You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The progress made by those in the medical field can now be transferred to dentistry using the dental videoscope. Advances in visual technology now allow clinicians to significantly improve clinical results by using minimally invasive procedures to treat periodontal and peri-implant problems. This follows a trend well established in medicine. As seen in medicine, improved visualization and smaller incisions result in improved surgical outcomes, less patient pain and morbidity, and more rapid healing.1 Advances in visual technology now available for dentistry are based on those used by the medical profession.2
Before the introduction of the videoscope, the surgical microscope was an early improvement. Unfortunately, this device is cumbersome and difficult to use in the posterior portion of the mouth and on the lingual aspects of teeth or implants (Figure 1).3,4 The next improvement was the fiber optic endoscope that was introduced to dentistry 20 years ago for use in performing nonsurgical periodontal procedures, such as periodontal root planing.5However, the dental endoscope is of limited use due to its extremely steep clinical learning curve, limited visual acuity, and the need for a constant flow of water to clean the lens (Figure 2). The latest improvement is the introduction of the dental videoscope. The dental videoscope uses a very small high-definition camera, which provides visualization technology that is clinically practical and easy to use, while avoiding the problems of older visualization approaches (Figure 3).
Extensive research has been published on the dental videoscope over the past decade. The research and development of the videoscope was performed with the assistance of multiple National Institutes of Health grants from the National Institute of Dental and Craniofacial Research. The videoscope is specifically designed for use in minimally invasive dentistry6 and is now commercially available for clinicians.
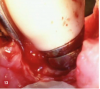
The videoscope differs from the endoscope. The endoscope uses an optical fiber, which produces inherent image distortion, whereas the videoscope eliminates the optical fiber and instead places a very small high-definition camera into the treatment site. Placing a camera into the minimally invasive treatment site generates an electronic signal that produces a clear, undistorted, true-color image displayed in real time on a surgical monitor (Figure 4). Another major improvement is that it eliminates the need for the constant flow of water required by the endoscope to keep the lens clear. Instead, the videoscope uses a low-pressure airflow that effectively and safely keeps the lens clear (Figure 5).7 By eliminating the optical fiber and water flow for clearing the lens, the videoscope overcomes the problems that have limited the application of minimally invasive visualization in dentistry, allowing dentistry to join medicine in establishing small incision procedures as a standard surgical approach.
The dental videoscope was initially designed for periodontal procedures and paved the way for the introduction of videoscope-assisted minimally invasive surgery (VMIS).8 Extensive publications have described the VMIS procedure as producing predictable and successful regeneration of periodontal bone and attachment around natural teeth.8-11 VMIS has been further refined for the treatment of attachment loss and regeneration around implants with peri-implant bone loss (peri-implantitis).12The information that follows gives detailed descriptions and instructions for performing VMIS regeneration procedures on both natural teeth and implants. Other uses for the dental videoscope, such as sinus elevation, surgical and nonsurgical endodontics, and repair of damaged implants, are also discussed.
VMIS for Natural Teeth and Implants
The long-term goals of VMIS are predictable regeneration of periodontal supporting tissues and minimization or elimination of negative esthetic consequences. Additionally, by using very small incisions and minimal reflection of the gingival tissue, VMIS is also designed to cause minimal to no postsurgical discomfort for the patient. The published long-term clinical results of using VMIS for regeneration on natural teeth report the fulfillment of these goals with shallow pockets, improved clinical attachment levels, apparent regeneration of clinical attachment to the tooth surface, no change in soft-tissue contours, and minimal to no pain for the patient.8-11Research is ongoing regarding the clinical results on implants. The information published to date reports positive clinical outcomes and radiographic evidence indicating bone regrowth in close approximation to the damaged implant, suggesting possible re-osseointegration.12
Indications for VMIS on Natural Teeth
Because VMIS is designed to regenerate periodontal supporting tissues such as bone and soft-tissue attachment, the ideal indication for VMIS on natural teeth is an isolated residual periodontal defect, often interproximal, that has not fully responded to nonsurgical treatment (scaling and root planing). Traditional periodontal bone regeneration, such as guided tissue regeneration, only yields predictable and favorable outcomes if the defect has intact walls of native bone (three-walled defect). Studies on the results of VMIS have shown that the same favorable results occur when there is only a minimal amount of the patient's native bone remaining. A large university study showed equal results with one-, two-, or three-walled bony defects.8-10 This means that VMIS is indicated and can be used successfully in many more defects than would be expected to respond to traditional regenerative procedures.
Indications for VMIS on Implants
The indications for VMIS on implants are in areas of peri-implantitis where bone loss has occurred. As with natural teeth, these are usually isolated bony defects.
Incisions for VMIS on Natural Teeth
The initial VMIS incisions are usually made using either a 15c or 12d blade. A micro-blade can also be used but is not necessary. For almost all interproximal defects on natural teeth, VMIS incisions should be made on the lingual. This means that no incision or flap elevation is made on the buccal. By placing the incisions on the lingual, the esthetically sensitive buccal papilla remains undisturbed. Three separate, very small incisions are made on the lingual (Figure 6). The first two incisions are made in the sulcus of the teeth adjacent to the interproximal lesion (incisions A and B in Figure 6). No tissue, such as a collar of tissue, should be removed with these two incisions. The aim of these incisions is to sever the granulation tissue in the sulcus from the bone and connective tissue. The incisions are extended only to the level of the remaining bone. Unlike traditional incisions for resective periodontal surgery (osseous surgery), these incisions are not designed to remove the sulcular lining. The third incision (incision C in Figure 6) is placed in the base of the papilla, at least 3 to 4 mm away from the tip of the papilla. The goal of the VMIS incision pattern is to leave the col tissue and tip of the lingual papilla intact.
After the three initial incisions are made, the base of the papilla is reflected using a split-thickness incision. This can be performed with a sharp Orban periodontal knife or one of several tunneling knives. The incision consists of splitting the apical portion of the papillary tissue (split-thickness incision) to the crest of the remaining bone that is the edge of the osseous defect (Figure 7). The aim of using a split-thickness incision is to maintain an intact periosteum. Maintaining the periosteum will preserve a large portion of the blood supply to the gingiva. Maintaining gingival blood supply will speed healing, will minimize postsurgical pain, will help prevent postsurgical recession, and may contribute to bone regeneration. The use of a periosteal elevator should be avoided. A periosteal elevator acts to pull the periosteum off the bone, and its use is associated with increased postsurgical pain and soft-tissue recession.
Incision for VMIS on Implants
The incisions for VMIS around implants are similar to natural teeth but must be modified to accommodate the shape of the implant. A sulcular incision is made around the implant in the area of bone loss. The incision is extended to the mesial and distal as a split-thickness incision. This incision will extend to the line angle of adjacent teeth if present, or several millimeters into adjacent edentulous areas (Figure 8). A major difference in the use of VMIS on an implant is the removal of a section of connective tissue approximately 1-mm thick that is directly adjacent to the area of bone loss. Surgically, this is similar to the harvesting of a thin connective tissue graft (Figure 9). This step is performed to remove any microscopic particles of cement or titanium, which have been shown to penetrate the tissue and cause inflammation in cases of peri-implantitis.13
Debridement of the Defect on Natural Teeth and Implants
As with all periodontal surgical procedures, granulation tissue must be removed from the defect. The videoscope allows for visualization of this step using minimally invasive access. Granulation tissue removal is performed using small periodontal curettes, which can be used with the small surgical access opening, without placing undue pressure on the margins of the soft tissue. Many large surgical curettes used in routine periodontal access surgery, such as a Prichard curette, are not suitable for VMIS due to the inability to insert them into the bony defects through the small VMIS access incisions. Either a Younger-Goode 7/8 used in a manner similar to a spoon for caries (Figure 10) or a small Gracey curette is generally chosen because their small size allows them to access the periodontal defect using the small VMIS surgical access incisions.
Debridement of Root Surfaces on Natural Teeth in VMIS
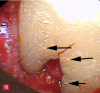
On natural teeth, debridement of the exposed root surface and the complete removal of calculus is considered pivotal to the results reported for VMIS. Calculus removal usually starts with the judicious use of an ultrasonic scaler. The coolant spray from the scaler may briefly obscure vision with the videoscope, but the airflow over the lens will clear the water in seconds. Further calculus removal is performed with the use of small curettes. The judicious use of a bone file on the calculus surface is excellent for removing calculus through the small incisions (Figure 11). Following routine mechanical debridement of the root surface, the high magnification of the videoscope reveals what has been clinically termed "microislands of calculus" (Figure 12).9 The material shown in Figure 12 is verified to be small areas of calculus, as opposed to a post-scaling smear layer, based on laser fluorescence.14These microislands of calculus are removed by burnishing the root surface with 24% neutral pH ethylenediaminetetraacetic acid (EDTA) on a cotton pellet until the microislands are no longer visible using the videoscope. This step usually takes less than a minute of burnishing but may require longer. It is postulated that the removal of these microislands of calculus may be a critical factor in the high predictability of regeneration success reported with VMIS.2
Debridement/Disinfection of the Implant Surface in VMIS
For implants, instrument contact with the roughened implant surface is avoided. Although soft-tissue debris and biofilm are usually present on the roughened surfaces of implants with peri-implantitis, no studies have positively identified calculus formation on implant surfaces. Further, the roughened surfaces of implants have a thin layer of titanium oxide, which can be easily damaged. Because of this, the VMIS technique avoids instrumentation of the implant surface and does not use any harsh or acidic chemicals for disinfection, such as hydrogen peroxide. Disinfection is accomplished by gently cleaning the implant surface with sterile gauze soaked with a saline solution (Figure 13).12
Regeneration Material Used With VMIS on Natural Teeth and Implants
Many types of regeneration material have been used with VMIS. The published university-based studies of VMIS on natural teeth have used the protocol and materials described here.8-12Demineralized freeze-dried bone allograft (DFDBA) mixed with enamel matrix derivative (EMD) is placed in the defect after debridement. According to the manufacturer's instructions, the cleaned root surface is dried and EMD is placed on the root or implant. The DFDBA is first moistened with a saline solution for several minutes before adding the EMD. The DFDBA is placed in a container and then blotted with sterile gauze to remove excess saline. At that point a small amount of EMD is added to the moistened DFDBA. The DFDBA/EMD mixture is then placed into the debrided defect (Figure 14). Care should be taken to not place too much bone in the defect. Overfilling the defect with bone can make it difficult to obtain primary soft-tissue closure of the lesion.
Closure of the VMIS Surgical Access on Natural Teeth and Implants
For an interproximal lesion on natural teeth, a single vertical mattress suture is placed at the base of the papilla using 4-0 or 5-0 suture material of the surgeon's choice. For implants, a similar vertical mattress suture is placed on the mesial and distal of the implant. Chromic or plain gut suture was used in the published university-based studies.8-11 Suture placement is shown in Figure 15. The purpose of the suture is to stabilize the base of the papilla and is not designed to close the mesial-distal incision. Care should be taken to not place the suture at the thin tip of the papilla or reflected tissue. Placing the suture in the thin portion of the papilla is associated with increased soft-tissue recession. The soft-tissue edges of the incision are approximated using finger pressure on a saline-soaked gauze. A closed VMIS incision is shown in Figure 15. Complex suturing, as is used in the papilla preservation suturing technique, is not necessary and may be detrimental to soft-tissue retention.
Postsurgical Discomfort and Patient Perception of VMIS
Almost all patients report no pain following VMIS.9 In a large study of 110 surgical sites in 30 patients, only a single patient reported slight pain after VMIS.8-11 This includes a pain scale that was obtained on the evening of the surgical procedure. In this same study, a patient satisfaction questionnaire was obtained after surgery at 6 months, 12 months, and 36 months. All patients expressed satisfaction with the surgery regarding discomfort, function, and esthetics. All patients stated they would have the surgery performed again if it was necessary at another site and would recommend the surgical procedure to a friend.
Long-term Regenerative Results of VMIS
The 3- to 5-year findings from a large university-based study of VMIS on natural teeth showed excellent and predictable results.10At 36 months postoperative, the mean pocket probing depth of surgical sites was 2.73 mm and the mean clinical attachment was 2.94 mm. Of the 110 sites in 30 patients, all surgical sites had pocket postsurgical probing depths of less than 4 mm. Unlike other periodontal regenerative surgery reports that show some postsurgical recession,15 VMIS showed no mean postsurgical recession and actually showed an improvement in soft-tissue height of 0.49 mm. An improvement in recession after periodontal regenerative surgery has not been reported with any other periodontal regenerative surgical techniques. Clinical results at 6 months, 12 months, and 36 months are shown in Table 1.
There are ongoing studies regarding the use of VMIS with implants. One study reported on an implant with a preoperative 10-mm pocket probing depth with pain and bleeding on probing.12At 1 year it was reduced to a 2-mm pocket probing depth with no pain or bleeding on probing. A radiograph showed apparent bone fill of the defect in close approximation to the implant, suggesting re-osseointegration.
Practice Implications
The use of VMIS on natural teeth and implants adds a new dimension to the clinical delivery of periodontal therapy. The use of the videoscope allows the clinician to offer a true minimally invasive periodontal regeneration procedure that has strong published scientific outcomes data. This is not true for some other procedures that are represented as "minimally invasive." Additionally, VMIS can deliver regenerative results with minimal to no discomfort using a procedure that is focused on only those areas that have not responded to traditional nonsurgical procedures, thus sparing the patient the inclusion of multiple healthy teeth in the surgical site, as is the case in using traditional "quadrant" surgery. Frequently, patients are fearful of painful periodontal surgery and the esthetic results of long teeth and black triangles. VMIS offers a focused, therapeutic approach with minimal discomfort that results in little to no negative esthetic changes and can frequently produce improved, esthetically pleasing soft-tissue contours. These factors are attractive to patients in need of periodontal therapy who wish to save their teeth. In the authors' experience, patient acceptance of VMIS is excellent when they are presented with the benefits of VMIS.
Use of the Videoscope for Other Dental Procedures
The dental videoscope was initially designed for use in regenerative periodontal procedures, and most published studies have reported on this aspect of its use. However, the videoscope is increasingly being used in other dental procedures. The videoscope is frequently used for improved visualization during surgical (Figure 16) and nonsurgical (Figure 17) endodontic procedures.16 For both applications, the videoscope is used in place of the surgical microscope. Unlike the surgical microscope, the videoscope can be easily maneuvered to a favorable angle to obtain different views of an endodontic treatment area and can be held by an assistant so that both the operator's hands are free. Another use of the videoscope is for sinus elevation surgery (Figure 18). The videoscope allows close-up visualization of the sinus membrane during elevation and close observation of the membrane during repair of any perforation of the membrane before bone grafting. The videoscope can also be used in prosthetic complications. Figure 19 shows a broken screw in an implant before removal. The videoscope allows detailed observations during removal of the screw fragment.
Summary
Minimally invasive periodontal surgery represents a proven approach for treating periodontal disease that yields favorable results compared with traditional periodontal therapy.17 The dental videoscope and VMIS represent a new and improved approach for visualization of minimally invasive dental procedures. Extensive research has shown that using the videoscope to perform VMIS regenerative periodontal procedures for defects on natural teeth yields excellent, predictable, and long-term stable results. Additionally, VMIS on natural teeth does not result in postsurgical soft-tissue recession. The application of VMIS to treating peri-implant bone loss has shown excellent early results. The videoscope is also used successfully in multiple other dental procedures. The videoscope is a new visualization technology that can move dentistry toward the advantages of minimally invasive techniques, which are currently routine in many areas of medicine.
About the Author
Stephen K. Harrel, DDS
Professor
Department of Periodontics
Texas A&M University College of Dentistry
Dallas, Texas
Jonathan Blansett, DDS, MS
Private Practice
Rogers, Arkansas
References
1. Hunter JG, Sackier JM. Minimally invasive high tech surgery: into the 21st century. In: Hunter JG, Sackier JM, eds. Minimally Invasive Surgery.New York, NY: McGraw-Hill; 1993:3-6.
2. Harrel SK. Videoscope-assisted minimally invasive surgery (VMIS) for bone regeneration around teeth and implants: a literature review and technique update. Dent J (Basel).2018;6(3):30.
3. Tibbetts LS, Shanelec DA. An overview of periodontal microsurgery. Current Opin Periodontol.1994;1:187-193.
4. Tibbetts LS, Shanelec D. Periodontal microsurgery. Dent Clin North Am.1998;42(2):339-359.
5. Stambaugh RV, Myers G, Ebling W, et al. Endoscopic visualization of the submarginal gingival sulcus and tooth root surfaces. J Periodontol.2002;73(4):374-382.
6. Harrel SK, Wilson TG Jr, Rivera-Hidalgo F. A videoscope for use in minimally invasive periodontal surgery. J Clin Periodontol.2013;40(9):
868-874.
7. Harrel SK, Abraham CM, Rivera-Hidalgo F. Tissue resistance to soft tissue emphysema during minimally invasive surgery. J Contemp Dent Pract.2012;13(6):886-891.
8. Harrel SK, Abraham CM, Rivera-Hidalgo F, et al. Videoscope-assisted minimally invasive periodontal surgery (V-MIS). J Clin Periodontol.2014;41(9):900-907.
9. Harrel SK, Abraham CM, Rivera-Hidalgo F, et al. Videoscope-assisted minimally invasive periodontal surgery: one-year outcome and patient morbidity. Int J Periodontics Restorative Dent.2016;36(3):363-371.
10. Harrel SK, Nunn ME, Abraham CM, et al. Videoscope assisted minimally invasive surgery (VMIS): 36-month results. J Periodontol. 2017;88(6):528-535.
11. Harrel SK, Valderrama P, Barnes JB, Blackwell EL. Frequency of root surface microgrooves associated with periodontal destruction. Int J Periodontics Restorative Dent. 2016;36(6):841-846.
12. Wilson TG Jr. A new minimally invasive approach for treating peri-implantitis. Clin Adv Periodontics.2019;9(2):59-63.
13. Wilson TG Jr, Valderrama P, Burbano M, et al. Foreign bodies associated with peri-implantitis human biopsies. J Periodontol. 2015;86(1):9-15.
14. Harrel SK, Wilson TG Jr, Tunnell JC, Stenberg WV. Laser identification of residual microislands of calculus and their removal with chelation. Submitted for publication.
15. Garrett S. Periodontal regeneration around natural teeth. Ann Periodontol. 1996;1(1):621-666.
16. Barrett CW, Harrel SK. Use of the dental videoscope in endodontics. Decisions in Dentistry.2017;3(4):16-22.
17. Drisko CL. Periodontal debridement: still the treatment of choice. J Evid Based Dent Pract.2014;14(suppl):33-41.