You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
PART III: INFECTION CONTROL
Chapter 7: Rules, Regulations, Recommendations and Rationales
Infection control in dentistry has gained the attention of regulatory governmental agencies only since the mid-1980's. Prior to the AIDS pandemic, infection control among dental practitioners depended greatly upon their individual perception of risk and their determination of what precautions were appropriate. As a result, increasing numbers of dentists contracted the hepatitis B virus and reports of infected dentists transmitting their hepatitis B infections to their patients surfaced in the scientific literature.
Centers for Disease Control and Prevention
In 1986, the CDC published; Recommended Infection-Control Practices for Dentistry. This was the first time a government agency had developed guidelines specific to infection control in the delivery of dental care. However, the CDC is not a regulatory agency and therefore the guidelines were not enforceable by any governmental agency.
Subsequently, the CDC updated its guidelines in 1993 and most recently, in 2003. The current guidelines are in Appendix B of this review guide. It was not until the adoption of the Occupational Safety and Health Administration (OSHA) Bloodborne Pathogens Rule in 1990 that infection control in dental offices was required and enforced.
Since 1990, government agency activity in the area of infection control and safety for all healthcare settings, including dentistry, has increased dramatically. Regulations may pertain directly to the providers, such as OSHA and state board of licensure requirements, or indirectly by regulating the products dental workers use. Regulations cover patient safety, occupational safety, or environmental safety, depending on the responsibilities of the agency administering the rules. Some of the regulatory agencies involved are the:
• Occupational Safety and Health Administration (OSHA);
• Food and Drug Administration (FDA);
• Environmental Protection Agency (EPA);
• State and county health departments; and
• State and regional licensing agencies.
Occupational Safety and Health Administration
OSHA is an agency of the federal government whose mission is to "assure the safety and health of America's workers by setting and enforcing standards; providing training, outreach, and education; establishing partnerships; and encouraging continual improvement in workplace safety and health". As such, these rules and regulations target the employer on behalf of employees in an effort to establish safer workplaces and reduce work-related injuries and illnesses.
Although OSHA is a federal agency, states may voluntarily establish a state OSHA agency within their government framework and administer the rules on a more local level. The standards of the federal government then serve as the minimum standards for setting occupational safety regulations. The key point is that state OSHA programs may have regulations stricter than federal OSHA, but not less comprehensive.
OSHA regulates infection control through its Bloodborne Pathogens Rule. This regulation requires employers to provide education and training, appropriate protective measures, vaccinations and other methods and activities to ensure the prevention of exposure to blood and other potentially infectious materials (OPIM) that are a result of a person's work duties. The chapters that follow in this section cover the Bloodborne Pathogens Regulation requirements in more detail.
Food and Drug Administration
The FDA regulates the claims that manufacturers make regarding products, devices, equipment, and therapeutic agents. Companies that make certain types of medical/dental equipment such as sterilizers, handpieces, dental units, etc. must submit information regarding the safety and efficacy of their devices before they market them to the dental profession. The FDA determines what claims these manufacturers can place on their product or associate with their advertising materials. They do not allow manufacturers to use the fact that they have obtained FDA clearance in their marketing or advertising materials.
The FDA does not regulate the medical professional using the products or devices. However, there are ethical and legal liability issues with using a device for any purpose or application other than that which the manufacturer has cleared by the FDA. For instance, reprocessing and re-using a device (by disinfection or sterilization) labeled as single-use for more than one patient would be off-label use of an FDA-cleared device and could subject the user to liability if the patient suffers an adverse consequence.
Additionally, the CDC guidelines for infection control in dentistry state that single use devices should be used on one patient and then discarded. Many state dental licensing agencies have chosen to enforce the CDC guidelines through their dental practice laws and where this is the case, reusing devices would be a violation of the state standard.
Environmental Protection Agency
The mission of the EPA is to "protect human health and the environment". This government agency has very broad-reaching responsibilities that include:
• drinking water;
• hazardous and household waste;
• pollution prevention;
• wetlands, watershed and endangered species;
• radiation; and
• pesticides, among many others.
The EPA has ten regions, each of which has responsibility for states within its region. In addition, each state has some form of state environmental regulatory agency to ensure appropriate standards carry over from the federal government to the state level. For the purposes of infection control, EPA only regulates medical waste incinerators. Chapter 13 discusses regulation of dental office medical waste.
State Licensing Agencies
Many state licensing agencies regulate infection control in dental offices by requiring some minimum standard of care, and/or by requiring continuing education to include infection control. These requirements vary greatly from state to state, but in general would reflect the most recent CDC infection control guidelines. The remainder of this section details many of the expected infection control practices for the dental office.
Chapter 8: Sterilization
Sterilization is the terminal process used to ensure that instruments and devices that come into contact with the patient's oral tissues are free from contamination from previous patients. Not all dental instruments and equipment can withstand the heat sterilization process. There are chemical agents that achieve sterilization under the right conditions, but due to a number of factors, their use is limited and discouraged. Table 12 defines the categories of instruments, which is the first step in determining if an item must be sterilized or may be disinfected.
There are a number of devices and methods for achieving sterilization. We will discuss only those that apply to the practice of dentistry. Instrument reprocessing involves a number of steps.
Transporting Instruments
Upon completion of the dental appointment, transport instruments to the area where they will be cleaned, packaged, and sterilized. OSHA requires reusable sharps be transported in a puncture proof container that is solid on the sides and bottom. In their official directive, which outlines inspection guidelines for OSHA compliance officers, they state:
" Since reusable sharps, such as large bore needles, scalpels, and saws, pose the same percutaneous exposure hazard as disposable sharps, they must be contained in a manner that eliminates or minimizes the hazard until they are reprocessed. Therefore, the containers for reusable sharps must meet the same requirements as containers for disposable sharps, with the exception that they are not required to be closable since it is anticipated that containers used for collecting and holding reusable sharps will, themselves, be reused."
A possible solution is to place the instruments in a rigid plastic container upon completion of the dental procedure. In medical settings, workers use metal bins to transport used sharp instruments from the operating room to the instrument processing area. Sterilization of the bins or containers is not necessary provided they are used only for contaminated instruments.
Holding Solutions
If instruments cannot be cleaned immediately following use, a holding solution prevents debris from drying and becoming more difficult to clean. It is not necessary to use a holding solution or a "pre-soak" as part of routine instrument reprocessing where there is no delay in cleaning the instruments. It is more efficient to place the instruments directly into the cleaning device, such as an ultrasonic cleaner or washer, thus eliminating the additional step of pre-soaking.
If it is determined that a holding solution is necessary, select a mild product that will not cause pitting and corrosion of dental instruments. Instruments remain contaminated upon removal from the holding solution and it is necessary to wear heavy duty gloves in handling the instruments.
Cleaning
Wear personal protective attire throughout the cleaning process. Heavy duty gloves, gown or lab coat, mask, and eyewear will prevent the inadvertent contact with blood or saliva or contaminated solutions.
Mechanical cleaning, rather than hand scrubbing, is the preferred method of instrument cleaning. Hand scrubbing increases the handling of used sharp contaminated instruments, increasing the risk of accidental puncture injury. After mechanical cleaning, inspect instruments carefully and residual debris such as tissue or dental materials may then be removed using appropriate solvents or brushes.
There are two basic methods of mechanical cleaning used in dentistry. The first, ultrasonic cleaners, consist of a chamber into which the instruments are place. (Figure 1) A solution of water and detergent (formulated specifically for use with the ultrasonic cleaner and dental instruments) clean instruments with the assistance of sonic waves. The sonic waves produce cavitations, the mechanical means of cleaning instruments. A basket holds the instruments slightly elevated from the floor of the ultrasonic chamber, increasing the efficacy of the cleaning method. During operation, cover the ultrasonic machine to prevent the aerosolization of the fluids and potential contamination of the surrounding surfaces.
The second mechanical cleaning method is the use of instrument washers. (Figure 2) Instrument washers are a class of device more efficient and effective for the cleaning of dental instruments. Traditionally used in central sterilization services, such as in hospitals, these devices are relatively new to the dental profession. Two major categories of instrument washers are available to the dental market:
1. Instrument washer/disinfectors are Food and Drug Administration (FDA)-cleared medical devices that wash, disinfect and dry instruments.
2. Instrument washers, not cleared by the FDA to make the claim of disinfection, perform only the cleaning process. Some will also dry instruments.
Both may use a basket system to hold instruments, but are well-suited for use with instrument cassettes that hold and organize instruments. Household dishwashers will not substitute for these devices.
Instruments processed with a washer/disinfector are safe to handle, while those that have only been through a washing process require the same precautions as any contaminated items.
Regardless of the cleaning method used, it is important to dry instruments before placing into the final packing material prior to sterilization.
Packaging
Place critical and semicritical instruments and devices in appropriate packaging after drying and before sterilization. A variety of packaging exists for use with heat sterilizers, including paper pouches, plastic pouches, nylon tubing, and sterilization wrap. (Figure 3) If using instrument cassettes, the cassettes also require packaging with either wrap or pouches.
Generally, paper and plastic pouches or wrap will scorch or melt in a dry heat sterilizer. Nylon pouches or tubing is available for dry heat sterilizers. However, some settings may produce heat that will also melt nylon pouches. Always consult the manufacturer's instructions regarding the appropriate materials to use with a given sterilizer. Once wrapped or bagged for sterilization, place instruments in a single layer on multiple racks in the sterilizer or stacked loosely on their sides. Ensure adequate circulation of the sterilizing agent (i.e., steam and/or heat) between all packages of instruments. Instruments should remain wrapped or bagged until the time of use.
If the pouch or wrapping becomes wet, torn, or contaminated, repackage and resterilize the instruments. There is no rationale for routine sterilization of items based on shelf time. Instruments that have been sterilized wrapped or packaged will remain safe for patient use as long as the pack is uncompromised as described above. It is important to use only materials designed specifically for the sterilization process used, and to refrain from the reuse of these materials.
Sterilization
Heat sterilization is the desired method to reprocess multiple-use dental instruments and equipment. Most modern dental instruments are able to withstand the rigors of heat sterilization. Proper maintenance of items such as hinged instruments and dental handpieces will help increase the useful life of these items.
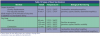
There are three major categories of heat sterilization available in dentistry. They are: steam under pressure (autoclave), unsaturated chemical vapor, and dry heat. Within these three classifications there are a few subcategories. Table 13 and Table 14 depict the types of heat sterilization used in dentistry and the times and temperatures required for sterilization. Time and temperature are for wrapped or packaged instruments. Although shorter cycles are available for unwrapped items it is inappropriate to routinely sterilize items unwrapped, since this does not allow for aseptic storage of instruments.
Sterilization Verification
Sterilization processes may fail due to equipment malfunction or operator error. Proper monitoring of sterilization procedures includes a combination of mechanical, chemical, and biological process monitoring.
Mechanical monitoring is simply observing the unit's gauges to confirm the proper times, temperatures, and pressure. (Figure 4) Chemical monitors use color changes on indicators to identify packages exposed to certain parameters, such as temperature and steam. (Figure 5) Examples of chemical monitors include autoclave tape, pouches with color-change indicators, and test strips processed in the packages of sterilized instruments. The CDC recommends chemical monitors on every package of instruments. Both of these types of indicators will tell the operator that some of the conditions necessary for sterilization were present, but they do not verify sterilization.
Biological indicators (BI), also called spore tests, are the only means currently available to verify sterilization. The BI is either a paper strip (Figure 6) or a vial of liquid medium (Figure 7) containing spores that are highly resistant to the sterilization process. The CDC recommends weekly biological monitoring of sterilizers, and many states have requirements for weekly, biweekly or monthly monitoring.
High Level Disinfection/Sterilization
A variety of chemicals exist that may provide either high-level disinfection or sterilization of instruments and devices. These products require immersion of the instruments for prolonged periods of time. Intended for use on critical and semi-critical instruments, the increase in heat-stable or disposable alternatives for items traditionally reprocessed in this manner has resulted in decreasing demand for these products. The CDC cautions that use of these chemicals is discouraged because of the difficulty verifying successful sterilization, the inability to wrap instruments, and safety concerns with occupational exposure to some of the chemicals that are used.
Chapter 9: Environmental Asepsis
Chemical Germicides and Equipment Barriers
For years, dental offices have relied on chemical germicides to decontaminate surfaces and equipment in the dental environment that are not detached for sterilization. By its very nature, disinfection differs from sterilization in its lack of sporicidal activity. Disinfectants are not capable of achieving sterilization. Heat sterilization is always the preferable method for sterilization of instruments used in the patient's mouth, or contaminated with patient body fluids (critical and semicritical instruments). High-level disinfectants are available for heat sensitive items. High-level disinfectants are not intended for use on environmental surfaces.
Housekeeping and Clinical Contact Surfaces
The CDC dental infection control guidelines identify two categories of environmental surfaces in the dental treatment room for the purpose of determining the appropriate level of asepsis. Housekeeping surfaces include:
• Floors
• Walls
• Doors
• Sinks
Housekeeping surfaces do not require disinfection after each patient but should be cleaned on a regular basis as part of the general housekeeping and sanitation procedures. If they become contaminated with blood, they should be disinfected with an intermediate-level disinfectant after cleaning.
Clinical contact surfaces include surfaces that are more likely to be handled during patient treatment or contacted with oral fluids. Areas that are touched with the worker's hand and may result in cross-contamination include:
• Light handles and switches
• Dental cart attachments such as high speed evacuator handles and hoses
• Handles of sonic scalers
• Buttons and knobs used to control dental devices and equipment during patient treatment
Clinical contact surfaces should be cleaned and then disinfected with a low- to intermediate-level disinfectant after each patient if barriers are not used. If barriers are used to protect surfaces, they should be of fluid resistant material and changed between each patient.
Chapter 10: Personal Protective Equipment
PPE
As part of standard precautions, dental personnel should make use of personal protective equipment (PPE). This includes, but is not limited to, gloves, protective eyewear, face masks, and protective clothing. (Figure 8) The purpose of PPE is to prevent the exposure of the DHCW to blood or other potentially infectious material (OPIM). OSHA requires employers to supply PPE to employees at risk of occupational exposure to blood or OPIM. OSHA also requires the employer to provide PPE at no cost to the employee. The employer is responsible for cleaning, laundering, repair, replacement and disposal of the PPE.
Gloves
Dental health care workers must wear gloves whenever there is the possibility that there will be bare-handed contact with blood, saliva, mucous membranes, or even blood-contaminated objects or surfaces. Gloves not only protect the DHCW from contact with microorganisms in the patient's mouth, but they also protect the patient from microorganisms on the DHCW's hands.
Gloves are single-use items, intended for use in connection with one patient. It is unacceptable to wash or decontaminate gloves for re-use. Gloves should be changed during a procedure when their ability to act as a barrier is compromised, as would happen if they become torn or punctured.
Hand washing, performed before donning and after removing gloves, is an essential element of asepsis. Hands serve as an excellent reservoir for transient and resident microorganisms that have the potential to transmit to the patient if there is a break in the hand hygiene or gloving protocol. Jewelry worn under gloves may tear or puncture the gloves and may harbor microorganisms. There is concern that petroleum-based products may accelerate glove deterioration, therefore the use of non-petroleum hand products is preferred for the clinical setting.
Types of Gloves
There are several types of gloves available. Always consider the type of procedure when selecting which glove is appropriate.
• Nonsterile Exam Gloves - These gloves are acceptable for most dental procedures. Traditionally, these are made of either latex or vinyl. Latex has been the most common material used, but there has been an increased incidence of latex sensitivity, in both dental health care workers and patients (see discussion of harmful reactions to latex below). Dental personnel who are allergic to latex may need to use an alternative, such as gloves manufactured with vinyl, polyethylene or nitrile rubber. The employer must supply the latex-allergic employee with an appropriate alternative. Often, non-specific dermatitis is mistaken for latex allergy. A worker with suspected latex allergy should always consult an appropriate health care provider such as an allergist or dermatologist for diagnosis. A true latex allergy has the potential to produce serious reaction, including shock and death and must be diagnosed and managed for the safety of the allergic individual.
• Sterile Surgical Gloves - Oral surgical procedures involve the incision, excision, or reflection of tissue that exposes the normally sterile areas of the oral cavity. Examples include biopsy, periodontal surgery, apical surgery, implant surgery, and surgical extractions of teeth (e.g., removal of erupted or nonerupted tooth requiring elevation of mucoperiosteal flap, removal of bone or section of tooth, and suturing if needed) Sterile surgical gloves are indicated for these procedures.
• Utility Gloves - Utility gloves are heavy-duty gloves used when disinfecting operatories and equipment, sterilizing instruments and when cleaning the high volume evacuation system. Replace utility gloves when they become cracked or their ability to function as a barrier is diminished.
Latex Hypersensitivity and Dermatitis
With an increase in the use of latex gloves and other latex products, there has also been an increase in hypersensitivity to this material, in both dental health care workers and patients. Latex gloves, manufactured with latex from rubber trees, may contain up to 200 different chemicals. It is the chemicals that are the primary irritant in latex gloves, although in rare instances individuals are allergic to the proteins in the natural rubber latex (NRL).
Reactions to latex gloves occur because the individual is sensitive to either the latex proteins or to various chemicals used in the manufacture of the gloves. Three different types of reactions may occur: irritant dermatitis, allergic dermatitis, or latex allergy.
Irritant dermatitis is a non-allergic response to chemicals or physical irritation, either from the gloves or other sources. With this reaction, the skin on the hands will become sore, dry and red, and may crack and peel. Common causes of irritant dermatitis are water, detergents, solvents, acids, alkalis, adhesives, metalworking fluids, and friction. Irritants damage the skin by removing oils and moisture from its outer layer, allowing the irritants to penetrate more deeply and cause further damage by triggering inflammation.
Allergic contact dermatitis often looks similar to irritant contact dermatitis, but is caused by an immune response following skin contact with an allergenic substance, in this case chemicals used in the manufacture of gloves. Tiny quantities may be sufficient to cause allergy, whereas a certain minimum exposure is necessary for irritant contact dermatitis. Irritant and allergic contact dermatitis may coexist.
Latex allergy is an allergic reaction to the naturally occurring proteins in the latex. With this reaction, the symptoms can range from dermatitis to anaphylaxis. The latex proteins may also become airborne when other workers removed their powdered gloves and the proteins, which adhere to the powder, are released into the environment.
In addition to the latex gloves, many other materials in the dental office, such as latex rubber dams, prophy cups, or orthodontic elastics may pose problems for these patients (and for latex sensitive staff also). A detailed medical history is essential in identifying patients who may be allergic to latex. Examples of high-risk groups include: patients with a history of spina bifida, allergies to bananas or avocado, and those with a history of multiple surgeries. If a patient has a latex sensitivity, clearly label the chart with the words "Latex Allergic" so that all office personnel are alerted to this fact.
Protective Eyewear
Protective eyewear, worn whenever there is a potential for spray or spatter, such as during the use of handpieces, air/water syringes, and laboratory equipment, protects the eyes from splatter that may contain blood, saliva and chemicals, and from flying debris such as fragments of amalgam or teeth. Appropriate eyewear includes goggles or eyeglasses with solid side shields, chin-length face shields or masks with face shield attachments. Patients need protective eyewear to prevent accidental splatter and flying debris from getting in their eyes. Follow proper decontamination procedures using a low to intermediate level disinfectant after each use of protective eyewear.
Face Masks
As with protective eyewear, face masks provide a barrier against spray and spatter that potentially contain infectious organisms. The mask must completely cover the nose and mouth and fit snugly to the face, but should not contact the mouth. A mask that can filter at least 95% of droplet particles 3-3.2 microns in diameter is best. These are generally labeled as surgical masks. A new mask should be worn for each patient, or more often it becomes heavily moistened. Excessive moisture may break down the filtration media in the mask and compromise the barrier properties.
Protective Clothing
When there is potential for contamination of workers' clothes or skin with blood or saliva, wear protective clothing, such as a lab coat or clinic gown. The protective clothing needs to be adequate to prevent penetration of blood or saliva through the garment and onto clothes or skin. Long-sleeve protective attire is indicated for most dental procedures.
For more high exposure procedures, such as oral and periodontal surgery, fluid-resistant material might be necessary. Whatever the material, the protective attire should be changed daily at a minimum, or more often when visibly soiled.
Always remove PPE prior to leaving the work area. This means that when a worker goes to and from work, to lunch, or any other activity outside the office, they must leave all protective attire behind.
Employers are required to either provide disposable clothing or to take responsibility for laundering protective clothing. Staff members must not take this clothing home for laundering. When laundering clothing in the office, the person responsible must wear gloves, protective eyewear and a face mask. If an outside laundry or cleaning service is used, contaminated linens should be transported in appropriate bags and labeled with a biohazard symbol (described later).
Handwashing
In October 2002, the Centers for Disease Control and Prevention (CDC) published a Guideline for Hand Hygiene in Health-Care Settings.The Association for Practitioners in Infection Control and Epidemiology (APIC) published a previous major guideline for hand hygiene in 1995. Both documents cite prolific evidence that hand asepsis is likely the most important aspect in preventing the spread of infectious diseases in healthcare settings. The CDC's Guideline for Infection Control in Dental Health-Care Settings, 2003,applies many of the hand hygiene concepts presented in the previous guidelines, with a specific focus on the practice of dentistry.
Handwashing is one of the most important components of infection control. It is one of the most effective ways that dental personnel can prevent the transfer of microorganisms from one person to another. A dental health care worker's hands harbor two types of microorganisms, resident flora and transient flora. Resident flora are organisms present on the hands of the worker and tend to be in the deeper layers of skin. These microorganisms carry a lower threat of infectious disease transmission than transient flora. Transient flora are not naturally occurring on the hands, but are picked up primarily from environmental surfaces. These organisms tend to reside on the outer layers of the skin and are relatively easy to remove through proper hand washing techniques.
Alcohol-based Hand Rubs
The 2002 Hand Hygiene guidelines cite twenty-two studies comparing the relative efficacy of plain or antimicrobial soaps to that of alcohol-based antiseptics in reducing counts of viable bacteria on hands. All but two found that the alcohol reduced bacterial counts on hands more than washing hands with soaps or detergents containing a variety of antimicrobial agents.
Alcohol hand rubs present benefits in the form of increased antimicrobial activity over soaps, greater accessibility in areas that do not have sinks with running water, and according to the literature, potentially increased compliance with handwashing protocols. However, alcohol hand rubs are only for use on hands that are not visibly dirty or contaminated with proteinaceous materials, such as blood. Although alcohol-based hand rubs have antimicrobial activity superior to that of most antimicrobial hand soaps, it does not replace these products in the dental office or other healthcare settings. Physical removal of debris is required for visibly dirty or contaminated hands before an alcohol hand rub may be used. In the absence of visible debris, it is acceptable to use alcohol-based hand sanitizers alone.
Routine Handwashing Technique
For routine or non-surgical dental procedures, workers should wash visibly soiled hands with soap (either antimicrobial or non-antimicrobial) and water. If hands are not visibly soiled, an antimicrobial soap and water, plain soap and water, or an alcohol-based hand rub may be used.
In order to prevent cross-contamination, the ideal situation is to have foot-controlled or electronically controlled faucets and soap dispensers. If not using one of these types of soap dispensers, be sure to use a pump soap dispenser as opposed to bar soap, which can harbor microorganisms. Do not refill or top off soap dispensers, as this can result in contamination of the soap. Either completely empty and rinse containers before refilling, or use disposable containers. Use a paper towel to turn off the faucet after washing hands if a foot- or electronically controlled faucet is not available.
Frequent handwashing may cause the hands to become dry, irritated, and cracked. It is important to take good care of the hands because nonintact skin does not act as a barrier against microorganisms. It may be necessary to try various products to find one that will not irritate the skin. In addition, hand lotion or a protective skin barrier cream may help to keep the skin healthy. When using lotion it is important to avoid oil-based products because they may deteriorate the latex of gloves.
Surgical Hand Hygiene
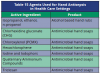
For oral surgical procedures, workers should perform surgical hand antisepsis using both antimicrobial soap and water, or plain soap and water followed by an alcohol-based hand rub with persistent antimicrobial activity (Table 15). Following surgical hand hygiene procedures, carefully place sterile surgical gloves on hands, taking care to avoid contamination of the outside of the gloves.
Exposure Prevention
Accidental exposure to patient's blood or saliva through inadvertent injury with contaminated sharp instruments is a potential avenue for occupational transmission of bloodborne diseases. Altering the manner in which a job is done to make it safer (work practice controls), or using safer devices (engineering controls) are two methods that help prevent accidental exposures.
Some of the examples of work practice controls include:
• The safe transfer of instruments from operator to assistant and back
• Chair positioning to increase focal distance and decrease the amount of splatter from dental handpieces and other devices to the healthcare workers' faces
• The use of a dental dam to decrease the amount of saliva in splatter from dental handpieces and other devices
Some examples of engineering controls include:
• Retractable scalpels
• Needles with sliding sheaths
• Needle-free IV ports
• Safety IV catheters
Although engineering controls are not always available for sharp devices used in dentistry, OSHA requires their use when they are available. At a minimum, the employer must actively seek out devices available to the dental profession and conduct an evaluation to determine if the device is suitable for use in their setting. Some reasons a device may be found unsuitable would be that the device:
• Interferes with the delivery of patient care
• The device is not safer than the alternative currently in use
• The device is not generally available
When safety needles are not used, reusable needles should be recapped using a one-handed scoop technique or some other device that prevents the needle from having potential contact with the worker's hand during recapping. OSHA specifically prohibits manually recapping the syringe using a two-handed technique.
Exposure Incident Management
Despite best effort, exposure to patient's blood or OPIM may occur through percutaneous injury, splash to the mucous membranes of the eyes, nose, or mouth, or by contact with body fluids to the nonintact skin of the worker. It is important to have an effective management protocol in place before an incident occurs. Timely follow-up by an appropriate health care provider is essential for good post exposure management. Chapter 14 details the elements of an exposure management protocol in the section entitled Occupational exposure follow-up.
Chapter 11: Immunizations
Immunizations are a primary defense against vaccine-preventable disease. Every health care worker needs to be aware of what vaccinations are recommended and whether their immunizations are up to date. Many of the immunizations are given during childhood and do not require repeated vaccination. People with a history of some of these diseases may not require vaccination. Most vaccines do not require re-immunization later in life (e.g., MMR, hepatitis B). Other diseases have viral shifts each year and require annual revaccination (i.e., influenza).
Vaccines recommended for all health care workers include:
• Hepatitis B;
• Influenza;
• Measles, Mumps, Rubella (MMR);
• Varicella (chicken pox);
• Diphtheria;
• Tetanus (tetanus and diphtheria vaccines are usually given in childhood as the DPT vaccine, which also contains pertussis).
Chapter 12: Radiographic and Laboratory Asepsis
Taking dental radiographs poses the potential for cross-contamination. In order to decrease the risk of cross-contamination, the dental professional should use the appropriate personal protective equipment, use protective barriers on equipment when possible, use heat sterilizable or disposable equipment, and follow recommended procedures for exposure and processing of films. When using digital radiographic equipment, cover the sensor and keyboard with impervious barriers, since they cannot be heat-sterilized. Place clean new barriers for each patient.
Impervious barriers such as plastic bags are ideal for covering the x-ray tube head. Alternatively, use a low- to intermediate-level disinfectant to clean and disinfect equipment between patients. Use plastic sheets or other impervious barriers to protect the control box dials and exposure activation button.
If exposing a panoramic radiograph, place protective barriers on the exposure control switch and, if possible, on the chin rest, head position guides, and hand grips. Use either disposable or sterilizable bite sticks and change between each patient. Those areas that are not covered must be cleaned and disinfected after use.
Equipment
Disposable equipment, such as film holders, bitewing tabs, and bite blocks, provides the quickest and easiest answer to infection control issues. Otherwise, it is necessary to sterilize film positioners and other reusable equipment after each use.
Exposure Procedures
Place a plastic-backed patient napkin over the protective apron and thyroid collar during exposures. This helps prevent saliva contamination of the apron and thyroid collar. Remember that when gloves are contaminated, touch only those surfaces covered with a barrier. Clean and disinfect surfaces that are not covered and were touched with contaminated gloves during the procedure. Place the exposed films in a paper cup, but avoid touching the exterior of the paper cup, so that it does not become contaminated.
If using barrier films, remove the barrier from the film before placing it in the paper cup, being careful to not touch the film or the cup with the barrier or contaminated gloves. After completing the x-rays, remove the patient napkin from the lead apron. Avoid touching the lead apron with contaminated gloves. Ask the patient to assist in removing the lead apron if there is concern regarding cross-contamination by the worker's gloves. Remove barriers and clean and disinfect areas as appropriate before seating the next patient.
Processing Procedures
All dental personnel should adhere to infection control procedures for both automatic and manual processing to avoid cross-contamination.
Automatic processors with daylight loaders perhaps pose the greatest challenge when trying to avoid cross-contamination. These are designed in such a way that the hands must be passed through sleeves that are usually made of cloth. These sleeves are easy to contaminate, and it is not possible to adequately disinfect them. Avoid contamination by refraining from placing contaminated gloved hands through the sleeves.
It is possible to disinfect poly-coated film packets using a low- to intermediate-level disinfectant, then to process the film while wearing a clean pair of gloves. If the films are not disinfected, or barrier films were not used, follow the processing procedures below to avoid cross-contamination.
Automatic Processor with a Daylight Loader
1. Put on a clean pair of gloves and carry the cup containing the exposed films to the processor.
2. Open the top of the processor and place the cup of exposed films and 2 extra cups into the processor.
3. Close the cover and put hands through the insertion sleeves. Take an exposed film from the cup and open it, dropping the film into one of the empty cups. Place the film packet in the other empty cup.
4. Continue this procedure for all films.
5. After opening all films, remove gloves and place them in the cup with the contaminated film packets.
6. Place films into the slots of the processor, being careful to handle them only by the edges.
7. Remove hands through sleeves. Open top of processor and remove the cup. Put on a clean pair of gloves and separate foil from packets. Discard packets according to local and state regulations and place lead foil in appropriate container for recycling. Remove gloves and wash hands.
Automatic Processor without a Daylight Loader
1. Put on a clean pair of gloves and carry the cup containing the exposed films to the darkroom.
2. Place an opened paper towel on the counter.
3. Turn on safelights and turn off overhead light.
4. Take an exposed film from the cup and open it, dropping the film onto the platform of the processor. Place the film packets and lead foil on the opened paper towel.
5. After opening all films, dispose of packets and place lead in appropriate container. Remove gloves. Wash and thoroughly dry hands.
6. Place films into the slots of the processor, being careful to handle them only by the edges.
Manual Processing
1. Put on a clean pair of gloves and carry the cup containing the exposed films into the darkroom.
2. Check the temperature of the developer and set timer accordingly. Stir solutions and set racks on counter.
3. Open two disposable towels and place them on the clean dry counter.
4. Turn on safelights and turn off overhead light.
5. Take an exposed film from the cup and open it, dropping the film onto one paper towel. Place the film packet and the lead foil on the other paper towel.
6. Continue this procedure for all films, being careful not to touch the unwrapped films.
7. When all films have been opened, dispose of film packets and place lead foil in appropriate container for recycling. Remove gloves. Wash and thoroughly dry hands.
8. Place films on the racks, being sure to handle them only by the edges. Check to be sure that they are all secure. Continue processing using the proper time/temperature technique.
9. When films are in the fixer solution, turn on overhead light, wash hands, reglove (utility gloves), and disinfect the counter top and any other area that may have been contaminated.
Dental Laboratory
The CDC recommends cleaning and disinfecting all laboratory items used in the mouth before sending to the laboratory. This includes items such as impressions, bite registrations, fixed and removable prostheses, and orthodontic appliances. In addition, before delivering prostheses to the patient, clean and disinfect all items.
Effective infection control in the laboratory involves education and communication. All personnel involved must be educated about, and follow standard laboratory infection control procedures. Communication regarding protocols for disinfection of impressions and prostheses between the dental office and the commercial laboratory is essential. Duplication of disinfection procedures, although seemingly a good idea, may distort or corrode some items, while a lack of disinfection poses the serious risk of cross-contamination.
Whenever possible, disinfect items to be used with laboratory equipment. This reduces the need to sterilize or disinfect laboratory equipment. If lab equipment, such as lathe pans, rag wheels, and polishing stones become contaminated during use, they should be disinfected with an appropriate low to intermediate level disinfectant, or heat sterilized.
The disinfection of impressions poses problems because many impression materials are adversely affected by disinfectant solutions. It is extremely important to consult the manufacturer regarding which disinfectant to use for the particular impression material in question. There are some general recommendations that have been shown to be effective and without adverse effects on the final outcome of the case.
Wear personal protective equipment when working with all dental impressions because they are contaminated with saliva and often with blood. After removal from the mouth, gently rinse the impression in order to remove debris and shake to remove excess water. If stubborn debris remains, use a small amount of stone mixed with water and a soft brush to carefully remove the excess debris. Brush away from your face. Use an EPA registered, low- to intermediate-level disinfectant compatible with the impression material. Immersion is the preferred method when possible, as this is more likely to reach all contaminated surfaces. If immersion is not feasible, wrap the item in disinfectant-soaked towels for the time recommended on the disinfectant label.
Disinfect new prostheses or appliances before placing in the patient's mouth. Clean and disinfect any prosthesis or appliance brought to the dental office for an adjustment or repair. Thoroughly rinse items after disinfection and before delivery to the patient.
Chapter 13: Medical Waste
State and local public health authorities regulate contaminated medical waste. Regulations may differ significantly from location to location. Some general rules regarding medical waste do apply.
Contaminated Waste
Dental office contaminated waste consists of items that may be contaminated with blood or saliva. Contaminated waste must be handled carefully, and measures implemented that will prevent bare-handed contact with these items. These measures include:
• Refraining from discarding items that would release blood or saliva during handling into the regular trash.
• Instructing all personnel to refrain from pushing down on top of trash to compress.
• Emptying trash by removing trash can liner with contents to reduce potential for bare-handed contact with items.
Trash generated during patient care that will not release blood or saliva during handling does not require a biohazard bag. There are no incidents of medical waste causing a disease outbreak, indicating that it poses little risk to the public. Examples of non-regulated medical waste (unless they would release blood or saliva during handling) include:
• Gloves
• Patient bib
• Tray covers for instrument trays
• Disposable PPE
• Teeth, if given to the patient or to a dental school
Regulated Medical Waste
Regulated medical waste is the waste with potential to release blood or saliva during handling and contaminated disposable sharp items (sharps). This waste is collected in containers that are labeled with the universal biohazard symbol, leak-proof, solid on the sides and bottom, and closable. Examples of regulated medical waste include:
• Gauze used during surgical procedures
• Used syringe needles
• Used suture needles
• Used disposable scalpels/blades
• Ends of orthodontic wires
• Ends of wires used during fracture reduction
• IV and IM syringes/needles
• Tissue
• Liquid blood or OPIM
Collect all disposable sharps in the specialized containers intended for that purpose. (Figure 9 and 9A) Keep one sharps container at each dental chair for the discarding of sharp items as soon as feasible after use. Avoid the transport of disposable sharps to a central disposal location in the office.
Collect "soft" waste separately from the sharps in a container designed for that purpose. Most states have storage time limits for medical waste. There is often a shorter time in which soft waste may be stored as compared to the longer storage periods for sharps containers.
In most locations, it is permissible to discharge fluid blood or OPIM down the sanitary sewer line. For specific requirements, check with the state or county department of public health.
Chapter 14: Dental Waterlines
This chapter excerpted from the workbook, From Policy to Practice: OSAP's Guide to the Guidelines, is used courtesy of the Organization for Safety and Asepsis Procedures (OSAP).
Dental Waterline Contamination
In many dental practice settings, water used for dental treatment comes from the municipal water supply directly into the dental unit. Thin, plastic tubing carries water from the dental unit to the highspeed handpiece, air-water syringe, ultrasonic scaler, and subsequently, to the operating field in the patient's mouth. The inside surface of these dental waterlines can become colonized with a variety of microorganisms; including bacteria, fungi, and protozoa that live inside a slime layer that protects and feeds them. This phenomenon, called a biofilm, allows microorganisms to survive and thrive in dental waterlines and raises concerns about possible health effects of exposure to dental unit water.
Biofilm forms in all water environments. The structure of narrow-bore dental tubing and the typical way dental unit water is used in the practice setting, however, worsens the problem.
Dental waterlines hold only a small volume of water, almost all of which is in contact with the inside surfaces of the tubing. This allows any microorganisms present in the water to latch on to tubing walls, where they multiply to create a biofilm. Once formed, the biofilm serves as a reservoir that can increase the number of free-floating microorganisms in water used for dental treatment.
Microbial counts in dental treatment water can reach as high as 200,000 CFU/mL within five days of installing new dental unit waterlines. Counts greater than 1,000,000 CFU/mL have been reported.
Although oral flora and some human pathogens have been found living in dental water systems, most organisms recovered from dental waterlines are common water bacteria that have little potential for causing illness in healthy, immunocompetent persons. Nonetheless, for the purposes of providing health care, using water of poor quality is simply not acceptable.
No measurable risk to dental workers or patients from exposure to dental unit water has been calculated, but reasons for concern remain. For example:
• Dental workers were found to have altered nasal flora or significantly higher titers of Legionella antibodies, suggesting exposure to the microorganism that can cause Legionnaires' Disease.
• According to one scientific publication, contaminated dental water may have been the source of infections in the gingival tissue of two immunocompromised patients. Pseudomonas aeruginosa, a common water bacteria, was the cause of their infections.
• Waterborne microorganisms have been linked to numerous infections and instances of disease transmission in hospital settings and in the community.
Dental unit water that remains untreated or unfiltered is likely to contain high numbers of microorganisms and unlikely to meet drinking water standards. Use available commercial devices and procedures that improve the quality of dental treatment water to standards set by the EPA for safe drinking water (less than 500 CFU/mL).
Improving Dental Water Quality
Dental water that remains untreated or unfiltered is not likely to meet drinking water standards. To control and maintain the quality of dental unit water:
• Contact the manufacturer of your dental unit to find out which method(s) of water quality control are compatible with your unit. Always follow the manufacturer's instructions for using any waterline maintenance product or protocol. Follow the schedule for maintenance set forth by the manufacturer.
• Use commercial devices and procedures designed to improve the quality of water used in dental treatment. Methods shown to be effective include:
• Self-contained water systems used with other available methods,
• Chemical treatment,
• In-line microfilters, and
• Combinations of these treatments.
• Use source water containing less than 500 CFU/mL of bacteria (for example, tap, distilled, or sterile water). In most urban areas, municipally plumbed water meets this standard. However, source water control alone will not eliminate contamination in treatment water if biofilm in the water system is not controlled. Even with a self-contained water system, water can become contaminated as it runs from the tubing to the patient's mouth. Controlling source water quality can only be effective if the biofilm in the waterline is eliminated through the use of available devices, products, and procedures.
• Clean self-contained water systems according to the manufacturer's instructions. Improperly maintained, these devices can become highly contaminated.
• After each patient, run any dental device used in the mouth and connected to the dental water system for a minimum of 20-30 seconds to discharge water and air. Running handpieces, ultrasonic scalers, and air-water syringes after use physically flushes out any patient material that may have entered the turbine, air, or waterline.
• Do not rely on flushing waterlines at the beginning of the clinic day to maintain water quality. Flushing does not affect biofilm in the waterlines or reliably improve the quality of water used during dental treatment. Dental workers may wish to flush lines before beginning patient appointments for the day to clear stagnant
water from the lines, but flushing is no longer recommended as a water quality-control measure.
• If using a dental unit manufactured before 1985, consult the owner's manual or contact the manufacturer to determine whether anti-retraction valves or other devices are (or should be) present and require testing or maintenance. Most recently manufactured dental units are engineered to prevent retraction of oral fluids, but older systems often have valves that require periodic maintenance. Even with anti-retraction valves, flushing the above devices for a minimum of 20-30 seconds after each patient is recommended.
Chapter 15: A Basic Clinical Asepsis Protocol
As discussed previously, infection control recommendations and regulations arise from many sources. In order to ensure the office infection control protocol is comprehensive, it is best to have one document that addresses all the issues, rather than separate protocols to comply with the different regulatory agencies. This chapter provides the groundwork with a sample clinical infection control protocol that is a starting point for a more comprehensive and office-specific document.
Each dental practice should develop a protocol that includes items specific to that office. Factors that may affect the protocol include state and local regulations, the types of dental procedures that the office performs and the duties allowed of the allied health professionals in the office.
Sample Infection Control Office Policy
Infection Control Policy and Procedures
I. General Guidelines
This policy reflects the minimum standards for infection control observed by all individuals providing patient care in our dental practice. Additional policies and practices apply as indicated by current best infection control practices recommended by the Centers for Disease Control and Prevention (CDC), or other public health and regulatory agencies.
A. Standard Precautions
This office uses Standard precautions in the treatment of all patients. This means we treat the blood and other body fluids of all patients as if potentially infectious. Standard precautions apply to all body fluids, excretions, and secretions with the exception of sweat.
B. Personal Protective Equipment
Personal protective equipment that does not permit blood or other potentially infectious materials to pass through or to reach employee's work clothes, street clothes, undergarments, skin, eyes, mouth, or other mucous membranes under normal conditions or for duration of time that the protective equipment will be used will be provided by the employer at no cost to employees. The use of personal protective equipment is required whenever there is potential for occupational exposure to blood or other potentially infectious materials (e.g., saliva or blood).
1. Gloves
This office uses disposable exam gloves whenever there is potential for hand contact with mucous membranes, blood, saliva, or instruments and equipment contaminated with patient body fluids. All employees involved in contact with the patient wear sterile surgical gloves for all surgical procedures.
Workers change gloves as soon as practical when contaminated and as soon as feasible when torn or punctured or when their ability to function as a barrier is compromised. It is not acceptable to wash or decontaminate single use gloves for re-use.
2. Masks and Protective Eyewear
Masks in combination with eye protection, such as goggles, glasses with side shields, or chin-length plastic face shields shall be worn whenever splashes, spray, splatter, or droplets of blood or other potentially infectious materials may be generated and eye, nose, or other mouth contamination can reasonably be anticipated. A new mask is used for each patient. Disinfect eyewear between each use.
3. Protective Clothing
If blood or saliva is present in spray or droplets during a procedure, all workers use long-sleeve protective gowns or lab coats. For most dental procedures, a lab coat is sufficient. The material used in the covering prevents blood or saliva from contacting work clothes, street clothes, skin and any other attire.
C. Hepatitis B Vaccination
All employees with occupational exposure to blood or other potentially infectious materials are encouraged to receive the hepatitis B vaccination. The vaccination is available to all at-risk employees at no charge to employees within ten days of first assignment. All employees at risk of occupational exposure to potentially infectious materials will first receive information regarding occupational risk for hepatitis B and the safety and efficacy of the vaccine. If the employee does not wish to receive the vaccine, they must complete and sign the mandatory hepatitis B declination form. If any employee that declines the vaccination series later changes their mind, the vaccine remains available at no cost to the employee provided they continue to have occupational exposure. If the employee has received the vaccine from a source other than the employer, that employee must provide written verification of dates of vaccines or sign a declination form indicating the vaccine is unnecessary. This information is in the employees' confidential medical record.
D. Occupational Exposure Follow-up
If an employee receives an accidental exposure (eye, mouth, mucous membrane, non-intact skin, or puncture) from a contaminated source, report it immediately to _______________. If skin is involved, wash the exposed area with soap and water. Treat the surrounding skin with an antiseptic to further cleanse the site. If the exposure is to mucous membranes, flush the affected area with copious amounts of water. Complete an exposure incident report form and obtain referral to a physician for follow-up. The employer and/or the Worker's Compensation carrier will pay all expenses for post-exposure testing and treatment. The employer will keep the medical records required by the Bloodborne Pathogens standard for the length of employment plus 30 years.
The employer will ask the source patient to submit to testing for HIV, hepatitis B, and hepatitis C. The cost of such testing will be borne by the employer.
II. Chairside
A. Instrument Asepsis
1. Critical Instruments: Instruments and equipment that penetrate bone or soft tissue will be heat sterilized or disposed of following each use.
2. Semicritical Instruments: Instruments and equipment that come into contact with oral tissues or fluids without penetrating tissue will be heat sterilized when possible. If heat sterilization is not feasible for these items, disinfect with a hospital level tuberculocidal disinfectant according to label instructions.
3. Noncritical Instruments: Instruments that contact only intact skin but may become contaminated during patient treatment require intermediate or low level disinfectant between patients.
All critical and semicritical instruments will be packaged before sterilization and remain packaged until ready for use. Sterilization will be verified through use of a biological indicator (spore test) completed weekly. Individual packages will monitored using a chemical indicator such as autoclave tape or color-change indicator on the packaging.
B. Handwashing
Perform handwashing before donning gloves, and after removing gloves. For surgical procedures, all workers use anti-microbial soap. If hand contact with patient care equipment or patient's body fluids is likely, use latex exam gloves to protect skin from direct contact. If tear or puncture of glove occurs, remove gloves, wash hands, and wear a new pair of gloves. Never wash or disinfect exam or surgical gloves for reuse. If an employee with occupational exposure has a documented allergy to latex, or other component of exam gloves, the employer will provide hypoallergenic gloves at no cost to the employee.
C. Handling of Personal Protective Equipment
Change masks between patients and whenever they become moistened. Change gowns daily or more often if visibly soiled. Laundering of the gowns is at the expense of the dentist, or disposable gowns may be used. Employees may not take home gowns or lab coats for laundering. Remove all personal protective equipment prior to leaving the work areas.
D. General Asepsis
During patient treatment, maintain a constant awareness of cross-contamination. Avoid touching objects and areas during patient treatment that cannot be easily decontaminated. Use equipment barriers when deemed appropriate and change the barriers between each patient. Plastic overgloves are useful to protect exam gloves when handling objects or surfaces during patient treatment with the exam gloves. Counter tops are kept free of excessive materials and containers to reduce the likelihood of cross contamination.
Flush dental unit lines with air or water for two minutes at the beginning of each day, prior to attaching handpieces, air/water syringes, or ultrasonic scalers. Flush lines for 30 seconds between each patient. If a system shown to be effective in control of biofilm is in use, do not perform flushing, as it will not be necessary unless using a product that specifically requires it. Eating, drinking, smoking, applying cosmetics and lip balm, and handling contact lenses is prohibited in patient treatment areas and areas which may contain surfaces or objects contaminated with the blood or saliva of patients. These areas include treatment rooms, sterilization areas, and dental laboratory areas.
E. Accident Prevention
To prevent accidental exposure to blood or saliva, minimize handling of contaminated sharp instruments and equipment. Perform all instrument transfers in a safe manner. Do not manually recap needles, but recap either by using the one-handed scoop technique or by use of a recapping device that does not require the person recapping the needle to place a hand in front of the used needle.
F. Engineered Sharps Injury Protection
When available and shown effective, use engineered sharps protection devices such as self-sheathing needles in connection with dental procedures. The entire team evaluates new devices as they become available. A representative number of employees from each category whose job duties include handling of contaminated sharps will be included in the evaluation process.
G. Clean-up of Treatment Room
Remove all equipment barriers after each patient. It is not necessary to disinfect these areas. Disinfect unprotected contaminated surfaces according to the following method:
1. Spray surface or a paper towel with cleaner/ disinfectant.
2. Wipe with paper towel to remove debris.
3. Spray with disinfectant; allow to stand for recommended time. (Usually 10 minutes.)
H. Waste Disposal
Discard disposable items used during patient treatment into a lined garbage container. Remove the liner each time the garbage is disposed of. The person handling the garbage will wear exam gloves to prevent accidental exposure to blood or saliva. If the items contain tissues, blood, or other potentially infectious materials that may be released if compressed, or fluid blood or saliva, they will be collected in a container dedicated to biohazard waste. That container must be red and labeled with the universal biohazard symbol.
Discard disposable contaminated sharps as soon as possible into a sharps container. Sharps containers are puncture resistant, leak proof on sides and bottom, labeled with the universal biohazard symbol and the legend "biohazard." They are available in the treatment rooms and trayroom/laboratory. Disposable sharps include needles, blades, wires, glass, and other objects capable of puncturing skin. Close sharps containers when they become full. All waste is disposed of in accordance with state and local regulations governing the transport, treatment, and disposal of biohazard waste.
III. Sterilization/Tray/Room
A. Instrument Sterilization
Instruments which penetrate bone or soft tissue must be either disposed of or heat sterilized following use. These are critical instruments. Semicritical instruments are those that contact oral fluids and tissue, but do not necessarily penetrate tissues (i.e., mouth mirror and amalgam carrier). These items should also be heat sterilized following use, unless it is not possible due to the design of the item. In this case, immerse in a chemical sterilant/disinfectant for the time required by the manufacturer to achieve sterilization. Noncritical instruments and items are those that do not enter the oral cavity, but may become contaminated during patient treatment (i.e., x-ray heads). If the item cannot be heat sterilized, disinfection with a chemical germicide, which is EPA-registered as an intermediate-level disinfectant and labeled tuberculocidal, is appropriate.
Wear personal protective equipment, including heavy-duty rubber gloves, eye protection, and gown when processing used instruments. Place instruments in an ultrasonic cleaner or washer/disinfector for cleaning. Upon removal, carefully dry instruments and place in a pouch for sterilization. If instrument cassettes are used, process the entire cassette with the instruments remaining in the cassette. Avoid hand-scrubbing instruments. Restrict hand scrubbing to those times when mechanical cleaning fails to remove all debris. If this is necessary, wear the heavy-duty gloves and scrub instruments individually in order to avoid accidental injury. During sterilization, place the pouches (or cassettes) in a single layer or loosely on their sides in the sterilizer. Process the instruments for the appropriate length of time at proper temperature and pressure. Verification of sterilization is achieved through the use of biological indicators (spore tests) conducted weekly. Monitor individual packages of instruments through the use of process indicators such as autoclave tape and color-change indicators on pouches.
Disinfect instrument trays in the same manner as equipment and surfaces, using the spray-wipe-spray technique described earlier.
Alternatively, use disposable trays or plastic covers for single patient use.
IV. X-ray and Darkroom
The following protocol minimizes the risk of cross-contamination during x-ray procedures.
1. Assemble x-ray films, film holders and cup, and place equipment barriers before donning gloves or while wearing clean gloves.
2. Drape patient with x-ray shield.
3. Put on exam gloves.
4. Take x-rays, placing each in a paper cup following exposure.
5. When all x-rays have been exposed, remove gloves, wash hands, and place cup of x-rays in the daylight loader.
6. Wearing clean gloves, place hands through sleeves of daylight loader, open all film packets allowing film inside packet to drop onto a clean surface without touching the films.
7. Remove gloves.
8. Process films with bare hands. Because the films have not been touched with contaminated gloves or contacted oral tissues, no special precautions are necessary when mounting processed films.
9. Remove plastic barriers from x-ray equipment. Disinfect the surfaces that were touched during the procedure and were unprotected by barriers.
X-ray films with barrier packs may be used. Remove the barriers immediately after exposure of the x-ray, place all films in a clean cup, and remove gloves before processing or handling the films.
Note: for digital radiographs, the x-ray sensor and all equipment touched during the procedure is protected with impervious barriers, which are changed between each patient.
V. Laboratory Asepsis
A. Impressions
Rinse impressions to remove blood and saliva before decontamination. Spray or immerse impressions in an EPA-registered tuberculocidal disinfectant for at least 10 minutes. The impressions may then be poured up in stone or plaster, or sent to the dental laboratory off-site.
B. Prostheses and Crowns
Disinfect prostheses and temporary crowns before being inserted into the patient's mouth and after removal from the patient's mouth.
C. Lathe Pans and Wheels
Lathe pan, rag wheels, etc. should be maintained in a clean condition and disinfected regularly. Disinfect items before manipulation in the laboratory and disinfect prostheses before insertion into the patient's mouth.
VI. Blood and Body Fluid Spills
Clean spills containing blood or body fluids using absorbent material. Personnel conducting the cleanup will wear gloves and protective attire. Decontaminate the area of the spill by washing with a dilute bleach solution. Mix the bleach solution fresh for each use in a mixture of one part bleach to ten parts water.
BIBLIOGRAPHY AND SELECTED REFERENCES
General Recommendations
Bolyard EA, Tablan OC, Williams WW, Pearson ML, Shapiro CN, Deitchman SD, Hospital Infection Control Practices Advisory Committee. Guideline for infection control in health care personnel, 1998. Am J Infect Control 1998;26:289--354.
CDC. Guidelines for prevention of transmission of human immunodeficiency virus and hepatitis B virus to health-care and public-safety workers: a response to P.L. 100-607 The Health Omnibus Programs Extension Act of 1988. MMWR 1989;38(suppl No. 6S).
US Department of Labor, Occupational Safety and Health Administration. 29 CFR Part 1910.1030. Occupational exposure to bloodborne pathogens; needlesticks and other sharps injuries; final rule. Federal Register 2001;66:5317--25. As amended from and includes 29 CFR Part 1910.1030. Occupational exposure to bloodborne pathogens; final rule. Federal Register 1991;56:64174--82. Available at http://www.osha.gov/SLTC/dentistry/index.html.
US Department of Labor, Occupational Safety and Health Administration. OSHA instruction: enforcement procedures for the occupational exposure to bloodborne pathogens. Washington, DC: US Department of Labor, Occupational Safety and Health Administration, 2001; directive no. CPL 2-2.69.
US Department of Labor, Occupational Safety and Health Administration. 29 CFR 1910.1200. Hazard communication. Federal Register 1994;59:17479.
CDC. Immunization of health-care workers: recommendations of the Advisory Committee on Immunization Practices (ACIP) and the Hospital Infection Control Practices Advisory Committee (HICPAC). MMWR 1997;46(No. RR-18).
CDC. Updated U.S. Public Health Service guidelines for the management of occupational exposures to HBV, HCV, and HIV and recommendations for postexposure prophylaxis. MMWR 2001;50(No. RR-11).
CDC. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care facilities, 1994. MMWR 1994;43(No. RR-13).
Smart ER, Macleod RI, Lawrence CM. Allergic reactions to rubber gloves in dental patients: report of three cases. Br Dent J 1992;172:445--7.
Cleveland JL, Robison VA, Panlilio AL. Tuberculosis epidemiology, diagnosis and infection control recommendations for dental settings: an update on the Centers for Disease Control and Prevention guidelines.J Am Dent Assoc. 2009 Sep;140(9):1092-9.
Kanjirath PP, Coplen AE, Chapman JC, Peters MC, Inglehart MR. Effectiveness of gloves and infection control in dentistry: student and provider perspectives. J Dent Educ. 2009 May;73(5):571-80.
Policy on infection control.American Academy on Pediatric Dentistry Clinical Affairs Committee-Infectious Disease Control Subcommittee; American Academy on Pediatric Dentistry Council on Clinical Affairs. Pediatr Dent. 2008-2009;30(7 Suppl):85.
OSAP. Creating a successful infection control program. Dent Assist. 2008 Nov-Dec;77(6):19-22, 24-6, 30-1.
Smith A, Creanor S, Hurrell D, Bagg J, McCowan M.Management of infection control in dental practice. J Hosp Infect. 2009 Apr;71(4):353-8.
Boyce R, Mull J.Complying with the Occupational Safety and Health Administration: guidelines for the dental office. Dent Clin North Am. 2008 Jul;52(3):653-68.
Herd S, Chin J, Palenik CJ, Ofner S.The in vivo contamination of air-driven low-speed handpieces with prophylaxis angles. J Am Dent Assoc. 2007 Oct;138(10):1360-5.
OSAP.OSAP'S safety and infection control report card. Dent Assist. 2006 Nov-Dec;75(6):6-10.
Basquill LC, Govoni M, Bednarsh H.OSHA--what is its role in dentistry and how do we provide training? Compend Contin Educ Dent. 2005 Mar;26(3 Suppl):10-3.
Palenik CJ.An overview of OSHA training for dentistry. Compend Contin Educ Dent. 2005 Mar;26(3 Suppl):6-8.
Weissenbock, H. (2010). Zoonotic mosquito-borne flaviviruses; Worldwide presence of agents with proven pathogenicity and potential candidates of future emerging diseases. Veterinary Microbiology 140 (3-4), pages 271-280.
Globally Harmonized System of Classification and Labelling of Chemicals (Second revised ed.), New York and Geneva: United Nations, 2007, ISBN 978-92-1-116957-7, ST/SG/AC. 10/30/Rev.2 ("GHS Rev.2")
Latex Hypersensitivity
American Dental Association Council on Scientific Affairs. The dental team and latex hypersensitivity. J Am Dent Assoc 1999;130:257--64.
CDC. National Institute for Occupational Safety and Health. NIOSH Alert: preventing allergic reactions to natural rubber latex in the workplace. Cincinnati, OH: US Department of Health and Human Services, Public Health Service, CDC, National Institute for Occupational Safety and Health, 1997.
Hamann CP, Turjanmaa K, Rietschel R, et al. Natural rubber latex hypersensitivity: incidence and prevalence of type I allergy in the dental professional. J Am Dent Assoc 1998;129:43--54.
Bloodborne Disease Transmission
Werner BG, Grady GF. Accidental hepatitis-B-surface-antigen-positive inoculations: use of e antigen to estimate infectivity. Ann Intern Med 1982;97:367--9.
Shapiro CN. Occupational risk of infection with hepatitis B and hepatitis C virus. Surg Clin North Am 1995;75:1047--56.
Cleveland JL, Siew C, Lockwood SA, Gruninger SE, Gooch BF, Shapiro CN. Hepatitis B vaccination and infection among U.S. dentists, 1983--1992. J Am Dent Assoc 1996;127:1385--90.
CDC. Recommendations for preventing transmission of human immunodeficiency virus and hepatitis B virus to patients during exposure-prone invasive procedures. MMWR 1991;40(No. RR-8).
US Department of Labor, Occupational Safety and Health Administration. 29 CFR Part 1910.1030. Occupational exposure to bloodborne pathogens; final rule. Federal Register 1991;56:64004--182.
Cleveland JL, Gooch BF, Shearer BG, Lyerla RL. Risk and prevention of hepatitis C virus infection: implications for dentistry. J Am Dent Assoc 1999;130:641--7.
Gruninger SE, Siew C, Azzolin KL, Meyer DM. Update of hepatitis C infection among dental professionals [Abstract 1825]. J Dent Res 2001;80:264.
Ciesielski C, Marianos D, Ou CY, et al. Transmission of human immunodeficiency virus in a dental practice. Ann Intern Med 1992; 116:798--805.
Ashkenazi M, Fisher N, Levin L, Littner MM. Seroepidemiology of hepatitis C antibodies among dentists and their self-reported use of infection control measures. Community Dent Health. 2009 Jun;26(2):99-103.
Azarpazhooh A, Fillery ED. Prion disease: the implications for dentistry. J Endod. 2008 Oct;34(10):1158-66
Cristina ML, Spagnolo AM, Sartini M, Dallera M, Ottria G, Lombardi R, Perdelli F. Evaluation of the risk of infection through exposure to aerosols and spatters in dentistry. Am J Infect Control. 2008 May;36(4):304-7
Redd JT, Baumbach J, Kohn W, Nainan O, Khristova M, Williams I.Patient-to-patient transmission of hepatitis B virus associated with oral surgery. J Infect Dis. 2007 May 1;195(9):1311-4. Epub 2007 Mar 21. Erratum in: J Infect Dis. 2007 Jun 15;195(12):1874
Immunization
CDC. Hepatitis B virus: a comprehensive strategy for eliminating transmission in the United States through universal childhood vaccination: recommendations of the Immunization Practices Advisory Committee (ACIP). MMWR 1991;40(No. RR-13).
Needlestick Prevention and Response
CDC. National Institute for Occupational Safety and Health. NIOSH alert: Preventing needlestick injuries in health care settings. Cincinnati, OH: US Department of Health and Human Services, Public Health Service, CDC, National Institute for Occupational Safety and Health, 1999.
Cleveland JL, Gooch BF, Lockwood SA. Occupational blood exposure in dentistry: a decade in review. Infect Control Hosp Epidemiol 1997; 18:717--21.
Gooch BF, Cardo DM, Marcus R, et al. Percutaneous exposures to HIV--infected blood among dental workers enrolled in the CDC needlestick study. J Am Dent Assoc 1995;126:1237--42.
CDC. National Institute for Occupational Safety and Health. Selecting, evaluating, and using sharps disposal containers. Cincinnati, OH: US Department of Health and Human Services, Public Health Service, CDC, National Institute for Occupational Safety and Health, 1998. DHHS publication no. (NIOSH) 97-111.
Hecht N, Wettan S.Percutaneous injuries. J Am Dent Assoc. 2007 May;138(5):574.
Cleveland JL, Barker LK, Cuny EJ, Panlilio AL; National Surveillance System for Health Care Workers Group.Preventing percutaneous injuries among dental health care personnel. J Am Dent Assoc. 2007 Feb;138(2):169-78
Hand Hygiene
CDC. Guideline for hand hygiene in health-care settings: recommendations of the Healthcare Infection Control Practices Advisory Committee and the Field EA, McGowan P, Pearce PK, Martin MV. Rings and watches: should they be removed prior to operative dental procedures? J Dent 1996;24:65--9.
DeGroot-Kosolcharoen J, Jones JM. Permeability of latex and vinyl gloves to water and blood. Am J Infect Control 1989;17:196--201.
Murray CA, Burke FJ, McHugh S. An assessment of the incidence of punctures in latex and non-latex dental examination gloves in routine clinical practice. Br Dent J 2001;190:377--80.
Adams D, Bagg J, Limaye M, Parsons K, Absi EG. A clinical evaluation of glove washing and re-use in dental practice. J Hosp Infect 1992;20:153--62.
Myers R, Larson E, Cheng B, Schwartz A, Da Silva K, Kunzel C. Hand hygiene among general practice dentists: a survey of knowledge, attitudes and practices. J Am Dent Assoc. 2008 Jul;139(7):948-57.
Disinfection/Sterilization
Spaulding EH. Chemical disinfection of medical and surgical materials [Chapter 32]. In: Lawrence CA, Block SS, eds. Disinfection, sterilization and preservation. 5th Edition. Philadelphia, PA: Lippincott Williams & Wilkins, 2001: 517--31.
CDC. Guidelines for environmental infection control in health-care facilities: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC). MMWR 2003;52(No. RR-10).
Favero MS, Bond WW. Chemical disinfection of medical and surgical material [Chapter 43]. In: Block SS, ed. Disinfection, sterilization and preservation. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2001:881--917.
Miller CH, Tan CM, Beiswanger MA, Gaines DJ, Setcos JC, Palenik CJ. Cleaning dental instruments: measuring the effectiveness of an instrument washer/disinfector. Am J Dent 2000;13:39--43.
Joslyn LJ. Sterilization by heat [Chapter 36]. In: Block SS, ed. 5th ed. Disinfection, sterilization, and preservation. Philadelphia, PA: Lippincott Williams & Wilkins, 2001:695--728.
CDC. National Institute for Occupational Safety and Health. Glutaraldehyde: occupational hazards in hospitals. Cincinnati, OH: US Department of Health and Human Services, Public Health Service, CDC, National Institute for Occupational Safety and Health, 2001. DHHS publication no. (NIOSH) 2001-115.
Miller CH, Sheldrake MA. The ability of biological indicators to detect sterilization failures. Am J Dent 1994;7:95--7.
Rutala WA, Web DJ . Disinfection and Sterilization in Health Care Facilities: What Clinicians Need to Know.Clin Infect Dis 2004;39:702-709.
Rutala WA, Web DJ, HICPAC. Guideline for Disinfection and Sterilization in HealthCare Facilities-2008. CDC. Nov. 2008.
Ghahramanloo A, Sadeghian A, Sohrabi K, Bidi A. A microbiologic investigation following the disinfection of irreversible hydrocolloid materials using the spray method. J Calif Dent Assoc. 2009 Jul;37(7):471-7.
Wu G, Yu X. Influence of usag history, instrument complexity, and different cleaning procedures on th e cleanliness of blood-contaminated dental surgical instruments. Infect Control Hosp Epidemiol. 2009 Jul;30(7):702-4.
Regulated Waste
Palenik CJ. Managing regulated waste in dental environments. J Contemp Dent Pract 2003;4:76.
Rutala WA, Mayhall CG. Medical waste. Infect Control Hosp Edidemiol 1992;13:38--48.
Dental Waterline Contamination
Williams JF, Johnston AM, Johnson B, Huntington MK, Mackenzie CD. Microbial contamination of dental unit waterlines: prevalence, intensity and microbiological characteristics. J Am Dent Assoc 1993;124:59--65.
Mills SE. The dental unit waterline controversy: defusing the myths, defining the solutions. J Am Dent Assoc 2000;131:1427--41.
Clark A. Bacterial colonization of dental units and the nasal flora of dental personnel. Proc Roy Soc Med 1974;67:1269--70.
Fotos PG, Westfall HN, Snyder IS, Miller RW, Mutchler BM. Prevalence of Legionella-specific IgG and IgM antibody in a dental clinic population. J Dent Res 1985;64:1382--5.
Reinthaler FF, Mascher F, Stunzner D. Serological examinations for antibodies against Legionella species in dental personnel. J Dent Res 1988;67:942--3.
Shearer BG. Biofilm and the dental office. J Am Dent Assoc 1996; 127:181--9.
Walker JT, Marsh PD.Microbial biofilm formation in DUWS and their control using disinfectants. J Dent. 2007 Sep;35(9):721-30.
Pankhurst CL, Coulter WA.Do contaminated dental unit waterlines pose a risk of infection? J Dent. 2007 Sep;35(9):712-20.
Cross Contamination
Gooch B, Marianos D, Ciesielski C, et al. Lack of evidence for patient-to-patient transmission of HIV in a dental practice. J Am Dent Assoc 1993;124:38--44.
Crawford JJ, Broderius C. Control of cross-infection risks in the dental operatory: preventon of water retraction by bur cooling spray systems. J Am Dent Assoc 1988;116:685--7.
Lewis DL, Arens M, Appleton SS, et al. Cross-contamination potential with dental equipment. Lancet 1992;340:1252--4.
Kuehne JS, Cohen ME, Monroe SB. Performance and durability of autoclavable high-speed dental handpieces. NDRI-PR 92-03. Bethesda, MD: Naval Dental Research Institute, 1992.
Filho IB, Esberard RM, Leonardo R, del Rio CE. Microscopic evaluation of three endodontic files pre- and post instrumentation. J Endodontics 1998;24:461--4.
Laboratory Asepsis
Chau VB, Saunders TR, Pimsler M, Elfring DR. In-depth disinfection of acrylic resins. J Prosthet Dent 1995;74:309--13.
Powell GL, Runnells RD, Saxon BA, Whisenant BK. The presence and identification of organisms transmitted to dental laboratories. J Prosthet Dent 1990;64:235--7.
Giblin J, Podesta R, White J. Dimensional stability of impression materials immersed in an iodophor disinfectant. Int J Prosthodont 1990;3:72--7.
Plummer KD, Wakefield CW. Practical infection control in dental laboratories. Gen Dent 1994;42:545--8.
Al-Jabrah O, Al-Shumailan Y, Al-Rashdan M. Antimicrobial effect of 4 disinfectants on alginate, polyether, and polyvinyl siloxane impression materials. Int J Prosthodont. 2007 May-Jun;20(3):299-307.
For added information
HYPERLINK "https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2018-vol-30.pdf" Diagnoses of HIV infection in the United States and dependent areas, 2018 pdf icon. HIV Surveillance Report 2019;30. Retrieved from: https://www.cdc.gov/hiv/statistics/overview/ataglance.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fhiv%2Fstatistics%2Fbasics%2Fataglance.html
Global Health Observatory (GHO) data
Retrieved from: https://www.who.int/gho/hiv/en/
HIV and Pregnant Women, Infants, and Children Retrieved from: https://www.cdc.gov/hiv/group/gender/pregnantwomen/index.html
Dental Practice Management, (2015). Retrieved from: http://practicemanagement.dentalproductsreport.com/article/nitrous-oxide-what-dental-assistants-need-know?page=0,1