You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The American Dental Association has reported that the two most common procedures performed by general dentists are posterior resin Class II direct restorations and single-unit crowns.1 To determine whether the clinician should treat a tooth with a Class II direct restoration or a single-unit crown, there are many factors to consider. Although a practitioner should consider all facets of direct versus indirect restorations, the most important factors are the size of the lesion and the destruction of tooth structure.2 Other considerations include determining whether the remaining tooth structure must gain strength and protection from the restoration.3 If so, an indirect restoration should be the treatment of choice. Additional indications in choosing a single-tooth crown as the best option are the following4:
• Large failing existing restorations (greater than one-half of the buccolingual intercuspal distance posteriorly)
• Cracks in the existing tooth (symptomatic and asymptomatic)
• Endodontically treated teeth
• Cusp fractures
• Improving existing esthetics
After the clinician decides on a single-unit restoration and properly explains to the patient that it is the best option in lending long-term strength and function back to the tooth, treatment may begin. Fabricating a single crown consists of various procedures, a series of steps that fit into the greater whole. Although these steps may seem basic, they are not as easy to achieve as one might believe. Mastering each step is a challenge unto itself, and achieving a successful outcome is dependent on the clinician's ability to perform each individual step or procedure well.
Although this article will concentrate specifically on the fixed prosthodontic landscape, it should be remembered that restorative treatment is just one component of overall dental care; therefore, in addition to the specific steps mentioned, patients would receive a comprehensive evaluation of their medical status and the health or disease state in their oral cavity. The comprehensive examination would include a treatment plan and clinical evaluation with radiographs, a thorough medical and dental history, and a diagnosis and assessment of the periodontium and tooth vitality.
Initial Visit
Steps involved during the fixed prosthodontic landscape initial visit for a single-crown procedure are the following:
• The patient is prepared. (The series of events that must be accomplished during the first and second appointments are reviewed. Initial discussion with the patient should occur when the treatment plan is presented.)
• A matrix impression is made for provisional fabrication.
• Anesthesia is given.
• Tooth preparation takes place.
• Tissue management is undertaken.
• The final impression is made.
• Fabrication of a provisional restoration occurs.
• Cementation of the provisional restoration is performed.
It is imperative that the correct amount of time is allotted to properly perform each task involved in the first visit. Performing all tasks well in the first visit will most likely allow the second appointment to take less chairtime and increase the success of cementing the definitive crown.
Second Appointment
The second phase or appointment in the fixed prosthodontic landscape is the insertion appointment. The steps involved are as follows:
• The provisional restoration is removed, and the residual temporary cement is cleaned up. (Anesthesia may be necessary to ensure patient comfort.)
• Fitting occurs, with necessary adjustments made to the permanent crown (occlusal, interproximal).
• Final cementation of the definitive crown takes place, including cleanup of residual final cement and verifying proper occlusion.
Recognizing Errors
Errors made within any phase of treatment may contribute to failure of the final restoration. Errors in tooth preparation and final impressions are the most common problems that a clinician and laboratory technician may encounter. Clinicians should be cognizant of the most common errors in tooth preparations5:
• Inadequate tooth reduction on the incisal, occlusal, and axial walls of the tooth
• Over-reduction on tooth surfaces
• Excess taper of the preparation
• Inadequate buildup of missing tooth structure
• Indistinct margins of the preparation
• Excess gingival extensions
• Undercuts in the axial walls of the preparation
• Sharp angles on the preparation
Recognizing the most common errors and avoiding them provides opportunities for the clinician to learn from mistakes, be more critical when evaluating current methods of tooth preparations, and ultimately improve on current techniques to achieve more successful outcomes.
Tooth Preparation
The fundamentals in tooth preparation should include a planned process for transforming the tooth. A tooth preparation should be uniformly reduced in a geometrical form that permits sufficient space for the final restoration. In addition, there should be clean, closely defined finish lines and margins.
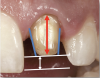
The most important factors to consider in preparing teeth for single-unit restorations are the taper (convergence), height (clinical crown height-how much tooth structure is above the gingiva and the height of the preparation), and reduction (Figure 1).6 Less than or equal to 20 degrees of taper or convergence is clinically appropriate. Overly tapered preparations will prevent the final restoration from being retentive. A preparation that is modestly parallel, while still achieving a good draw, is optimal. A 4-mm crown height is minimally adequate. If the height of the preparation is less than 4 mm, additional retentive features should be considered, such as slots and grooves in the preparation.
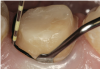
Tooth preparation should be performed as dictated by the type and substrate of the final restoration. Various types of restorations and substrates require different preparation methods. For example, lithium disilicate, porcelain-fused-to-metal (PFM), and porcelain-fused-to-zirconia (PFZ) anterior crown preparations require 1.5 to 2.0 mm incisally, 1.5 mm facially and lingually, and 1.0 mm at the cervical third facially and lingually. Full zirconia crowns in the posterior require 1.0 mm at the cusp tips, 1.5 mm occlusally, 1.0 mm buccally and lingually, and .75 mm at the marginal areas (gingival third of the tooth). Lithium disilicate, PFM, and PFZ posterior crowns require 1.5 to 2.0 mm occlusally, 1.5 mm buccally and lingually, and 1.0 mm at the gingival third or at the margin area (Figure 2).
Depending on the type of restoration and the clinician's choice, a variety of finish lines and margins may be prepared. Margins may be finished in a knife edge, bevel, chamfer, shoulder, or shoulder bevel. The clinician should prepare the finish lines and margins required by the particular substrate of the restoration to ensure strength, fit, and durability.
The ferrule effect, or circumferential banding effect, is primarily the prepared tooth below a core material. This effect is particularly important for endodontically treated anterior teeth. The ferrule should be at least 1.5 to 2.0 mm to increase resistance form (Figure 3).7
Tissue Management
Tissue management is another key step in the fixed prosthodontic landscape. Gingival retraction cords remain the most commonly practiced procedure for tissue management. The goal is to achieve a V-shaped sulcus at a 0.2-mm minimum width, whether a single cord or double cord technique is used. The V-shaped sulcus with a 0.2-mm width creates access for the wash or syringe material so that enough volume may be placed into the desired area and removed in one piece without tearing (Figure 4).
A variety of retraction cords are available in knitted, braided, or twisted configurations. They can be plain cord, also called non-impregnated, or may be impregnated with a hemostatic agent such as aluminum chloride or ferric sulphate. Retraction cords are fairly inexpensive and very effective. The use of a retraction cord may require additional anesthesia to allow comfort to the patient during placement. Retraction cords should always be placed gently because their use has been associated with gingival recession8 (there may be up to 1 mm of gingival recession after using a retraction cord) and may also cause local inflammation and acute tissue injury.9
Using the smallest-diameter cord to achieve desired results is the best option. Placement of the retraction cord should be accomplished using gentle pressure to prevent traumatization of the tissue. The cord could be responsible for postoperative gingival discomfort; however, this condition should resolve within a day or two. A postoperative saltwater rinse or an analgesic such as acetaminophen or ibuprofen may help relieve pain and swelling. The top of the cord should always be visible so that it can be removed before impression making. Wetting the cord with water spray before removal will ensure that the cord will easily slide out without tearing the tissue or causing further bleeding.
A common alternative to retraction cord is the use of retraction pastes and compression caps. In many cases, retraction pastes are used in conjunction with retraction cords. Retraction pastes are useful if the margins of the preparation are equigingival or supragingival-they do not offer much assistance in retracting the tissue but are very effective in hemostasis.
Using a retraction cord and retraction paste together may offer very good results. Compression caps, when used in conjunction with pastes, force the paste somewhat subgingivally and also contribute pressure to stop bleeding (Figure 5). Pastes are recommended to be kept in place for a minimum of 2 minutes and a maximum of 5 minutes. Leaving the paste in place for more than 5 minutes may not prove to be more effective. With the active ingredient in most pastes being an aluminum chloride, allowing the paste to remain longer than 5 minutes could result in irritation of the tissues and promote further bleeding.
Final Impressions
Final impressions are defined as an unequivocal negative likeness or copy in reverse of the surface of an object, an imprint of the teeth and adjacent structures.10 Final impressions may be accomplished using a scanning method or by using conventional impression materials such as a polyvinyl siloxane material. The method of making a final impression depends on both the choice of the clinician and the type of final restoration chosen. If a vinyl impression material is chosen, one that offers more hydrophilicity in the syringe material and a tray material that hydraulically pushes the wash into the sulcus may be best. Capturing adjacent structures is crucial to allow the final restoration to blend with surrounding dentition and tissues. It will also provide a landscape for the laboratory technician to fabricate a final crown with correct form and function.
Provisional Restoration
After the completion of an accurate final impression (and an accurate opposing model), fabricating the provisional restoration is another important step in the process of the fixed prosthodontic landscape. A perfectly functioning provisional restoration is one that stays in place and lends itself to maintaining optimal periodontal health. These factors are especially important when cementing the definitive crown. In addition, the provisional restoration plays an integral part of maintaining space within the dentition; maintaining proper vertical dimension, occlusion, and function; having good esthetics; allowing for proper phonetics; and protecting the dentin and pulp. The provisional should also exhibit optimal marginal integrity to preserve the health of the gingival tissue. Provisional restorations may be used as a blueprint for final restorations, which is helpful when fabricating either multiple units or single units in the anterior region of the oral cavity. To achieve the aforementioned ideals, it is crucial to choose a provisional material that encompasses the following requirements:
• Strength
• Wear resistance
• Esthetics
• Biocompatibility
• Dimensional stability
• Convenient handling
• Ease of contouring and polishing
There are a multitude of choices for the clinician for provisional materials, all of which meet the criteria for fabricating a proper provisional restoration. Methacrylate-based materials include the following:
• Poly-methyl methacrylate
• Poly-ethyl methacrylate
• Vinyl-methyl methacrylate
• Ethyl methacrylate
There are also composite-based provisional materials from which to choose. They include the following:
• Bis-acrylics
• Bis-GMA (bisphenol A-glycidyl methacrylate) resins
• UDMA (urethane dimethacrylate) resins
Any of these materials will allow the clinician to fabricate strong, esthetic provisional restorations. The choice may depend on price point, convenience, and what works best in the clinicians' hands and for the particular task.
Choosing a provisional cement is also dictated by the type of preparation, esthetic considerations, and overall wellness of the tooth and gingival tissues. For example, a clear or translucent provisional cement is ideal for anterior crowns and veneer provisionals because the cement allows greater esthetics. More opaque cements may be used anteriorly if there is a need to block out underlying dark tooth shades. Clinicians may want to use a eugenol-based cement if the tooth is symptomatic postoperatively. The dental professional should, however, be aware of the interaction of eugenol on resin-based or composite-based provisional materials. Some clinicians may choose a cement containing an antimicrobial such as chlorhexidine. The most common types of provisional cements are the following:
• Resin-based
• Zinc-oxide eugenol
• Zinc-oxide non-eugenol
• Zinc polycarboxylate
Final Restoration
Final cementation of the definitive crown also offers a choice to the clinician, on the type of final cement that is appropriate for the particular crown substrate, as well as the area of the oral cavity in which the crown is to be placed. The history of definitive cements dates pre-1870s with the use of oxychloride/oxysulfate cements, followed by zinc phosphate cement (1870), silicate cement (1873), zinc-oxide eugenol cement (1875), zinc-polycarboxylate cement (1963), glass-ionomer cement (GIC, 1972), adhesive resin cement (1986), resin-modified glass-ionomer cement (RMGI or RRGI, 1992), and self-adhesive resin cement (SARC, 2004).11,12 Today, the final cement categories most commonly used are GIC, RMGI or RRGI, SARC, and traditional resin cement.
Depending on the type of substrate for the final restoration, there are recommendations pertaining to the type of final cement that should be used. In addition, it is necessary that the clinician and dental laboratory follow particular clinical requirements for preparing the substrate or final crown before final cementation. Manufacturers have recommended methods of preparing the final restoration before cementation. The dentist and laboratory technician should be particularly aware of the recommendations to optimize the longevity of the definitive crown.
The most common types of ceramics used for final restorations are feldspathic porcelains, leucite-reinforced ceramics, and lithium-disilicate, alumina, and zirconia-based ceramics. Matching the most compatible final cement to the type of ceramic can be the difference between success and failure. Careful attention should be placed when matching a ceramic crown to final cement (Figure 6).
Preparing the definitive crown for final cementation, as mentioned previously, may require the dentist or laboratory technician to treat the crown before try-in and final placement. The clinician and technician should be aware of the effects of some of the treatments recommended for the intaglio of the ceramic crown.
Hydrofluoric acid is recommended by certain ceramic manufacturers for pre-treatment of the crown. Hydrofluoric acid is capable of dissolving bonds in silicate substrates. It creates micro-retentive etching patterns on the internal surfaces of glass-containing ceramics. This acid will not weaken the strength of silicate-ceramic materials. However, the use of hydrofluoric acid in the oral cavity is not recommended. It is an extremely caustic substance, and extreme care should be used when handling it. It is not recommended on tooth structures under any circumstances.13
Silane coupling agents are also commonly required for pre-treating the intaglio of the ceramic restoration before cementation. Silane coupling agents are compounds with functional groups that bond both organic (resins) and inorganic materials (glass, silica). The silane agent acts as an intermediary between the ceramic crown and cement, improving the adhesion of both substrates. In addition, silanes promote wetting of the surface to allow better penetration of the resin cement.
Metal priming agents are also among the types of pre-treatments for the intaglio of the definitive crown before cementation. Metal primers are similar to silane coupling agents in that they contain bifunctional phosphate monomers that bond to the metal or oxide ceramic, such as zirconia or alumina on one side, and bond to resin cement on the other side.13
All individual procedures mentioned in this article are vital in delivering a final restoration that will restore proper form and function for the patient. Mastering the basic steps is easier said than accomplished. The clinician must focus on the details for each procedure and perform them all to the very best of one's ability.
About the Author
Jason H. Goodchild, DMD
Private Practice, Havertown, Pennsylvania
Summary
In summary, one should keep in mind the key points that ultimately will lead to success. Preparations should be created that coincide with the type of substrate chosen. Preparations should be easy to impress, and the final impression should be easily interpreted by the laboratory technician. The clinician should critique and evaluate impressions before sending them to the laboratory. Errors should be identified before sending, and if necessary, final impressions should be retaken. The required cement for the type of substrate chosen should be used to ensure the best outcome. Finally, one should communicate often and effectively with the dental laboratory; laboratories are clinicians' partners and are an integral part of the team working with the clinician to provide optimal care to patients.
References
1. ADA Survey Center. 2005-06 Survey of Dental Services Rendered. Chicago, IL: American Dental Association; 2007.
2. Schillingburg HT Jr. Treatment planning for single-tooth restorations. In: Fundamentals of Fixed Prosthodontics. 4th ed. Quintessence Publishing; 2012:71-79.
3. Smithson J, Newsome P, Reaney D, Owen S. Direct or indirect restorations? Int Dent. 2001;1(1):70-80.
4. Christensen GJ. When is a full-crown restoration indicated? J Am Dent Assoc. 2007;138(1):101-103.
5. Christensen GJ. Frequently encountered errors in tooth preparations for crowns. J Am Dent Assoc. 2007;138(10):1373-1375.
6. Goodacre CJ. Designing tooth preparations for optimal success. Dent Clin North Am. 2004;48(2):359-385.
7. Tan PL, Aquilino SA, Gratton DG, et al. In vitro fracture resistance of endodontically treated central incisors with varying ferrule heights and configurations. J Prosthet Dent. 2005;93(4):331-336.
8. Ruel J, Schuessler P, Malament K, Mori D. Effect of retraction procedures on the periodontium in humans. J Prosthet Dent. 1980;44(5):508-515.
9. Feng J, Aboyoussef H, Weiner S, et al. The effect of gingival retraction procedures on periodontal indices and crevicular fluid cytokine levels: a pilot study. J Prosthodont. 2006;15(2):108-112.
10. The glossary of prosthodontic terms. 9th ed. J Prosthet Dent. 2017;117(5s):e1-e105.
11. Albers HF. Tooth-Colored Restoratives: Principles and Techniques. 9th ed. BC Decker; 2001:43-45.
12. Pameijer CH. A review of luting agents. Int J Dent. 2012; 2012:752861. doi: 10.1155/2012/752861.
13. Kimmich M, Stappert CF. Intraoral treatment of veneering porcelain chipping of fixed dental restorations: a review and clinical application. J Am Dent Assoc. 2013;144(1):31-44.