You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Introduction
Head and neck or oral cancers rank sixth as the most common cancer, worldwide.1 According to the International Statistical Classification of Diseases and Related Health Problems (ICD CM-10) definition, oral and oropharyngeal cancers are grouped based on their site of occurrence which includes cancers of lip, tongue, buccal mucosa, alveolar ridge and gingiva, floor of mouth, tonsils, hard and soft palate, oropharynx and/or other unspecified parts of mouth.2 The American Cancer Society estimated that 53,260 new cases of oral and oropharyngeal cancers (OC) were diagnosed in the United States in 2020 with over 10,750 deaths.3 The 5-year survival rate of OC in the United States is 60%, with significant improvement for survival with early detection.4 In the state of Wisconsin, an estimated 990 new cases of OC were projected for 2019, with 200 deaths due to OC.5 Tobacco use is considered a common risk factor for oral cancer6 along with alcohol consumption, combined use of alcohol and tobacco use, and human papilloma virus (HPV).7-9 Disease severity, complications of treatment, length of recovery, and prognosis of survival can be influenced by a patient's insurance status or ability to pay for oral health care at the time of OC diagnosis.10 Individuals who are uninsured or underinsured are less likely to receive preventive health care and early detection of OC compared with individuals who have health and or dental insurance.10 Studies have shown that oral cancer risks can be modified by targeting factors that include improving public awareness and reducing barriers to care surrounding oral cancer.7,9,11 Shimpi et al. surveyed patients at a large medical-dental health system serving a rural population located in central, northern and western Wisconsin and found that while 94% of patients were aware that tobacco use increases OC risk, 79% were unable to correctly identify other oral cancer risk factors.11 Furthermore, participants in these rural settings demonstrated low knowledge surrounding additional signs and symptoms of OC including an abnormal mass/lump in mouth, sore that does not heal, white/red patches, difficulty chewing/swallowing and gradual change in voice quality.11
Although the American Dental Association (ADA) recommends routine visual and tactile examinations for oral and oropharyngeal cancer for all patients during a dental visit,12 individuals living in rural areas are less likely to receive routine OC preventive education and screenings due to a lack of health and dental resources compared with individuals residing in urban areas.13-15 Screening and education programs surrounding oral cancer at public events have the potential to reach individuals who might not routinely receive preventive head and neck examinations and oral cancer screenings such as those who reside in rural areas.16,17
Approximately one in every nine jobs in the state of Wisconsin are related to agriculture.18,19 The purpose of this study was to collect information related to oral cancer awareness, offer education and provide oral cancer screenings at an educational farming event in the state of Wisconsin.
Methods
This study was granted exempt status by the Marshfield Clinic Research Institute's Institutional Review Board. Participants were recruited among a convenience sample of attendees at the 2018 Wisconsin Farm Technology Days (WFTD) Exposition, an educational farming event held annually at different dairy farms throughout the state. The 2018 WFTD took place in Wood County, a designated Dental Health Professional Shortage Area (DHPSA).20 Flyers were distributed among Marshfield Clinic Health System (MCHS) employees and at various community locations to notify the public of the opportunity to participate in this study and have an oral cancer screening. The study was also advertised in the official WFTD program distributed at the event.
Instruments and data collection
Members of the study team randomly invited WFTD attendees, 18 years of age and older, to complete a voluntary, anonymous paper-based survey and to participate in an oral cancer screening examination. Participants had the option to only complete the survey or only have the oral cancer screening or to complete both aspects of the study.
The investigator-produced survey was written at a 5th grade readability level and consisted of 12 items. The survey instrument was pilot tested by ten random MCHS staff members unfamiliar with professional dental terminology and a statistician and dentist conducted face validity of the survey instrument. The survey items included socio-demographics, knowledgeability, and social practice behaviors surrounding oral cancer. The socio-demographic questions captured study participants farming status, age, gender, level of completed education, and oral cancer history. The two questions related to oral cancer knowledge consisted of identifying risk factors associated with oral cancer and identifying signs and symptoms of oral cancer. Social practice behaviors included professional dental-care frequency, dental/health insurance status, and historic behavioral habits surrounding alcohol and tobacco use. Pilot testing demonstrated that a non-dental professional could complete the survey in 5 to 7 minutes.
Oral cancer screenings and recording instrument
Six licensed dental hygienists were calibrated by the research team for performing oral cancer screening to ensure uniform data collection. During calibration, each dental hygienist identified photographs of healthy oral tissue or oral lesions according to guidelines provided by the National Institute of Dental and Craniofacial Research (NIDCR) and ADA oral cancer screening guidelines.22,23 A video available from ADA demonstrating oral cancer screening methodologies and protocols was also used as a training and calibration tool.24 The dental hygienists performed two separate oral cancer screenings and documented the findings on three volunteers to achieve inter and intra-rater reliability score of 100%.
Participants read and signed a waiver providing an explanation of the OC screening process. The screenings consisted of visual and tactile examination of twelve areas of the oral cavity including: the submandibular lymph nodes, lips, labial mucosa, buccal mucosa, gingiva, tongue (dorsum, ventral, and lateral borders), floor of mouth, hard and soft palates, and oropharynx as per NIDCR and ADA clinical guidelines.22,23 An oral cavity graphic on the oral cancer screening form served as a mouth map to document oral lesions along with a table containing each of the twelve oral cavity locations under the graphic. For each location in the oral cavity, the screening instrument contained a box to mark for "normal" indicating no oral lesion was present at that anatomic location. If an oral lesion was present, a research assistant would mark the size (≤2mm or ≥3mm); color (red or white); contour (ulcer, raised, smooth, rough); and duration of lesion (≤2 weeks or ≥3 weeks).
Each screening participant received one of three pre-determined written follow-up recommendations. The survey instrument and oral cancer screening forms had corresponding numbers for each study participant in order to establish relationships between the survey instrument data and the OC screening data. No identifiers were collected to link individual participants to consent forms, personal information or screening outcomes. Upon completion of the screening, participants received a copy of the signed waiver form; a follow-up recommendation form; pertinent oral health literature; and a complimentary toothbrush.
Oral cancer education
An informational poster board displayed at the oral cancer booth provided information regarding oral cancer risk factors, oral cancer prevention, and oral cancer signs and symptoms. Dental hygienists explained the screening process and recommended annual visual and tactile head and neck examinations as additional opportunity to educate study participants on OC. Printed material from the National Institute of Dental and Craniofacial Research on signs, symptoms, and prevention of oral cancer23 as well as information on Wisconsin tobacco Quit Line (WIQuitLine.org)25 were available. In addition, information regarding Wisconsin's free and reduced cost dental clinics was also provided for individuals who did not have a dental home.26
Data analysis and reporting
Responses to the surveys and the screening results were manually entered into a REDCap database.27 A 10% validation was performed by second data entry personnel to validate the accuracy of the data entered. Data was then converted into statistical software formatted datasets (SAS Windows 9.4, SAS Institute Inc., Cary, NC).27 Rates of missing data were reported for each question and number of actual responses for each question was represented in the denominator to indicate that missing data elements were not included in final analysis. For the purpose of this study, tobacco use included cigarettes, cigars, pipes, e-cigarettes, vaping, smokeless tobacco, snuff, and snus.
Descriptive statistics (for any categorical measurements: percentage and corresponding 95% confidence interval (CI); for continuous variables: mean, standard deviation, median, and range) were reported for data surrounding measurements (e.g., alcoholic drinks consumed per week) as well as categorical measurements including participants sociodemographic descriptors (e.g., age, gender, education level). Education levels were categorized as I=(less than 1 year of schooling, completed grades 1-8, and/or completed grades 9-12 with no diploma), II=(High school diploma or equivalent, some college with no degree, and/or associate degree), III=(bachelor's degree, master's degree, professional degree, and/or doctorate degree).
Fisher's Exact test was performed to compare the difference in percentages of reported responses: (a) actively farming (defined as yes versus no), (b) categories of patients' age groups (18-40 years, 41-60 years, 61-89 years), (c) gender, (d) education level, (e) duration since last dental visit, (d) previous oral cancer diagnosis, (e) insurance status, (f) OC knowledge, (g) tobacco status, (h) type of tobacco products used, (i) reported frequency of alcohol use. In addition, Chi square test and odds ratio (ORs) with 95% CI were estimated to examine knowledge concerning specific risk factors in association with OC (defined as ‘yes' versus ‘no') by using unconditional univariate logistic regression analysis. P-values were derived and values of <0.05 were considered statistically significant.
Results
Demographics
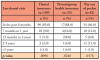
A total of 236 individuals participated in this study, with 82% (n=193) also consenting for oral cancer screening; 43% of the participants (n=102) were male and 55% (n=130) were female. Over three-fourths of the participants (78%, n=186) were between the ages of 51-80 years old and nearly one-quarter (24%, n=56) identified themselves as farmers. Less than half (46%) reported having dental insurance and they majority (82%) reported paying ‘out of pocket' for dental care. Eleven percent reported having private or group health (medical) insurance, 22% qualified for Medicare, and 4% had Medicaid. Participant demographics are shown in Table I.
Most study participants (96%, n=226) did not have a previous history of oral cancer and frequently sought routine dental care as evidenced by (84%, n=198) seeking oral care services within the last year. Seventy-two percent (n=169) had seen their dental provider for routine care within the last six months, with only 4% reporting a dental visit more than 2 years earlier. Seventy-two percent of participants with Education level II (n=161) reported having a dental visit in the last six months compared to 75% (n=38) with Education level III. Very few participants (5%, n=11) reported Education level I or reported not having a high school diploma. Of the individuals who routinely sought dental care, fewer than half had dental insurance (46%, n=109). Frequency of dental visits and modes of payment are shown in Table II.
Tobacco use
Of the 233 participants who responded to the tobacco use questions, 83% (n=195) reported never having used tobacco products, with 12% (n=29) reporting a history of using tobacco products in the past, and 4% (n=9) reporting current use of tobacco. Twelve percent (n=7) of participants who were active farmers (n=56) reported current or former tobacco use and nearly three-quarters (73%, n=27) of the current or former tobacco users had Education level II.
Alcohol use
When questioned about alcohol consumption, 65% (n=154) of participants reported some alcohol consumption. Eighty-five percent (n=126) of participants reported consuming less than or equal to four drinks a week and 14% (n=21) of participants reported consuming more than four drinks per week. Notably, most participants with Education Level III (80%, n=41) reported consuming alcohol, whereas 60% (n=99) of participant's with Education Level II reported alcohol consumption (p=0.0196).
Oral cancer knowledge and awareness
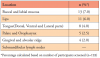
Over one third (35%, n=84) of participants identified at least one risk factor for oral cancer, while 46% (n=110) identified two or more risk factors for oral cancer. Correct identification of the various risk factors for OC by the participants is shown in Table III. Only 10% (n=4) of the participants who reported current or former tobacco use correctly identified all the risk factors for oral cancer, and 31% (n=12) of them identified all signs and symptoms of the oral cancer. Over half (65%, n=153) of the participants correctly identified two or more signs/symptoms of oral cancer, while 19% (n=44) correctly identified at least one sign/symptom of oral cancer. Participants' identification of oral cancer risk factors, signs and symptoms is shown in Table II.
Oral cancer screening
A total of 193 participants consented for oral cancer screening (n=193). Oral lesions were found in 17% (n=33) of the participants, with 52% (n=17) of this group being male. The locations of the lesions identified through the oral cancer screenings are shown in Table IV. Thirty percent (n=10) of the participants with oral lesions correctly identified at least two risk factors for oral cancer, and 42% (n=14) of the participants correctly identified all the signs and symptoms of oral cancer. Seventy percent (n=23) of the participants with visible lesions reported having seen a dentist in the past six months, and 36% (n=12) of them had dental insurance. Twenty-one percent (n=7) with visible lesions were current or former tobacco users and two-thirds (66%, n=22) reported alcohol consumption. Of the individuals with oral lesions, 65% (n=20) were encouraged to see a dental provider for routine oral examination; 32% (n=10) were advised to have a 2-week follow-up with a dental provider; and 3% (n=1) was advised to seek immediate care.
Discussion
Individuals residing in rural communities are considered an "at-risk" population for health concerns due to the remote location of work and home life.12,14,22 Determining a population's OC awareness, providing education, and offering OC screenings through a community outreach event, such as a farming exposition, represents a potentially effective venue for educating individuals on medical and/or dental care.16,17 Schroeder et al. found during a rural community oral health screening that while the majority of study participants sought routine dental care and engaged in adequate oral home care, they still found value with having an oral health screening and in being able to speak with an oral health professional regarding dental concerns at community events.15
Dental care utilization
Research supports routine preventive oral cancer examinations to increase early detection and early treatment of oral cancer, thereby improving oral cancer survival.17,26 Inconsistencies in oral cancer prognosis have been attributed to barriers to oral care access, low oral health literacy, and lack of oral cancer awareness.11,28,29 Shin et al. examined the records of patients diagnosed with oral pharyngeal squamous cell carcinoma to determine if insurance status played a role in oral cancer outcomes.10 Patients with private insurance were
more likely to seek preventive care, receive an early cancer diagnosis, and have a better prognosis than those who were uninsured or underinsured.10 Based on the findings in this study, the WFTD study participants appeared to seek routine preventive oral health care regardless of insurance status.
Tobacco use
A high percentage of study participants (71%) correctly identified smoking as a risk factor for oral cancer and the majority (96%) reported either never using or no longer using tobacco products, significantly lower than the national average of tobacco users.30 The Centers for Disease Control (CDC) reported approximately 18% of men and 13% of women in the United States use tobacco products.30 Analysis of patient records (n=4,759) obtained from the International Head and Neck Cancer Epidemiology (INHANCE) Consortium revealed smoking status and smoking intensity at the time of diagnosis of head and neck cancer was a reliable factor in determining oral cancer outcomes.31
Alcohol use
Study participants reported low use of alcohol, with the majority reporting drinking four or less alcoholic beverages per week. Of the participants with visible oral lesions, 66% reported alcohol consumption. The National Institute on Alcohol Abuse and Alcoholism defines low alcohol consumption for women as less than 3 drinks per day but no more than 7 drinks per week.32 For men, low alcohol consumption is considered no more than four drinks per day but less than 14 drinks per week.32 Study participants with Education Level III reported consuming alcohol more frequently than those with Education Level I or Education Level II. Alcohol use and intensity has been shown a significant factor for poor oral cancer outcomes and mortality rate.31 A 2017 cohort population study used data from 83,006 participants from five different studies to determine whether alcohol consumption was related to years of education and mortality rate.31 Findings revealed that individuals with high education levels consumed more alcohol overall than those with lower education levels.31
Oral cancer knowledge awareness
Male study participants identified risks associated with oral cancer more frequently (46%) than females (28%). This aligns with previous studies showing that men tend to be more knowledgeable about oral cancer risk factors than their female counterparts.14 The National Institute for Health reported that men are twice as likely as women to be diagnosed with oral cancer.1 Low rates of knowledge were demonstrated in this study surrounding oral cancer risk factors such as alcohol consumption and combined tobacco and alcohol use. As with a study conducted by Shimpi et al.,11 the most readily identifiable risk factor for oral cancer by the participants in this study was smoking. Participants also had low levels of knowledge regarding the signs and symptoms of oral cancer.
Oral cancer screening data
The buccal mucosa and the lips were the most common areas where lesions were detected in this population. A 2017 cohort study by Kachuri et al. evaluated cancer risks in agricultural workers in Canada from 1992-2010.32 Cancer of the lip was significantly higher for agricultural workers than non-farm workers conceivably due to sun exposure,33 which may also be reflected in this population.
Interventions
Varela-Centelles et al. conducted a systematic review representing individuals diagnosed with oral cancer (n=6,087) to disseminate the key steps and potential delays that occur from initial recognition of an oral lesion to when treatment begins.17 Survival rates were better when cancer was detected and treated during the early stages.17 Methods of reducing barriers for individuals residing in rural communities included improving access to preventive care services and offering public screening and education events.17 Findings from the WFTD 2018 oral cancer screening study also supports outreach programs to individuals residing in rural communities to bring awareness and knowledge surrounding oral cancer. School-based education programs surrounding tobacco, drug, and alcohol prevention and cessation have been shown to be effective methods at deterring youth from using these products.34 Many school based tobacco, drug, and alcohol prevention programs are available but need to be incorporated into the school curriculum in order to be effective.34
Individuals who seek routine medical care but not routine dental care are still in need of oral cancer screenings, education, and interventions through their health care provider.16,17,28,29 The primary care provider has the opportunity to be the first line of defense for identifying risk behaviors for oral cancer and oral lesions related to oral cancer. Studies have shown medical providers who offer oral health assessments and promptly refer patients to a dental provider can help improve patient willingness to seek dental care and improve oral and systemic health outcomes.16,29,35,36
Study limitations
This study encountered certain limitations due to the design, location, self-administration of the study, and participant demographics. Since Wood County, Wisconsin tends to be a primarily Caucasian population, race/ethnicity of study participants were not collected.37 Incomplete participation in the survey tool in combination with the oral cancer screening for all study participants resulted in statistical limitations. Other limitations in the sample size included a lack of participation incentives and poor weather conditions at the time of the event.
This community event in a rural setting had the potential to obtain significant information surrounding the oral cancer knowledge, awareness, and risk factors specific to farmers. The study instrument asked participants if they were ‘actively farming,' which excluded those who may have been raised on a farm or who were retired from farming. More study participants might have been considered a ‘farmer' if the survey tool specified ‘ever having been a farmer or resided on a farm.' More research studies are needed to determine oral and systemic health care needs and interests specific to the farming community. As with other studies involving health screenings, researchers were unable to follow-up with study participants to determine if the screening process was effective. Future studies which have a follow-up component is important to determine if public health screenings are in fact beneficial for early detection and improved OC outcomes.
Conclusions
Positive treatment outcomes for oral cancer increase if detected early during preventive head and neck examinations performed during routine oral health care visits. Individuals residing in rural communities might be at risk for late detection of oral cancer due to lack of access to oral health care. While participants in this study were receiving routine oral health care, they lacked knowledge regarding OC risk factors, signs, and symptoms indicating the need for additional methods to provide oral cancer awareness and knowledge during routine oral and medical examinations. Oral cancer intervention programs beginning in secondary and high school and continuing into college and university curriculums might also be an effective preventive care strategy.
Acknowledgements
The authors would like to thank the following dental hygienists and dental assistants from Marshfield Clinic Health System Family Health Centers (FHC): Stacey Bisenius, Katherine Mann, Linda Aden, Shoua Thao, Kristie Virden, Crystal Brings, and Megan Hintz for their work with the oral screenings and education program. The authors would also like to thank Yvonne Cerne and Dixie Schroeder from the Center for Oral and Systemic Health (COSH), Marshfield Clinic Research Institute (MCRI), for assisting with the planning at Wisconsin Farm Tech Days, Annie Steinmetz and Ingrid Glurich from COSH, MCRI for reviewing the manuscript, and to Greg Nycz from FHC and Patti Bell from Marshfield Clinic Health System for their overall contributions to this project.
Kelly Schroeder, RDH, MSis a national outreach specialist, DentaQuest, Boston, MA, USA. Aloksagar Panny, BDS, MSis a research specialist; Neel Shimpi, BDS, MM, PhD, FAMIAis an associate research scientist; both at the Marshfield Clinic Research Institute, Center for Oral and Systemic Health, Marshfield, WI, USA.
References
1. NIH. Oral cancer-Fact sheets [Internet]. Bethesda (MD): National Institutes of Health; 2020 [cited 2021 Jun 14]. Available from: https://seer.cancer.gov/statfacts/html/oralcav.html
2. WHO. International Statistical Classification of Diseases and Related Health Problems 10th Revision [Internet]. Geneva (CH): World Health Organization (WHO); 2010. [cited 2021 Jun 14]. Available from: https://www.who.int/classifications/icd/ICD10Volume2_en_2010.pdf
3. ACS. Cancer Facts and Figures [Internet]. Atlanta (GA): American Cancer Society; 2019. [cited 2019 July 25]. Available from: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf
4. NICDR. Oral Cancer 5-Year Survival Rates by Race, Gender, and Stage of Diagnosis [Internet]. Bethesda (MD): National Institute of Dental and Craniofacial Research; 2018. [cited 2021 Jun 14]. Available from: https://www.nidcr.nih.gov/research/data-statistics/oral-cancer/survival-rates
5. ACS. Cancer statistics center, Wisconsin 2018 Estimates [Internet]. Atlanta (GA): American Cancer Society; 2018. [cited 2021 Jun 14]. Available from: https://cancerstatisticscenter.cancer.org/#!/state/Wisconsin
6. Chaturvedi P, Singh A, Chien CY, Warnakulasuriya S. Tobacco related oral cancer. BMJ. 2019 Jun 5;365:I2142.
7. Mathur S, Conway DI, Worlledge-Andrew H, et al. Assessment and prevention of behavioral and social risk factors associated with oral cancer: Protocol for a systematic review of clinical guidelines and systematic reviews to inform primary care dental professionals. Syst Rev. 2015 Dec 22:184.
8. Mello FW, Melo G, Pasetto JJ, et al. The synergistic effect of tobacco and alcohol consumption on oral squamous cell carcinoma: a systematic review and meta-analysis. Clin Oral Investig. 2019 Jul;23(7):2849-59.
9. Raj AT, Patil S, Gupta AA, et al. Reviewing the role of human papillomavirus in oral cancer using the Bradford Hill criteria of causation. Dis Mon. 2019 Jun;65(6):155-63.
10. Shin JY, Yoon JK, Shin AK, Diaz AZ. The influence of insurance status on treatment and outcomes in oral cavity cancer: an analysis on 46,373 patients. Int J Oral Maxillofac Surg. 2018 Oct 1; 47(10):1250-7.
11. Shimpi N, Jethwani M, Bharatkumar A, et al. Patient awareness/knowledge towards oral cancer: a cross-sectional survey. BMC Oral Health. 2018 May 15;18(1):86.
12. Versaci MB. ADA expands policy on oral cancer detection to include oropharyngeal cancer [Internet]. Chicago (IL): American Dental Association; 2019 [cited 2020 Nov 12]. Available from: https://www.ada.org/en/publications/ada-news/2019-archive/september/ada-expands-policy-on-oral-cancer-detection-to-include-oropharyngeal-cancer
13. Skillman SM, Doescher MP, Mouradian WE, Brunson DK. The challenge to delivering oral health services in rural America. J Public Health Dent. 2010 Jun;70 Suppl 1:S49-57.
14. Pickett W, King N, Trask C, et al. Factors related to self-perceived health in rural men and women. J Agromedicine. 2015 Apr 3; 20(2):178-87.
15. Schroeder K, Gurenlian J, Portillo K. The oral health needs of Wisconsin farmers and the need for patient activation: a pilot study. J Agromedicine. 2017;22(3):235-43.
16. Brocklehurst P, Kujan O, O'Malley L, et al. Screening programmes for the early detection and prevention of oral cancer. Cochrane Database Sys Rev. 2013 Nov 19;2013(11):CD004150.
17. Varela-Centelles P, Lopez-Cedrun JL, Fernandez-Sanroman J, et al. Key points and time intervals for early diagnosis in symptomatic oral cancer: a systematic review. Int J Oral Maxillofac Surg. 2017 Jan 1;46(1):1-10.
18. DATCP. Wisconsin agricultural statistics [Internet]. Madison (WI): State of Wisconsin; 2021. [cited 2021 Jun 14]. Available from: https://datcp.wi.gov/Pages/Publications/WIAgStatistics.aspx
19. Wisconsin Farm Bureau Federation. Wisconsin farm facts [Internet]. Madison (WI): Wisconsin Farm Bureau Federation; 2015. [cited 2021 Jun 14]. Available from: https://wfbf.com/wp-content/uploads/2015/03/Wisconsin-Farm-Facts-2015-web.pdf
20. WIORH. Health professional shortage area: dental health care [Internet]. Madison (WI); Wisconsin Office of Rural Health; 2020. [cited 2021 Jun 14]. Available from: http://worh.org/library/health-professional-shortage-area-dental-health-care-0
21. ADA. Oral Cancer [Internet]. Chicago (IL): American Dental Association; 2020 [cited 2021 Jun 14]. Available from: https://www.mouthhealthy.org/en/az-topics/o/oral-cancer
22. NICDR. Detecting oral cancer: a guide for health care professionals [Internet]. Bethesda (MD): National Institute of Dental and Craniofacial Research; 2013 [cited 2021 Jun 14]. Available from: https://www.nidcr.nih.gov/sites/default/files/2017-09/detecting-oral-cancer-poster.pdf
23. UW Center for Tobacco Research and Intervention. Wisconsin tobacco quit line [Internet]. Madison (WI): Wisconsin Department of Health; 2019 [cited 2021 Jun 14]. Available from: https://quitline.wisc.edu/
24. DHS. Free or low cost health clinics [Internet]. Madison (WI): Wisconsin Department of Health Sciences; 2019 [cited 2021 Jun 14]. Available from: https://www.dhs.wisconsin.gov/forwardhealth/clinics.htm
25. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr;42(2):377-81.
26. Kupzyk KA, Cohen MZ. Data validation and other strategies for data entry. West J Nurs Res. 2015 Apr 19;37(4):546-56.
27. Shepperd JA, Howell JL, Logan H. A survey of barriers to screening for oral cancer among rural Black Americans. Psychooncology. 2014 Mar;23(3):276-82.
28. Messadi DV. Diagnostic aids for detection of oral pre-cancerous conditions. Int J Oral Sci. 2013 Jun;5(2):59-65.
29. CDC. Current cigarette smoking among adults in the United States [Internet]. Atlanta (GA): Centers for Disease Control and Prevention; 2021[cited 2021 Jun 15]. Available from:https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm
30. Giraldi L, Leoncini E, Pastorino R, et al. Alcohol and cigarette consumption predict mortality in patients with head and neck cancer: a pooled analysis within the International Head and Neck Cancer Epidemiology (INHANCE) Consortium. Ann Oncol. 2017 Nov 1;28(11):2843-51.
31. NIAAA. Alcohol's effects on health [Internet]. Bethesda (MD): National Institutes of Health; 2021. [cited 2021 Jun 14]. Available from: https://www.niaaa.nih.gov/alcohols-effects-health
32. Kachuri L, Harris MA, MacLeod JS, et al. Cancer risks in a population-based study of 70,570 agricultural worker: results from the Canadian census health and environment cohort (CanCHEC). BMC Cancer. 2017 Dec 19; 17(1):343.
33. Flay BR. School-based smoking prevention programs with the promise of long-term effects. Tob Induc Dis. 2009 Mar 26;5(1):6.
34. Ford PJ, Farah CS. Early detection and diagnosis of oral cancer: Strategies for improvement. J Cancer Policy. 2013 Mar 1; 1(1-2):e2-7.
35. Irani S. Pre-cancerous lesions in the oral and maxillofacial region: a literature review with special focus on etiopathogenesis. Iran J Pathol. 2016 Fall;11(4):303-22.
36. RHIhub. Oral health in rural communities [Internet]. Grand Forks (ND): Rural Health Information Hub; 2019. [cited 2021 Jun 14]. Available from: https://www.ruralhealthinfo.org/topics/oral-health