You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Dental impressions form the foundation for successful restorations, and yet with a wide variety of considerations, materials, and techniques, obtaining impressions may create confusion and inconsistencies in the dental practice. This article aims to inform dental assistants about how to master the art of impressions by understanding material characteristics, indication requirements, and techniques that will allow the clinical team to deliver quality dentistry that will last.
Although digital scanners are advancing alternatives for how impressions are made, many dental practitioners are still using conventional dental impression materials. There is still a need for physical impressions in specific cases, even though a survey has revealed that 76% of dental students prefer intraoral scanning-the same survey showed that only 48% of practicing dentists prefer digital to conventional impressions.1
Accurate physical impressions represent detailed records of the oral cavity. They capture the exact dimensions of the preparation and the soft tissue, the margins of the preparation, and the prepared teeth themselves and surrounding dentition relationship.2 The finite details ensure that restorations can be placed quickly and comfortably. However, gag reflexes and patient discomfort limit impression success by potentially compromising accuracy.3 Determining which types of materials and techniques to use can make capturing exact details less difficult.
The Evolution of Impression Materials
The introduction of impressions as a dental technique began in the 1700s, when Philipp Pfaff demonstrated the method using softened wax.4 Over the following centuries, dental professionals have used a variety of materials. Wax appeared usable but exhibited too much distortion on removal. Plaster and zinc oxide-eugenol showed an inability to flex over and around undercut without breakage and were quickly abandoned.5
The introduction of hydrocolloid materials, agar, and alginate (Figure 1 and Figure 2) provided greater accuracy but lower tear-resistance and decreased dimensional stability over time.5,6 Created to improve tear-resistance, polysulfide rubber-based impression materials provided greater accuracy but only minor improvements in dimensional stability. The materials also proved challenging to mix and produced a bad odor.5 The 1960s brought polyethers, and in the 1970s, condensation and addition-reaction silicones were introduced. These materials eliminated both poor stability and low tear-resistance problems.4 Although the materials provided an improvement over previous options, they still had limitations, and no material is ideal for every impression situation.5
Dental professionals use impressions to obtain exact replicas of hard and soft tissues. With superior properties, improved materials ensure the creation of more accurate and predictable impressions.7 By providing the foundation for future dental procedures, impressions represent a blueprint to successful indirect restorations.8,9
Characteristics of Impression Materials
Hydrophilicity
Hydrophilicity, the impression's affinity for water, affects the way the material reacts in the oral cavity. This characteristic influences the material's ability to accurately record intraoral surface detail.4 Hydrophilic materials demonstrate a high affinity for moisture and allow a high degree of surface detail because of their strong surface-wetting capabilities. Hydrophobic materials, contrarily, demonstrate low affinity for moisture and offer a low degree of surface detail, with poor surface-wetting properties.4,10-12Hydroactive material provides a combination of both hydrophobic and hydrophilic characteristics. Because it is naturally hydrophobic, hydroactive material becomes hydrophilic through the addition of surfactants.2 This hybrid material offers a superior degree of surface-wetting ability and detail.4
Elasticity and Tear Strength
Elasticity and tear strength describe the way an impression material changes as it is removed from the mouth. Ideally, the elasticity of the material would allow it to stretch and then return to its original shape. An impression can become distorted when it is stretched beyond its elastic capacity and does not return to its original shape. Similarly, tear strength of an impression material demonstrates its ability to return to its original shape without tears.7 Several factors influence the tear strength of impression material, including gingival retraction, depth of the subgingival margin, amount of bleeding, any sharp edges on the preparations, and any tooth preparations that increase the resistance needed to remove the impression materials.13 Both elasticity and tear strength require proper understanding to prevent the need for multiple impression retakes. Additionally, choosing a material that can be disinfected is important, as are the protocols for disinfection that may be impression-material specific.
Viscosity
Viscosity describes the flow of unset impression material. The four classifications of viscosity include low (eg, syringe or wash material), medium (eg, one-step monophasic material or heavy body), high (eg, tray material), and very high (eg, putty).7 The viscosity of impression materials varies based on the amount of filler present in the material.14 Viscosity affects the ability of the material to capture intraoral details. Generally, lower-viscosity materials record finer details and allow for the most significant shrinkage while the impression material sets.14However, low-viscosity materials prove harder to work with compared with high-viscosity impression materials. Depending on the type of planned restoration and the detail necessary from and in the impression, different levels of viscosity may be appropriate.
Working and Setting Time
Working and setting time describe the amount of time it takes to mix and place the material in the impression tray and the time required by the impression to set in the oral environment, respectively.7 Working time is influenced by the number of preparations, the use of hand-mix or automix materials, and the viscosity of the material.2 Manufacturers have a variation in setting times from regular to fast to allow the clinician to select which amount is appropriate for the case being treated. Temperature affects both working and setting time.2,15 Ideal working time and setting time depend on the number of preparations, the manufacturer's directions, and the skill of the assistant.
Dimensional Stability
Dimensional stability ensures that the laboratory receives accurate and stable impressions. Ideally, a completed impression remains unaltered for prolonged periods, resists temperature changes during shipping, and retains capability for fabricating multiple accurate casts.10 Affected by temperature, water absorption, and reduction in spatial volume because of contraction from polymerization, dimensional stability remains an essential characteristic for the usability of an impression.
Material Selection
Preliminary Impressions
Preliminary impressions, used for treatment planning, do not require as many details as the final versions; therefore, material options are less costly, including hydrocolloids, such as alginate, and polysulfide.7 These materials should be avoided, however, when taking final impressions.
What makes these materials less than adequate for final impressions? Water-based hydrocolloids are made of up to 80% water.14 They are very delicate materials with low tear strength and that do not provide finite detail.16Rubber-based polysulfide materials lack dimensional stability; although they provide enough detail for treatment planning, they should not be used for final impressions.
It is crucial to remember that although preliminary impressions may not require as much detail, it is still necessary to obtain accurate impressions for diagnostic models used for treatment planning. The accuracy stipulations are not nearly as stringent as they are for crowns, implants, bridges, and any other restoration that dentists place. However, preliminary models are used to study occlusion, arch form, occlusal plane, and esthetics, which are all important records used in treatment planning.
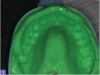
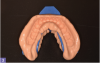
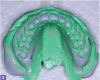
Polyvinyl siloxane impression materials are excellent for creating an optimum diagnostic impression. They allow multiple pours if necessary and eliminate the need to pour the model immediately. When using this material, assistants should dry the teeth before placing the impression and be careful to capture all the surfaces of the teeth, extending well beyond the free gingival margins (Figure 3 and Figure 4).
Final Impressions
Polyethers provide an accurate and useful option for final impressions. They allow multiple pours, long-term dimensional stability, and short setting time.2 With a shelf life of up to 7 days, high accurate surface detail, minimal distortion on removal, and adequate tear strength, polyethers offer an impression that will last. However, polyethers' disadvantages include rigidity, unpleasant taste and odor, tendency to absorb water from the atmosphere and swell over time, and difficult intraoral removal.2,5 Nevertheless, polyethers have a successful clinical history and still represent an established option in impressions.
Another final impression material, vinyl polysiloxane (VPS), improves several of polyether's disadvantages. VPS materials provide less rigid impressions, neutral odor and smell, and impressions that do not absorb excess fluid.2 Other VPS advantages include multiple accurate casts, extremely high accuracy, superior tear strength, excellent elasticity, improved dimensional stability, and shelf life of up to 7 days.2 An inherently hydrophobic material, VPS improves this characteristic with added surfactants to increase the hydrophilicity.7 However, a disadvantage is reduced polymerization when latex contamination occurs.2As the most popular category of impression material, VPS ensures an accurate final impression.2
A combination of polyethers and VPS, vinyl-polyether hybrids offer the advantages of both materials. Hybrids demonstrate high tear strength, multiple pours, and high dimensional stability.7 The polyether contributes to the material's genuinely hydrophilic nature without added surfactants,7 and the silicone element increases dimensional stability and elasticity. Also, like some VPS materials, the hybrid material offers a pleasant flavor, eliminating the bitter taste and smells of polyethers.7 Vinyl-polyether hybrids present an ideal combination of characteristics for accurate impressions (Figure 5).
Impression Techniques
Figure 6 and Figure 7 present a step-by-step guide for creating an impression with an example putty material. Retraction techniques are described below.
Methods of Retraction
It is important to recognize that retraction and hemostasis are two different objectives. Although it may be possible to accomplish both tasks with a single treatment modality, this is not always the case. Retraction is the temporary displacement of the gingival tissue away from the surface of the tooth to expose a subgingival margin and to make room for the impression material to record it. Retraction can also be used before preparing the tooth. In that case, retraction serves as a visual aid in establishing an ideal subgingival location to place a preparation margin. This may help prevent iatrogenic injury to the gingival crevicular tissues and facilitates the preservation of periodontal health and the biologic width. Four types of retraction techniques are in general use today, depending on case requirements. The retraction method chosen may be influenced by the clinician's familiarity with the technique, the location, quality, and condition of the soft tissue, the clinician's skill level, and the complexity of the case.
Cord Techniques
The cord-packing technique is the most popular method of retraction and is done using a twisted, knitted, woven, or braided cord. A variety of natural and synthetic fiber types are used in making gingival retraction cords, including wool yarn, cotton, and silk. The cords are commercially available in plain versions and impregnated or pretreated with hemostatic medicaments. When using a cord-packing technique, an appropriately sized cord is gently placed into the gingival sulcus with the intent of mechanically displacing the soft tissues from the tooth and margin of the preparation. In general, it is best to use the smallest cord possible because larger cords can sometimes tear delicate gingival tissue, increase hemorrhage, and damage the sulcular epithelium. Fortunately, newer impression materials can capture excellent marginal detail within relatively small gingival spaces. Typically, retraction cords are placed after the tooth preparation is completed and then removed immediately before the impression tray is seated. Cords are packed with many different types of hand instruments.
Single-cord technique. The single-cord technique helps to deflect and manage the soft tissues. It works best with tooth preparations that terminate supragingival or at the tissue height.17Although occasionally uncomfortable for patients, the cord displaces the tissues, exposing the marginal area of the preparation, and remains in place until it is time for the final impression.17 The end of the cord packer must be thin enough to be placed in the gingival sulcus without damaging the tissue and causing any bleeding (Figure 8). The angulation of the instrument will help in the orientation for the placement.
Double-cord technique. The double-cord technique uses the single-cord technique but adds another retraction cord. With the single cord in place, the second cord lies on top of the first, further displacing the tissue.17 This creates sufficient room for the impression material to fill the sulcular area and flow around the preparation.18 The double-cord technique creates a space to record intricate details of the marginal area.19 With the first cord still in place from the preparation to the final impression, patients may complain of discomfort from this technique.
Gingival Retraction Paste Technique
The gingival retraction paste technique aims to alleviate some of the pain and uncomfortable nature of the retraction cord techniques. When placed in the gingival sulcus, the paste displaces the soft tissue, allowing greater exposure of the preparation margin (Figure 9).17 Its chemical composition also provides a localized homeostasis effect, and it can be used as the basis of the double-cord technique, eliminating the need for the single retraction cord.17
Soft-Tissue Laser
Soft tissue lasers create surgical retraction in much the same way as electrosurgery. Lasers are generally considered safer than electrosurgery because they use a high-intensity form of light instead of electrical current to remove the tissue. The laser light typically is delivered into the surgical area by a thin glass fiber or fiber-optic bundle (Figure 10). Lasers tend to produce a shallower cellular necrotic burn in the tissues adjacent to the epithelial layer, so healing is faster and more predictable than with electrosurgery. Although lasers can also cause burn damage to the dentinal, cemental, and attachment tissues, the risks are lower. Lasers are also safe for patients with pacemakers or when gaseous anesthetics are in use. Depending on the type and wavelength of the laser, they may be either useful or totally ineffective in assisting with hemostasis. Lasers are most often recommended in cases where margins are especially deep or when there is excessive bleeding.
Conclusion
An ideal impression accurately records intraoral details, maintains its dimensional stability, and is poured for multiple casts. In the last 250 years, the evolution of impression materials has enabled dental professionals to obtain highly accurate, easy to use, and stable dental impressions. Improved techniques offer a variety of sufficient means to achieve great impressions without sacrificing patient comfort. Successful impressions rely on careful evaluation of each patient and planned restoration to identify the ideal material and technique for an effective and accurate impression.
About the Author
Shannon Pace Brinker, CDA, CDD
Private Practice
Virginia Beach, Virginia
References
1. Joda T, Lenherr P, Dedem P, et al. Time efficiency, difficulty, and operator's preference comparing digital and conventional implant impressions: a randomized controlled trial. Clin Oral Implants Res. 2017;28(10):1318-1323.
2. Terry DA, Leinfelder KF, Lee EA, James A. The impression: a blueprint to restorative success. Inside Dentistry. 2006;2(5):66-71.
3. Dickinson CM, Fiske J. A review of gagging problems in dentistry: 2. Clinical assessment and management. SADJ. 2006;61(6):258-262, 266.
4. Pitel ML. Successful Impression Taking. First Time. Every Time. Armonk, NY: Heraeus Kulzer, 2005: C-C14.
5. Berry T, Radz G. New technologies for easier and more accurate impressions. Inside Dentistry. 2007;3(9):46-48.
6. Wassell RW, Barker D, Walls AWG. Crowns and other extra-coronal restorations: impression materials and technique. Brit Dent J. 2002;192(12):679-690.
7. Burgess JO. Impression material basics. Inside Dentistry. 2005;1(1):30-33.
8. Vakay RT, Kois JC. Universal paradigms for predictable final impressions. Compend Contin Educ Dent. 2005;
26(3):199-209.
9. Kois JC, Vakay RT. Relationship of the periodontium to impression procedures. Compend Contin Educ Dent. 2000;
21(8):684-690.
10. Lee EA. Impression material selection in contemporary fixed prosthodontics: technique, rationale, and indications. Compend Contin Educ Dent. 2005;26(11):780-789.
11. Johnson GH, Lepe X, Aw TC. The effect of surface moisture on detail reproduction of elastomeric impressions. J Prosthet Dent. 2003;90(4):354-364.
12. Petrie CS, Walker MP, O'mahony AM, Spencer P. Dimensional accuracy and surface detail reproduction of two hydrophilic vinyl polysiloxane impression materials tested under dry, moist, and wet conditions. J Prosthet Dent. 2003;90(4):365-372.
13. Laufer BZ, Baharav H, Cardash HS. The linear accuracy of impressions and stone dies as affected by the thickness of the impression margin. Int J Prosthodont. 1994;7(3):247-252.
14. Donovan TE, Chee WW. A review of contemporary impression materials and techniques. Dent Clin N Am. 2004; 48(2):445-470.
15. Mandikos MN. Polyvinyl siloxane impression materials: an update on clinical use. Aust Dent J. 1998;43(6):428-434.
16. Kurtzman, G. Creating great dental impressions. Inside Dental Assisting. 2012;8(1):42-45.
17. Radz GM. Soft-tissue management. The key to the perfect impression. Compend Contin Educ Dent. 2010;31(6):463-465.
18. Paquette JM, Sheets CG. An impression technique for repeated success. Inside Dentistry. 2012;8(2):70-80.
19. Perakis N, Belser UC, Magne P. Final impressions: a review of material properties and description of a current technique. Int J Periodontics Restorative Dent. 2004;24(2):109-117.