You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Giomer Technology combines characteristics of composite resins and glass-ionomers, containing particles of pre-reacted glass filler within the composite and resulting in quality function and esthetics.
A determination of parameters for patient selection requires an examination of the classes of marginal tissue recession as defined by Dr. P.D. Miller. A conservative approach to treating Class III and Class IV recession defects, per Miller, is possible utilizing a combination of pink and white Giomer Technology restorative materials. A Miller Class III features marginal tissue recession that extends to or beyond the mucogingival junction, with periodontal attachment loss in the interdental area or malpositioning of teeth, and a Miller Class IV features marginal tissue recession that extends to or beyond the mucogingival junction, with severe bone or soft tissue loss in the interdental area and/or malpositioning of teeth1 (Figure 1). Recommended parameters for proper patient selection relating to this type of procedure generally include the existence of Class III and/or Class IV recession.
Giomer Technology offers benefits in the treatment of advanced gingival recession and cervical lesions. The practitioner who does not have pink composite in their office should consider obtaining some, as it has many applications. Although the practitioner may not be familiar with Giomer Technology, with just a little time, energy, and focus, they will be able to use it with skill and offer greater benefits and options for patients, particularly those reluctant to engage in a large reconstruction.
Traditionally, practitioners have used white composite when augmenting areas, filling diastemas and black triangles. The evolution of pink Giomer offers added flexibility.
Case Presentation I: Severe Recession
As a practitioner, the author had Giomer materials in both white and pink, but had been employing them only for temporization. When placing an implant temporary or hybridization procedures, this practitioner would augment with pink composite up around the temporary to demonstrate esthetics of pink composite or pink ceramic.
Patient "Cody" presented after having been referred by another dentist. The original dentist had worked patient up for veneers, but decided they were not going to work because there was severe recession and attachment loss, and veneer margins would be on root tissue next to recessed tissues, potentially causing bondability problems. The patient had good enamel (Figure 2), which practitioners did not want to cut. However, the patient did not like the coloration of his teeth.
This practitioner discussed pink and white composites with patient, suggested whitening, and mocked up pink composite around the roots and took photos. Although Cody's case was an advanced one, this was the first such case this practitioner was going to attempt with pink composite and new technique, and the technology was new as well. The patient was pleased with the esthetics and wanted to proceed.
From teeth Nos. 22 to 27, the patient had Miller Class III defects. He also had some recession spots, other areas that were Miller Class I and Class II, and old crowns that needed correction.
The patient's Class I areas would have been easily graftable, with marginal tissue recession that did not extend to the mucogingival junction. The schematic drawing in Figure 1 shows little classic recession defects that are Class III, with marginal tissue recession that extends to or beyond the mucogingival junction with no attachment loss of bone or soft tissue in the interdental area.
Although this article does not focus on Class I and Class II cases, pink Giomers can be used for both. In a later follow-up visit, Cody asked for the application of pink Giomers in the Class I and Class II areas.
Before the development of pink Giomer, practitioners would often choose gingival grafting procedures. When looking at Class II and Class IV cases, practitioners cannot predictably expect to get very good root coverage when the interdental papilla has recessed to a severe degree. A Class III case may have marginal tissue recession that extends to or beyond the mucogingival junction with periodontal attachment loss in the interdental area, or malpositioning of teeth. In a lot of these cases, there is a combination. A Class IV would be marginal tissue recession that extends to or beyond the mucogingival junction with severe bone or soft tissue loss in the interdental area and/or malpositioning of teeth. A combination of pink and white is indicated in such cases. Filling areas with white alone may not look natural on long teeth. A good fill with pink and white will not allow as much bacterial interproximally because there will be less of a chance of calculus bridges and build-up in black triangles.
Dr. Ward Smalley of the University of Washington, an orthodontist and prosthodontist, recommends beginning the treatment planning process with a vision,2 and that is particularly important for working with Giomer Technology, because there may not be a simple answer as to how to treat a particular case and what the next step is. It is important to have a blueprint to establish a vision (Figure 3). Initiate a systematic treatment plan or evaluation for correction that includes esthetic, functional, structural, and biologic evaluation. Treat in the reverse order, going from biologic, to structural, to functional, to esthetic evaluation (Figure 4).
Clinicians must ask themselves questions such as: Is there another way here? Will this require a work-up for a veneer case? Could the treatment be more conservative? Explain the options so the patient can make an informed decision. Practitioners should also ask themselves: How conservative can they be with this case? How little can they touch the tooth structure and yet provide maximum benefit? One advantage of techniques using pink and white composite bonding is that they do not require any destructive reduction of teeth. They allow the most minimally invasive dentistry possible to optimize a positive outcome.
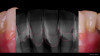
Figure 5 shows radiographs on Cody's anterior teeth that were indicated for treatment. His gingival recession and bone loss already had been classified, and he had already had orthodontics; Cody did not need orthodontics again, but it is an option in many such cases. Possible options were porcelain veneers on both the mandibular and maxillary teeth, porcelain crowns, and splinted bridges on the mandibular anterior-requiring compromising and removing a lot of tooth structure. Removal of mandibular incisors with implant placements was another option, as was a four unit bridge with or without orthodontic extrusion-knowing that as teeth are extruded, tissue and bone will be pulled with them as well.3
The patient did not want the latter options, but was amenable to composite boding. Periodontal splinting in conjunction with bonding is called for in some cases-when there are not good interproximal contacts, when the maxillary and/or mandibular teeth are loaded in different dimensions, and when they have diastemas.4-10 Obviously, the teeth can move because of decreased periodontal support. However, when the diastema is decreased, the periodontium stabilizes, which has to do with the bioactivity of the Giomer Technology materials.2,11-14 Some of these cases still need to be splinted.
Digital smile design (DSD) is indicated as it not only helps the practitioner, but serves as an educational tool for patients. The practitioner can show the patient's dentition on screen, draw lines to make some areas pink and some white, detailing for the patient where gums should be without ever touching a tooth.
In Cody's case, this practitioner freehanded some composite interproximally with some white, and then cervically and slightly interproximally with some pink, and patient and his wife were pleased. With practice, practitioners will blend the composites better and better. Using dark pigmentation to create better composite colors can be particularly important when working with patients of color or others with darker gums.
In the case of Cody, after doing the digital smile design, whitening was called for, and afterwards the patient was diligent with his hygiene. Before treatment, the patient presented with calculus, and so hygienist removed it before any other procedures, as teeth have to be clean at the beginning. Patient was augmented with white and pink. Figures 5 and 6, with Figure 5 showing the radiograph superimposed, show the progression. Procedures took only a few hours, and patient was so pleased he asked for additional improvements, which have included grafting and replacement of posterior crowns. Figure 6 was taken one-year post-treatment. Patient and his wife actually wrote a letter offering thanks for allowing Cody to feel proud of his smile for the first time in his life.
In such procedures, practitioners work in small zones with minimal room for error and the work is difficult, so it is very rewarding when patients are pleased. Giomer procedures are not expensive, costing less than veneers; it recommended, however, that the practitioner charge more for such high-level composite procedures than for traditional bonding procedures.
Case Presentation II: Class III Defects
Patient "Jen," age 42, presented with Class III defects (Figure 7) and had previously had a free gingival graft between tooth Nos. 24 and 25. Treatment options were porcelain veneers; porcelain crowns/porcelain bridge after splinting or with removal of tooth Nos. 24 and 25 and pontics; removal of mandibular central mandibular incisors with implant placements (variable placements and restorative options); and composite bonding with or without periodontal splinting.
In doing a DSD blueprint (Figure 8), several questions arose: How would teeth be laid out? If veneers were done, where would they go, and would veneer margins go down into the roots? How would the teeth be prepared? How achievable would insertion be? Would the porcelain veneers have some pink?
Composite bonding was the option chosen. The patient's teeth had some minor mobility, so the practitioner decided to tighten them via orthodontic arch wire splinting to hold them in place. They have done very well and now are not as mobile as before. See in the radiographic analysis where the pink and white is augmented (Figure 9). There were no issues with cleaning. Tissue healing was good. Practitioners must be very diligent about placing the materials and not leaving flash and excess.
What is a Giomer?
Giomer Technology refers to any product containing a proprietary filler particle engineered by Shofu Dental that has the ability to release and recharge six different ions: fluoride, sodium, strontium, aluminum, silicate, and borate (Figure 10).
A benefit of Giomer Technology is its ion exchange (Figure 11). Fluoride ions offer acid resistance via fluoroapatite, antibacterial effect, and remineralization. Strontium ions offer acid resistance via strontium-apatite, inhibit dental sensitivity, accelerate calcification, and accelerate bone formation. Natrium/sodium ions offer resistance to decay and bacteria and caries prevention. Aluminum ions inhibit dental hypersensitivity. Silicate ions promote calcification of bone tissue. Borate ions offer a bactericidal effect and accelerate bone formation.15-18 Some patients find the science to be very impressive, and explanation of the science often helps convince them to undergo Giomer Technology procedures.
With Giomers, practitioners will see a sustainable fluoride release and recharge (Figure 12). Intraoral areas with high fluoride concentration allow these products to accept and recharge fluoride. In areas of low concentration, these products actually will release fluoride.19-20 Examination after years of service in the mouth shows no delaminations and no debonds.
Case Presentation III: Severe Gingival Recession
Patient "Judy" presented with severe gingival recession on mandibular anterior teeth-multiple Class III and Class IV defects. Treatment options were porcelain veneers; porcelain crowns/porcelain bridge either splinting or with removal of teeth Nos. 24 and 25 and pontics; removal of mandibular incisors with implant placements (variable placements and restorative options); and composite bonding.
Composite bonding was indicated because the teeth had suffered severe gingival recession and full coverage would be difficult, indicating the use of pink composite for both esthetics and biologic response. The patient already was undergoing conventional crown and bridge procedures on the maxillary arch.
A few areas needed to go through odontoplasty, visible in tooth No. 21 (Figure 13). More blending than usual was necessary on such an extreme case; charts are available to assist in blending. Vascularity was indicated with some red colorants. Whitening also was performed, as the patient was undergoing some upper restorative therapy as well. Radiographic analysis in Figure 14 shows that the treatment outcome (Figure 15) was superior.
Conclusion
In many Miller Class III and IV cases in the past, practitioners would have done bonding with large quantities of white material, which would not have looked natural, or would have performed other procedures that compromised dentition. Now, the use of pink and white restorative materials in combination constitutes a conservative approach to treating Class III and IV recession, under the recommended parameters for proper patient selection relating to this type of procedure. Giomer Technology offers great benefits, in terms of esthetics, health, and procedural conservatism, in the treatment of advanced gingival recession and cervical lesions.
About the Author
Dr. Andrew E. Skasko
Private Practice, New Albany, Ohio
References
1. Miller PD. Miller Classification of Marginal Tissue Recession
Revisited After 35 Years. Compend Contin Educ Dent. 2018;39(8):514-520.
2. Smiley W, Skasko A, Stoner J. 2015 Seattle Study Club World Treatment Planning Competition. Phoenix, Arizona. 2015.
3. Kokich V, Spear F. Guidelines for treating the orthodontic-
restorative patient. Sem Orthod Dentofac Ortho. 1997;3:3-20.
4. Kim YI, Kim MJ, Choi JI, Park SB. A multidisciplinary approach for the management of pathologic tooth migration in a patient with moderately advanced periodontal disease. Int J Periodontics Restorative Dent. 2012;32:225-30.
5. Turssi CP, Faraoni JJ, Rodrigues Jr AL, Serra MC. An in situ investigation into the abrasion of eroded dental hard tissues by a whitening dentifrice. Caries Res. 2004;38:473-7.
6. Jaeggi T, Lussi A. Toothbrush abrasion of erosively altered enamel after intraoral exposure to saliva: An in situ study. Caries Res.1999;33:455-61.
7. Addy M, Shellis RP. Interaction between attrition, abrasion and erosion in tooth wear. Monogr Oral Sci.2006;20:17-31.
8. Alexandria AK, Vieira TI, Pithon MM, et al. In vitro enamel erosion and abrasion-inhibiting effect of different fluoride varnishes. Arch Oral Biol.2017;77:39-43.
9. Dionysopoulos D, Tolidis K, Sfeikos T. Effect of air-
abrasion pre-treatment with bioactive glass 45S5 on enamel surface loss after erosion/abrasion challenge. Dent Mater. 2019;35(9):e193-e203. doi:10.1016/j.dental.2019.05.009
10. Hara A.T., Zero D.T., The potential of saliva in protecting against dental erosion. Mongr Oral Sci.2014;25:197-205.
11. D, Kraus T, Schach C, et al. Recontouring teeth and closing diastemas with direct composite buildups: A clinical evaluation of survival and quality parameters. J Dent.2010;38:1001-1009.
12. Lenhard M. Closing diastemas with resin composite restorations. Eur J Esthet Dent.2008;3:258-268.
13. Murchison DF, Roeters J, Vargas MA, Chan DCN. Direct anterior restorations. In: Summitt JB, Robbins JW, Hilton TJ, Schwartz RS, editors. Fundamentals of Operative Dentistry: A Contemporary Approach. 3rd ed. Quintessence; 2006:274-279.
14. Heymann HO. Additional conservative esthetic procedures. In: Roberson TM, Heymann HO, Swift EL Jr, eds. Sturdevant's Art and Science of Operative Dentistry. 5th ed. Mosby; 2006:635.
15. Takahashi Y, Okamoto M, Komichi S, et al. Application of a direct pulp capping cement containing S-PRG filler. Clin Oral Investig. 2019;23(4):1723-1731. doi:10.1007/s00784-018-2596-6
16. Ito S, Iijima M, Hashimoto M, et al. Effects of surface pre-
reacted glass-ionomer fillers on mineral induction by phosphoprotein. J Dent. 2011;39(1):72-79. doi:10.1016/j.jdent.2010.10.011
17. Okamoto M, Ali M, Komichi S, et al. Surface pre-reacted glass filler contributes to tertiary dentin formation through a mechanism different than that of hydraulic calcium-silicate cement. J Clin Med. 2019;8(9):1440. Published 2019 Sep 11. doi:10.3390/jcm8091440
18. Kawashima N, Hashimoto K, Kuramoto M, et al. A novel bioactive endodontic sealer containing surface-reaction-type prereacted glass-ionomer filler induces osteoblast differentiation. Materials (Basel). 2020;13(20):4477. Published 2020 Oct 9. doi:10.3390/ma13204477
19. Kamijo K, Mukai Y, Tominaga T, et al. Fluoride release and recharge characteristics of denture base resins containing surface pre-reacted glass-ionomer filler. Dent Mater J. 2009;28(2):227-233. doi:10.4012/dmj.28.227
20. Shimazu K, Ogata K, Karibe H. Evaluation of the ion-releasing and recharging abilities of a resin-based fissure sealant containing S-PRG filler. Dent Mater J. 2011;30(6):923-927. doi:10.4012/dmj.2011-124