motivated patient to achieve a beneficial effect over a long-term period. Future research is needed to test the effects of interdental cleaning aids in areas of previously inflamed gingiva or periodontitis. A detailed periodontal charting along with staging and/or grading of the periodontal status of the participants is also recommended.
Conclusion
Results from this clinical trial demonstrated that KFt is a safe and effective inter-dental oral hygiene cleaning technique for reducing plaque biofilm accumulation, gingival inflammation, and bleeding, as compared to IBt techniques in type II gingival embrasures, when used in conjunction with regular toothbrushing over a 6-week period. Both the KFt and IBt have shown to be superior to CFt for interdental cleansing in type II embrasures. The KFt appears to be a viable alternative to IBt in assisting patients in establishing cost-effective interdental cleansing habits in type II gingival embrasures.
Disclosures
None of the authors/investigators received any outside support, financial or otherwise from the companies producing the products used in this study. The study was wholly self-financed by contributions from the authors/investigators.
Aaron F. Gomes, MDS is a professor and Chair of the Department of Periodontics and Oral Implantology; Amit Rekhi, MDS is a senior lecturer, Department of Public Health Dentistry; Meru S, MDS is a professor and Chair of the Department of Oral Medicine, Diagnosis and Radiology; Divakar Pal, BDS is a post-graduate student, Department of Periodontics and Oral Implantology; all at the Uttaranchal Dental and Medical Research Institute, Mazri Grant, Dehradun, Uttarakhand, IND.
References
1. Chandki R, Banthia P, Banthia R. Biofilms: a microbial home. J Indian Soc Periodontol. 2011 Apr; 15(2):111-4.
2. Gurenlian JR. The role of dental plaque biofilm in oral health. J Dent Hyg. 2007 Dec; 81(suppl 1):116.
3. Lang NP, Bartold PM. Periodontal health. J Periodontol. 2018 Jun; 89(suppl 1):S9-S16.
4. Lasserre JF, Brecx MC, Toma S. Oral microbes, biofilms and their role in periodontal and peri-implant diseases. Materials (Basel). 2018 Sep; 11(10):1802.
5. Choo A, Delac DM, Messer LB. Oral hygiene measures and promotion: review and considerations. Aust Dent J. 2001 Sep; 46(3):166-73.
6. Harrison P. Plaque control and oral hygiene methods. J Ir Dent Assoc. 2017 Jun; 63(3):151-6.
7. Jafer M, Patil S, Hosmani J, et al. Chemical plaque control strategies in the prevention of biofilm-associated oral diseases. J Contemp Dent Pract. 2016 Apr; 17(4):337-43.
8. Mandal A, Singh DK, Siddiqui H, et al. New dimensions in mechanical plaque control: An overview. Indian J Dent Sci. 2017 May; 9(2):133-9.
9. Claydon NC. Current concepts in toothbrushing and interdental cleaning. Periodontol 2000. 2008 Oct; 48(1):10-22.
10. Rode S, Gimenez X, Montoya VC, et al. Daily biofilm control and oral health: consensus on the epidemiological challenge - Latin American advisory panel. Braz Oral Res. 2012; 26(suppl 1):133-43.
11. Worthington HV, MacDonald L, Poklepovic-Pericic T, et al. Home use of interdental cleaning devices, in addition to toothbrushing, for preventing and controlling periodontal diseases and dental caries. Cochrane Database Syst Rev. 2019 Apr; 4(4):CD012018.
12. Ng E, Lim LP. An overview of different interdental cleaning aids and their effectiveness. Dent J (Basel). 2019 Jun; 7(2):56.
13. Tarannum F, Faizuddin M, Swamy S, Hemalata M. Efficacy of a new interdental cleaning aid. J Indian Soc Periodontol. 2012 Jul; 16(3):375-80.
14. Asquino N, Villarnobo F. Interdental brushes, from theory to practice: literature review and clinical indications. [Internet]. Odontoestomatología. 2019 Jun; 21(33):46-53 [cited Oct 22, 2020]. Available from: https://odon.edu.uy/ojs/index.php/ode/article/view/277
15. Van der Weijden F, Slot DE. Oral hygiene in the prevention of periodontal diseases: the evidence. Periodontol 2000. 2011 Feb; 55(1):104-23.
16. Sana A, Pavithra S, Ahmed N. Interdental aids-a literature review. Open Access J Dent Sci. 2018 Jun; 3(2):000182.
17. Schmid M. Plaque control. In: Carranza F. editor. Glickman's clinical periodontology. 6th ed. Philadelphia: W.B Saunders Company; 1984. p.689-90.
18. Gomes AF, Rekhi A, Meru S, Chahal G. Efficacy, safety and patient preference of knotted floss technique in type I gingival embrasures. J Dent Hyg. 2019 Feb; 93(1):52-62.
19. Gomes AF, Meru S, Rekhi A. Knotted floss technique. J Adv Res Dent Oral Health. 2016 Apr; 1(1):6-7.
20. Asadoorian J. Flossing: Canadian Dental Hygienists Association position statement. Can J Dent Hyg. 2006 May; 40(3):112-25.
21. Chow S-C, Shao J, Wang H. Sample size calculations in clinical research. 2nd ed. Boca Raton: Chapman & Hall/CRC; 2008. 480p.
22. Silness J, Löe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964 Feb; 22(1):121-35.
23. Löe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963 Dec; 21(6):533-51.
24. Hada DS, Garg S. Unilateral mastication - silent messenger of periodontal status. Int J Periodontol Implantol. 2018 Apr; 3(2):80-3.
25. Adwazi K, Crawley F, Idänpään-Heikkilä JE, et al. Handbook for good clinical research practice (GCP): guidance for implementation. [Internet]. Geneva: World Health Organization; 2005 [cited 2020 Aug 17]. Available from: https://apps.who.int/iris/handle/10665/43392
26. Rustogi KN, Curtis JP, Volpe AR, et al. Refinement of the Modified Navy Plaque Index to increase plaque scoring efficiency in gumline and interproximal tooth areas. J Clin Dent. 1992 Jan; 3(Suppl C):C9-C12.
27. Lobene RR, Weatherford T, Ross NM, et al. A modified gingival index for use in clinical trials. Clin Prev Dent. 1986 Jan; 8(1):3-6.
28. Barnett M, Ciancio S, Mather M. The modified papillary bleeding index: comparison with gingival index during the resolution of gingivitis. J Prev Dent. 1980 Mar; 6(2):135-8.
29. Carter-Hanson C, Gadbury-Amyot C, Killoy W. Comparison of the plaque removal efficacy of a new flossing aid (Quik-Floss®) to finger flossing. J Clin Periodontol. 1996 Sep; 23(9):873-8.
30. Gomes AF, Meru S, Rekhi A. Letter to the Editor: Re: Reducing dental plaque and gingivitis with 0.6% Cortex Ilicis Rotundae toothpaste: a randomized, double-masked clinical trial. J Periodontol. 2017 Jan; 88(1):1.
31. Torkzaban P, Arabi SR, Sabounchi SS, Roshanaei G. The efficacy of brushing and flossing sequence on control of plaque and gingival inflammation. Oral Health Prev Dent. 2015 Jun; 13(3):267-73.
32. Slot DE, Wiggelinkhuizen L, Rosema NA, Van der Weijden GA. The efficacy of manual toothbrushes following a brushing exercise: a systematic review. Int J Dent Hyg. 2012 Aug; 10(3):187-97.
33. Marchesan JT, Morelli T, Moss K, et al. Interdental cleaning is associated with decreased oral disease prevalence. J Dent Res. 2018 Jul; 97(7):773-8.
34. Sälzer S, van der Weijden GA, Dörfer CE, Slot DE. Current evidence on prevention of gingivitis: oral hygiene devices and dentifrices. Int J Evid-Based Pract Dent Hyg. 2017 Summer; 3(2):118-27.
35. Imai PH, Hatzimanolakis PC. Interdental brush in type I embrasures: examiner blinded randomized clinical trial of bleeding and plaque efficacy. Can J Dent Hyg. 2011 Jan; 45(1):13-20.
36. Chapple IL, Van der Weijden F, Doerfer C, et al. Primary prevention of periodontitis: Managing gingivitis. J Clin Periodontol. 2015 Apr; 42(Suppl 16):S71-S76.
37. Sälzer S, Slot DE, Van der Weijden FA, Dörfer CE. Efficacy of inter-dental mechanical plaque control in managing gingivitis-a meta-review. J Clin Periodontol. 2015 Apr; 42((Suppl 16):S92-S105.
38. Jackson MA, Kellett M, Worthington HV, Clerehugh V. Comparison of interdental cleaning methods: a randomized controlled trial. J Periodontol. 2006 Aug; 77(8):1421-9.
39. Imai PH, Hatzimanolakis PC. Encouraging client compliance for interdental care with the interdental brush: the client's perspective. Can J Dent Hyg. 2010 Mar; 44(2):71-5.
40. Renton-Harper P, Addy M, Warren P, Newcombe RG. Comparison of video and written instructions for plaque removal by an oscillating/rotating/reciprocating electric toothbrush. J Clin Periodontol. 1999 Nov; 26(11):752-6.
41. Peeran SA, Peeran SW, Al Sanabani F, et al. "Education level" responsible for inequities in oral practices among 15-34-year-old individuals in Jizan, Saudi Arabia. J Int Soc Prev Community Dent. 2015 Mar; 5(2):120-4.
42. Segelnick SL. A survey of floss frequency, habit and technique in a hospital dental clinic and private periodontal practice. N Y State Dent J. 2004 May;70(5):28-33.
43. Cepeda MS, Weinstein R, Blacketer C, Lynch MC. Association of flossing/inter-dental cleaning and periodontitis in adults. J Clin Periodontol. 2017 Sep; 44(9):866-71.
44. Eke PI, Page RC, Wei L, Thornton-Evans G, Genco RJ. Update of the case definitions for population-based surveillance of periodontitis. J Periodontol. 2012 Dec; 83(12):1449-54.
45. Kadkhodazadeh M, Khodadustan A, Amid R, Darabi A. Plaque removal ability in left- and right-handed patients in different parts of the oral cavity. J Periodontol Implant Dent. 2012 Jun; 4(1):24-8.
46 Çakur B, Yıldız M, Dane S, Zorba YO. The effect of right or left handedness on caries experience and oral hygiene. J Neurosci Rural Pract. 2011 Jan; 2(1):40-2.
47. Hujoel PP, Cunha-Cruz J, Banting DW, Loesche WJ. Dental flossing and interproximal caries: a systematic review. J Dent Res. 2006 Apr; 85(4):298-305.
48. Ranganathan P, Pramesh CS, Buyse M. Common pitfalls in statistical analysis: clinical versus statistical significance. Perspect Clin Res. 2015 Jul; 6(3):169-70.
49. Sedgwick P. Clinical significance versus statistical significance. BMJ. 2014 Mar; 348:g2130.