You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Before recent developments in dental science and technology, all materials used to restore teeth—for example, amalgam, gold, and porcelain—were inert (had no interaction with the tooth structure) and did not offer any benefit to the surrounding tissues, other than to occupy the space left after decay removal and the completion of tooth preparation.1 With new materials that have been developed, the situation has changed.
Conventional Direct Dental Restorative Materials
In regard to direct restorative materials, comparing dental amalgam with composite resins, the placement of composite requires many more steps and a precise technique to achieve optimal clinical results. The process of adhesion includes etching the dentin and enamel followed by application of primers and adhesives, and in some cases, layering of composite resins to complete the restorative process. For many clinical situations, the clinician must also deal with challenges related to operator access and moisture control, as well as soft tissue-related problems (bleeding or excessive gingival tissue) that often arise with restorations where margin placement is at or below the level of the marginal gingival tissues. When composite resins are placed in layers, several independent steps are required to complete the restorative process; associated with them is the potential for clinical problems, such as voids and marginal leakage, which ultimately can lead to recurrent decay and restoration failure.2
The complexity of performing the steps required to place composite resins contrasts sharply with the requirements for dental amalgam, although both necessitate the use of a matrix system to restore anatomic proximal contours and contact areas and prevent proximal gingival overhangs for Class II restorations. For amalgam placement, a Class II procedure, most clinicians typically use a Tofflemire-type matrix to contain the restorative material, which is then condensed into the cavity preparation. Next, using a carving instrument, the restoration is sculpted into anatomic tooth form. Finally, the occlusion (bite) is checked with articulating paper, and the restorative material is adjusted to accommodate the occlusion.3
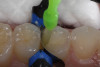
With composites, however, the clinician must first control the operating environment using isolation techniques, such as a rubber dam or other dental isolation system. The operative area is isolated to control moisture contamination and a specially designed matrix system is used-ie, a sectional matrix. Composite resin, when placed, requires (1) etching; (2) rinsing; (3) drying; (4) desensitizing; (5) placement of adhesive; (6) light-curing; (7) placing a base or liner, if needed; (8) light-curing; (9) placing the increment of composite; and (9) light-curing. Several increments may be placed and cured before final sculpting of the occlusal surface of the restoration, checking and adjusting the bite, and then placing an optional surface sealant to protect the marginal areas of the composite restoration. One potential clinical benefit of bonded composite resins is that, unlike dental amalgam, these materials by virtue of enamel and dentin bonding (adhesion) have the potential to seal the tooth-restorative interface more effectively long-term than their metallic counterparts.4
Giomers: A Class of "Smart" Direct Restorative Materials
Composite resins are made up of glass fillers that are ground to a very small particle size, often less than 1 μm, and dispersed in a resin matrix (bisphenol A-glycidyl methacrylate [BisGMA]) to hold these particles together and to attach or bond in a micromechanical fashion to the prepared tooth structure. Many advances have been made over the last several decades in both the esthetics and functionality of these materials; many of these materials are now being used for the restoration of both anterior and posterior teeth. As advances in materials science have expanded the use of composite resins clinically, the emphasis has been on clinical parameters such as polymerization shrinkage, polymerization shrinkage stress, bulk fill, luster retention, and handling. The composite material known as a Giomer, which incorporates these advances, has implemented an additional step to provide actual ion exchange with the microenvironment around the restoration to affect the biofilm (the ability to adhere to tooth structure and restorative materials) and pH (buffering acid attack), assisting in the protection of the restorative material and prevention of early breakdown, particularly for patients who may not have optimal oral hygiene habits.5
The Giomer class of direct composite restorative materials has the unique feature of a stable, surface pre-reacted glass filler (S-PRG) coated with an ionomer layer in a BisGMA resin matrix. This arrangement allows protection of the glass core from moisture, providing long-term esthetics and durability of conventional composites as well as ion release and recharge capabilities. Other benefits of Giomer technology, according to the manufacturer, include (1) forming an acid-resistant layer that can transpose to adjacent teeth; (2) neutralization of acids to help establish a stable pH in the oral microenvironment; (3) inhibiting biofilm formation and disrupting mature biofilm; (4) exhibiting anti-plaque properties by reducing plaque formation and bacterial adherence; and (5) exhibiting caries prevention, with the potential for secondary caries prevention.6,7
"Replacement" dentistry accounts for a significant amount of the dental services provided in a typical dental practice. Contrary to what was taught to most dentists in school, dental restorations do not typically last forever even when placed ideally. Marginal breakdown and recurrent decay have always been processes by which many dental restorations will ultimately fail and require replacement-and not always at the fault of the material used. One factor that could potentially increase long-term clinical success of a dental restorative material would be to find a mechanism by which the materials themselves would help slow down or interfere with the attraction of pellicle or plaque to tooth structure or help buffer the deleterious effects of bacterial-acid metabolism on the loss of calcium and phosphate ions from healthy tooth structure. It is well-documented in the literature that glass-ionomers work by releasing fluoride ions to help make tooth structure more resistant to acid attack. However, because of their degree of solubility, there is often only a short period that fluoride protection can be available.8-10
As mentioned, Giomer products contain a unique S-PRG filler within the composite resin matrix. These fillers consist of a glass core that has been pre-reacted with a polyacrylic acid solution. The glass-ionomer phase in Giomer fillers that is coated on the pre-reacted glass is protected from water sorption and early degradation by the addition of a surface-modified layer on top. Therefore, ion exchange can occur from a Giomer-containing composite material, providing the ability to help prevent plaque accumulation and help buffer or neutralize acid by-products of bacterial metabolism for extended periods over the life of the Giomer restoration. Giomers can be especially effective in caries-prone individuals, who often exhibit extreme periods of acid challenge to unrestored teeth and the tooth-marginal interfaces of restored teeth.11,12
Clinical Challenges for Successful Placement of Direct Composite Restorations
Establishing proximal contacts and anatomic interproximal contours for Class II and Class III composite restorations, while eliminating voids between layers and improving both predictability and time efficiency in placement, remain as significant challenges when placing direct composite restorations.13
Recurrent decay—the No. 1 cause of composite failure—is often traced to voids where horizontal and vertical walls of the cavity preparations meet-the line angles and point angles that are most vulnerable to incomplete filling because of the inability to condense composite resins. Although good cavosurface marginal adaptation can be verified visually in some areas of the restoration, the incremental placement process, along with the etching and bonding between layers, relies largely on "blind faith" that the preparation has been completely filled geometrically. Voids cannot be detected radiographically unless they are in the same directional plane as the x-ray beam.14
The traditional method of composite placement in 2-mm increments or less was meant to facilitate complete curing and to minimize any potential negative effects of polymerization shrinkage. The technique of layering, however, causes a greater potential to introduce voids into the restoration just by the nature of placement. Bulk-fill flowable composites have been developed as dentin replacements and can be cured in increments of up to 4 mm, based on manufacturer recommendations. Although these materials have the potential to eliminate some of the voids by decreasing the number of layers in the restoration, they are typically not designed with the physical properties required to withstand forces of occlusion and, because of the emphasis on depth of cure, are usually more translucent; therefore, an additional increment (enamel layer) of a nanohybrid composite material is required to complete the restoration.15
Reproducing Interproximal Contact and Contour for Class II Composite Restorations
In most clinical situations, Tofflemire-type universal matrix systems that are used for amalgam are not recommended for use with composite resins. A variety of sectional matrices designed specifically to reproduce the proximal contact and also the proximal contour of the tooth are now commercially available. The matrix band is placed between the prepared surface and adjacent interproximal surface; after placement of an anatomic wedge to seal the gingival margin, a ring is placed over the wedge and between the teeth to gently secure the matrix and push the teeth apart, ensuring the creation of an interproximal contact and allowing ideal anatomic placement of the composite material to replicate the convex contour of the natural interproximal tooth surface. When a sectional matrix is placed correctly, very little finishing with rotary instruments should be required.16
Filling Technique and Depth of Cure: How These Factors Affect Clinical Success
According to a study by Campodonico et al, depth of cure, rather than filling technique (bulk versus incremental fill), is the main issue facing practitioners using today's composite restorative materials.17
Direct composite resin restorations are typically placed by most clinicians with an incremental placement technique. This technique was required in the earlier days of composite resin use because the materials of that period shrank considerably (more than 3% by volume). In approximately the last decade, materials science has reduced the shrinkage of composite resins during placement significantly. But because polymerization shrinkage is still considered an issue, and taking into account that there may be an inability to light-cure composite materials adequately beyond a certain depth due to opacity of the material and other factors, it has been generally recommended to place composite resin in increments of 2 mm or less. The question is, with advances in polymer chemistry, photo activation, and curing-light technologies with today's composite resin materials and curing lights, is this still a common clinical problem? Several studies have been done, some as early as 2001, that compare incremental versus bulk-fill placement of composite, showing that there is no clinically significant difference in cuspal deflection (moving cusps together) or marginal integrity (opening marginal gaps) when comparing bulk versus incremental placement. A more important clinical issue with bulk-fill materials and techniques appears to be the depth of cure. It is also important to mention that directional curing from the buccal and lingual (palatal) aspects after removal of the matrix system helps to increase the ability to cure composite resin at the gingival levels of the preparation in deeper Class II restorations.18-20
Selection of Materials Available for Direct Composite Placement
One of the advantages clinicians have today is the wide variety of materials available to handle most clinical situations encountered in the everyday practice of dentistry. A disadvantage is that although many materials are available, it is easy for a dentist to gravitate toward "what works best in my hands" or to "which material is on special this month." More than ever, it is important in today's practice of dentistry to "be the doctor!" The dentist should choose the material that is best for the patient and tooth in the specific clinical situation that presents. What is the patient's caries risk assessment? Does the patient have a mouth full of multi-surface restorations, or is the patient relatively restoration-free? Does the patient maintain regular re-care visits or come in only when something hurts? What is the quality and quantity of the saliva? How effective is the patient's home care at maintaining plaque removal? All these criteria should influence the type of restorative material that is selected.
Heavy-Bodied Flowable Composites and Bulk-Fill Flowable Composites as Dentin Replacements
Heavy-bodied flowable composites were designed to be used to restore conservative Class I, Class II, Class III, and Class V cavity preparations. For microdentistry (slot and fissurotomy preparations), flowable composites are necessary because conventional instrumentation is too large to adequately condense a paste composite into such a small space (Figure 1 through Figure 6).21
Bulk-fill flowable composites were first introduced to the dental marketplace in 2011. These materials are indicated for use as a bulk-fill dentin replacement and are designed to be placed in a single increment of up to 4 mm in depth. An increment of that thickness (4 mm) is a significant time savings in placement and curing of each layer because it reduces the number of potential layers of the standard 2-mm increment thickness by half. Although this concept sounds advantageous, a material must meet several important factors for this type of indication. These factors include (1) increased depth of cure, (2) a viscosity that readily adapts to the internal geometry of the cavity preparation without the need for extra manipulation of the material, and (3) low polymerization shrinkage and polymerization shrinkage stress. In conservative Class II slot preparations, it may be possible to use some bulk-fill flowable composites for the entire restoration (Figure 7 through Figure 11).22
Because of their decreased opacity and decreased percentage of fillers to allow deeper penetration of the curing light, bulk-fill flowable composites, in most cases, require a conventional nanohybrid composite material to be placed as the final (occlusal) increment. A new bulk-fill flowable composite was recently introduced to the market that, based on manufacturer claims, has a 4-mm depth of cure and does not require a capping layer.23-25
Nanohybrid Composite Technologies
Nanohybrid and nanofilled paste composites that are typically used for tooth-colored restorative procedures are more highly filled and polishable than previous generations of composite materials because of advances in polymer chemistry and materials science. These materials are often called universal because they can be used in the posterior regions as well as in anterior, esthetic areas of the oral cavity. Many of these restoratives contain nanofiller technology and are formulated with Nanomer and nanocluster filler particles. Nanomers are separate, discrete nano-agglomerated particles of 20 to 75 nm in size, and nanoclusters are loosely bound agglomerates of nano-sized particles. The combination of Nanomer-sized particles and nanocluster formations reduces the spacing of the filler particles, thus creating the ability to increase filler capacity (better physical properties) while still having the ability to polish extremely well (less plucking, smoother surfaces). Nanohybrids therefore have improved physical properties over the earlier generations of microhybrid composites, while having increased luster and polish retention (Figure 12 through Figure 19).26-28
Bulk-Fill Composite Resins (Paste Type)
Bulk-fill composite materials in general are helping to simplify the placement of composite restorations by decreasing the number of increments that need to be placed and individually cured during the restorative process. Similar to bulk-fill flowable composites, paste-type bulk-fill materials can also be placed in up to 4-mm increments, as opposed to conventional composite materials (2 mm). The composition of paste-type bulk-fill composites must therefore be altered to allow increased depth of cure while having less shrinkage and shrinkage stress than conventional composite materials. One way to achieve a greater depth of cure has been to increase the amount of the existing photo initiator or use a combination of different photo initiators to allow increased depth of cure. Different monomers and elastic fillers have also been developed that minimize the shrinkage and shrinkage stress when the material is cured. The result of providing a deeper depth of cure, however, is often to have to settle for a more translucent, less "chameleon-like" quality to the material. Nevertheless, in most clinical situations, this is more of a problem for the dentist than it is for the patient. One of the challenges in making a bulk-fill material has been to have an opacity that retains the esthetic quality of the material without compromising the depth of cure (Figure 20 through Figure 25).29
Low-Shrink Composites
As previously mentioned, polymerization shrinkage of composite resins has been a clinical topic of discussion for a long time. Many failures of composite materials may have been attributed to the shrinkage of the resin during the curing phase, opening a gap between the composite and the tooth where bacterial access could lead to microleakage and recurrent decay. A goal of materials science has been to create a material whose polymer does not shorten or shrink during the photopolymerization phase of the restorative process, thus eliminating one potential cause of restorative failure. The amount that a composite resin will shrink varies greatly and can depend on the type of monomer used, the type and amount of fillers, and how the fillers and the resin matrix interact. Manufacturing modifications made to composites to reduce polymerization shrinkage may include (1) increasing the filler load while decreasing the amount of monomer; (2) incorporation of pre-polymerized fillers, which maintain their volumetric dimension, thereby reducing shrinkage; and (3) using monomers of higher molecular weights, which shrink less. Many dental manufacturers have responded by producing low-shrink composites that help to minimize the potential negative effects of polymerization and polymerization shrinkage stress (Figure 26 through Figure 30).30
Conclusion
One of the goals in the creation of new composite materials is to simplify the placement of direct composite resins without compromising the quality of the final result. Trying to recreate natural tooth structure with manmade materials is challenging. Yet advances are being made to allow clinicians to deliver high-quality restorations using direct tooth-colored restorative materials that can give patients a functionally esthetic, long-lasting result. Also, materials science continues to develop and refine tooth-colored filling materials that are more biologically harmonious with natural teeth and are "smart" in that they can contribute to protecting both teeth and restorations. Giomer technology incorporated into direct restorative materials gives the clinician a material that does more than just fill teeth: it also provides biologic benefits that can potentially extend the life of the restoration and the tooth. The Giomer line of restorative materials includes bulk-fill (flowable and paste) options along with conventional and low-shrink nanohybrid materials; an appropriate Giomer material is available for every clinical situation. Other materials options that aid in not only preserving but rebuilding damaged teeth continue to be developed as restoratives continue to become "smarter."
About the Author
Robert A. Lowe, DDS
Diplomat, American Board of Aesthetic Dentistry
Charlotte, North Carolina
References
1. Mjör IA, Hensten-Pettersen A, Skogedal O. Biologic evaluation of filling materials. A comparison of results using cell culture techniques, implantation tests and pulp studies. Int Dent J. 1977;27(2):124-129.
2. Juloski J, Carrabba M, Aragoneses JM, et al. Microleakage of Class II restorations and microtensile bond strength to dentin of low-shrinkage composites. Am J Dent. 2013;26(5):271-277.
3. Bayne SC, Heymann HO, Swift EJ Jr. Update on dental composite restorations. J Am Dent Assoc. 1994;125(6):687-701.
4. Rodrigues SA Jr, Pin LF, Machado G, et al. Influence of different restorative techniques on marginal seal of class II composite restorations. J Appl Oral Sci. 2010;18(1):37-43.
5. Nakamura N, Yamada A, Iwamoto T, et al. Two-year clinical evaluation of flowable composite resin containing pre-reacted glass-ionomer. Pediatr Dent J. 2009;19(1):89-97.
6. Tamura D, Saku S, Yamamoto K, Hotta M. Saliva protein which adsorbs to composite resin containing S-PRG filler. The Japanese Society of Conservative Dentistry. 2010;53(2):191-206.
7. Saku S, Kotake H, Scougall-Vilchis RJ, et al. Antibacterial activity of composite resin with glass-ionomer filler particles. Dent Mater J. 2010;29(2):193-198.
8. Izono T, Saku S, Yamamoto K. Application to the tooth coating material of the glass filler containing acid reactive fluoride. The Japanese Society of Conservative Dentistry. 2009;52(3):237-247.
9. Tech profile: Beautifil Flow Plus. Inside Dentistry. 2011;7(2):108.
10. Gordan VV, Blaser PK, Watson RE, et al. A clinical evaluation of a Giomer restorative system containing surface prereacted glass ionomer filler: results from a 13-year recall examination. J Am Dent Assoc. 2014;145(10):1036-1043.
11. Naoum S, Ellakwa A, Martin F, Swain M. Fluoride release, recharge and mechanical property stability of various fluoride-containing resin composites. Oper Dent. 2011;36(4):422-432.
12. Itota T, Al-Naimi OT, Carrick TE, et al. Fluoride release from aged resin composites containing fluoridated glass filler. Dent Mater. 2005;21(11):1033-1038.
13. Sarrett DC. Clinical challenges and the relevance of materials testing for posterior composite restorations. Dent Mater. 2005;21(1):9-20.
14. Purk JH, Dusevich V, Glaros A, Eick JD. Adhesive analysis of voids in Class II composite resin restorations at the axial and gingival cavity walls restored under in vivo versus in vitro conditions. Dent Mater. 2007;23(7):871-877.
15. Say EC, Civelek A, Nobecourt A, et al. Wear and microhardness of different resin composite materials. Oper Dent. 2003;28(5):628-634.
16. Patras M, Doukoudakis S. Class II composite restorations and proximal concavities: clinical implications and management. Oper Dent. 2013; 38(2):119-124.
17. Campodonico CE, Tantbirojan D, Olin PS, Versluis A. Cuspal deflection and depth of cure in resin-based composite restorations filled by using bulk, incremental and transtooth-illumination techniques. J Am Dent Assoc. 2011;142(10);1176-1182.
18. Rees JS, Jagger DC, Williams DR, et al. A reappraisal of the incremental packing technique for light cured composite resins. J Oral Rehabil. 2004;31(1):81-84.
19. Flury S, Hayoz S, Peutzfeldt A, et al. Depth of cure of resin composites: is the ISO 4049 method suitable for bulk fill materials? Dent Mater. 2012;28(5):521-528.
20. El-Safty S, Silikas N, Akhtar R, Watts DC. Nanoindentation creep versus bulk compressive creep of dental resin-composites. Dent Mater. 2012;28(11):1171-1182.
21. Bonilla ED, Stevenson RG, Caputo AA, White SN. Microleakage resistance of minimally invasive Class I flowable composite restorations. Oper Dent. 2012;37(3):290-298.
22. Ilie N, Bucuta S, Draenert M. Bulk-fill resin-based composites: an in vitro assessment of their mechanical performance. Oper Dent. 2013;38(6):618-625.
23. Van Ende A, De Munck J, Van Landuyt KL, et al. Bulk-filling of high C-factor posterior cavities: effect on adhesion to cavity-bottom dentin. Dent Mater. 2013;29(3):269-277.
24. Roggendorf MJ, Krämer N, Appelt A, et al. Marginal quality of flowable 4-mm base vs. conventionally layered resin composite. J Dent. 2011;39(10):643-647.
25. Rodrigues SA Jr, Ferracane JL, Della Bona A. Flexural strength and Weibull analysis of a microhybrid and a nanofill composite evaluated by 3- and 4-point bending tests. Dent Mater. 2008;24(3):426-431.
26. Curtis AR, Palin WM, Fleming GJ, et al. The mechanical properties of nanofilled resin-based composites: characterizing discrete filler particles and agglomerates using a micromanipulation technique. Dent Mater. 2009;25(2):180-187.
27. Beun S, Glorieux T, Devaux J, et al. Characterization of nanofilled compared to universal and microfilled composites. Dent Mater. 2007;23(1):51-59.
28. Yapp R, Powers JM. Depth of cure of several composite restorative materials. Dent Advis Res Rpt. 33:1, February 2011.
29. Alrahlah A, Silikas N, Watts DC. Post-cure depth of cure of bulk fill dental resin-composites. Dent Mater. 2014;30(2);149-154.
30. Ilie N, Jelen E, Clementino-Luedemann T, Hickel R. Low-shrinkage composite for dental application. Dent Mater J. 2007;26(2):149-155.