You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Patients are more likely to accept cosmetic concepts when they are educated by the clinician. When patients present to dental offices for cosmetic dentistry that incorporates implant dentistry, clinicians must be cognizant of hard- and soft-tissue availability for long-term function to deliver a desirable smile that meets the patients' expectations. Physically, candidates for the procedures should have an appropriate amount of bioavailability.
Hard- and Soft-Tissue Considerations
Dentists who provide cosmetic services and incorporate dental implants into treatment plans should have an awareness of hard and soft tissues in conjunction with the adjacent and opposing natural dentition. The best cosmetic results with natural dentition in the esthetic zone occur in those patients who present with a thicker soft-tissue profile and healthy alveolus that support the tooth and soft tissue in the absence of periodontal disease (gingival pockets greater than 3 mm, recession, and tooth mobility).1,2
Tooth position within the alveolus providing stable occlusal forces, along with space management and maintenance, also contribute to optimizing dental wellness and a desirable final result. If a clinician is trying to replicate a smile that mimics nature, the principles of space management and availability of existing bone and soft-tissue volumes should be considered.
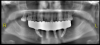
Figure 1 shows a comparison between natural dentition assembly and dental implant-tooth restoration assembly. If bone volume is sufficient to provide 1.5 to 2 mm of bone surrounding a dental implant (360 degrees), the dental implant should be placed into the center of the alveolus and will have an appropriate stable occlusal scheme3; then the functional and esthetic results can be achieved. Figure 2 depicts a cone-beam computed tomography (CBCT) image and virtual implant placement identifying 2 mm of bone surrounding the entire implant, centered within the maxillary alveolus.4 Dental imaging and treatment-planning software helps to develop surgical guides (placement guides or fully guided) to deliver implants, abutments, and final restorations with accuracy, consistency, and reproducibility.
Abutment Selection and Final Restoration Considerations
Abutment selection for single-unit cemented restorations has become computer-aided designed and computer-aided manufactured. The materials available for CAD/CAM abutments are zirconia ceramics, titanium, and lithium disilicate ceramics. Customization to achieve an adequate emergence profile with zirconia or lithium disilicate ceramics and their tooth-like characteristics achieve the translucencies that work well with ceramic final restorations. A study comparing zirconia abutments to alumina abutments showed that zirconia was 2.5 times more fracture resistant.5 The trend for metal-free abutments was also supported by a study showing less bacterial adhesion to zirconia than to titanium healing abutments.6 Choosing to use ceramic or metal abutments depends on angulation correction, soft-tissue profile, cosmetic zone, and space management of the final restoration. In the presence of parafunctional habits, metal abutments or zirconia abutments with ti-bases (hybrid ceramic abutments) should be considered. When failures of the ceramic hybrid abutment occur, they are due to metal fatigue of the retention screw.7 Ceramic hybrid bases are fabricated from titanium, assuring a precision fit of the ti-base to the titanium implant. The interface of the ceramic abutment and the ti-base features an anti-rotational design with the materials bonded to each other. In consideration of prefabricated stock abutments, there is a limit to customizing or preparing the abutment. The highest resistance to fractures of abutments has been demonstrated by metal-ceramic or full ceramic crowns on titanium abutments.8 Since the introduction of CAD/CAM abutment design, it has been possible to design restoration margins into the abutment that improve the soft-tissue situation for better control of cement removal.9
Restorative Vertical Height of Abutments
Restorative vertical height (RVH) is measured from the implant platform to the maximum distance to the incised or occlusal extent of the abutment superstructure. The internal connection of the abutment to the implant is an important success factor.10 RVH dimensions greater than 13 mm have higher fracture rates, especially in the anterior region when combined with parafunctional habits and are more common with bone-level implants than tissue-level implants.10
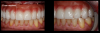
Figure 3 shows a ti-base connection, narrow emergence profile of the zirconia abutment (pink characterization), and final abutment with margins that were computer-generated and computer-manufactured to reflect the appropriate soft-tissue architecture for the patient. As shown in Figure 4, the abutment was seated and torqued to 25 Nm, allowed to rest for 10 minutes, and torqued once again to 25 Nm. The crown was tried in, fit was verified, and occlusion was established. This particular patient was concerned that the implant crown and implant would not look natural. Before beginning the single-tooth replacement with implant dentistry, a diagnostic wax-up and photographic imaging were employed to help develop a natural-looking provisional during the osseointegration phase. A treatment plan was developed and presented to the patient for considering cosmetic dentistry for tooth Nos. 6 through 11. The patient was still apprehensive and chose to begin therapy for only tooth No. 8. Since the final seat date, the patient has been very satisfied with the results of the single-tooth therapy and has committed to completing the cosmetic dentistry services for tooth Nos. 6 through 11.
Cementation
A classic cement such as a glass-ionomer should be considered for final cementation of the ceramic crown to either a titanium or zirconia abutment. Glass-ionomer cements allow excess cement to be removed more safely and have been shown to provide sufficient retention for crowns on dental implants during in vitro studies.11With clinical advantages of chemically bonding to tooth structure, glass-ionomer cements have a bacteriostatic effect, fluoride release, and adequate compressive and tensile strength. Glass-ionomer cements provide an acceptable option for final cementation of restorations for the long term. Additionally, among chief advantages seen with traditional glass-ionomers, resin-modified glass-ionomer cements have shown improvements in postoperative thermal sensitivity and are insoluble in the oral cavity.12Another option for final restoration and abutment alternatives is screw-retained hybrid abutment crowns (this alternative will not be discussed within this article).13
Creative Innovations in Digital Dentistry
Some situations within dentistry require creativity and use of technologic innovations to deliver esthetic and functional solutions for patients who may not want to spend much time in the dental office or may have difficulties with transportation to the dental facility. There are means of expediting treatment, particularly for the aging population. Figure 5 depicts a 94-year-old patient who had class 3 fractures with caries of dentin and cementum (non-restorable). With the aid of CBCT, photography, and intraoral scanning of a virtual model, a clinician can implement a fully guided surgical guide, abutments, and long-term polymethyl methacrylate (PMMA) provisional to be fabricated in a laboratory and delivered within 7 days. For this patient, extractions were completed atraumatically, implants seated with a fully guided surgical guide, ti-base abutments seated and verified with a periapical radiograph, and PMMA provisional placed on the same day and secured with screw retention (Figure 6).
The patient was seen at the 2-week postoperative evaluation appointment for observation and verification of stable occlusion (Figure 7). The patient was instructed to increase her oral hygiene home care and limit her diet to soft foods for an additional 3 months. After the 3-month healing phase, fabrication of a final 3-unit fixed restoration would begin. Using an implant with a pink collar provides a natural gingival color in the esthetic zone (Figure 8). In the event of gingival recession due to future bone loss, there is not the gray hew from the silver color of the implant platform.
Creativity within digital dentistry has made the process more efficient and proficient in developing cosmetic implant cases using multiple implants. Many patients present to the dental practice with periodontal concerns or carious lesions that require significant dentistry to help maintain their natural dentition. Patients who take responsibility for their dental wellness investigate the risks and benefits of traditional dentistry compared with removal of natural dentition and restoration with dental implants and computer-aided restorations.
Figure 9 and Figure 10 demonstrate the technology that the dentist and dental laboratory can accomplish within one appointment after diagnostic evaluations, virtual setups, and engineering for provisionals and final restorations. For this patient, occlusion was developed in the laboratory and delivered on surgery day (Figure 11). After 4 months of postoperative healing (Figure 12), the gingival tissues displayed keratinized tissue around the multi-unit abutments. The positive soft-tissue response was consistent with osseointegration of the dental implants. The final restoration was verified with digital scans and analog impressions of the PMMA provisional to replicate the soft-tissue architecture and occlusion related to the opposing arch. A computer-aided and milled zirconia screw-retained full-arch mandibular restoration was implemented, characterized to meet the patient's and dentist's expectations (Figure 13). After screw retention and occlusal verification, a CBCT image was taken to verify final seating of the restoration and radiographic evaluation of the implants (Figure 14).
For maxillary-arch cosmetic dentistry when considering dental implants, soft-tissue profile and bone volume are critical. Patient expectations are best met when the patient and dentist identify exactly what the patient desires in a smile. Patients normally desire as little maintenance as possible. The clinician must have an understanding not only of the physiologic and biologic availability, but also the amount of available space to provide the smile a patient desires and will be able to maintain with optimum oral hygiene and dental wellness.
At the time of consultation, a patient requested a cosmetic makeover without endodontic therapy and traditional crown-and-bridge. After discussing removable denture options and comparing fixed implant-supported full-arch zirconia, the patient felt the best concept for achieving his goals was to accept and commit to implant-supported full-arch restoration with zirconia. The initial diagnostic work-up included intraoral scanning to provide a digital impression of the maxillary and mandibular arches, CBCT, digital bite registration, and intraoral photography. The diagnostics revealed a requirement for bone reduction to allow enough restorative space to place implants at the correct level and have enough interocclusal distance to fabricate an ideal restoration. Figure 15 depicts a computer-designed chrome 3D-printed bone-reduction guide. After bone reduction and implant placement, multi-unit abutments (MUAs) with restorative cylinders were placed within the confines of the designed chrome indexing guide to relate the PMMA provisional to the bone-reduction guide and implant osteotomy assembly. Integrating digital technology with analog dentistry generates a smooth intaglio surface during the soft-tissue healing and osseointegration phases (Figure 16). On conversion of the PMMA provisional (luting the cylinders to the PMMA prosthesis) after implant placement, torqueing of the MUAs, and providing for balanced occlusion, the occlusal scheme and the midline were established. A 17-mm interocclusal dimension from the implant platform at the incised edges of the maxillary prosthesis was required (Figure 17). The central and lateral views showed a characterized PMMA that was acceptable to the patient in the esthetic zone. The flanges of the PMMA provisional were low-profile and created a ridge lap pontic throughout the restoration. The hygiene requirements for this provisional were light brushing and rinsing. Oral hygiene care with a water pick may begin 8 weeks after initial implant placement, after the integration and soft tissue have been completed.
Conclusion: Optimize Esthetics With a Pink Collar
Crowns fabricated from lithium disilicate or zirconia frameworks can be suitable superstructures cemented on titanium or zirconia hybrid abutments. The engineered materials have a failure mode that appears to protect the implant body. When considering patients with parafunctional habits, titanium abutments with lithium disilicate crowns should be considered.
In regard to cosmetics in dentistry within the esthetic zone, the clinician must evaluate the patient for appropriate amount of bone volume (approximately 2 mm completely around the implant) with a thick soft-tissue profile.3 Using the manufacturer's suggestions for implant placement and platform level also improves the cosmetic outcome. Long-term cosmetics may be compromised when bone or soft-tissue concerns are present. To help remedy this situation, the clinician can consider employing a dental implant that has an anodized pink platform (collar). If recession presents, the pink collar blends with the soft tissue and does not show the traditional gray hew of the underlying implant platform that appears when an anodized pink collar is not employed.
For cementation of single-unit ceramic crowns over titanium or zirconium abutments, the author's recommendation is glass-ionomer cement, which allows for safe removal of excess cement.
Smile design with implant dentistry in the esthetic zone can be worked up digitally with a qualified dental laboratory and expedited with predictable results. Computer-aided manufactured restorations are digitally created and can provide solutions for situations that require sophisticated analysis of space requirements that are not identified by traditional modalities within analog diagnostic techniques.
About the Author
Thomas M. Bilski, DDS
Private Practice
Independence, Ohio
References
1. Kois JC. Predictable single tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent. 2001;22(3):199-206.
2. Kois JC. Predictable single tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent. 2004;25(11):895-900.
3. Higginbottom FL, Wilson TG Jr. Three-dimensional templates for placement of root-form dental implants: a technical note. Int J Oral Maxillofac Implants. 1996;11(6):787-793.
4. Garber DA. The esthetic dental implant: letting restoration be the guide. J Oral Implantol. 1996;22(1):45-50.
5. Andersson B, Glauser R, Maglione M, Taylor A. Ceramic implant abutments for short-span FPDs: a prospective 5-year multicenter study. Int J Prosthodont. 2003;16(6):640-646.
6. Degidi M, Artese L, Scarano A, et al. Inflammatory infiltrate, microvessel density, nitric oxide synthase expression, vascular endothelial growth factor expression, and proliferative activity in peri-implant soft tissues around titanium and zirconia oxide healing caps. J Periodontol. 2006;77(1):73-80.
7. Silva NR, Teixeira HS, Silveira LM, et al. Reliability and failure modes of a hybrid ceramic abutment prototype. J Prosthodont. 2018;27(1):83-87.
8. Glauser R, Sailer I, Wohlwend A, et al. Experimental zirconia abutments for implant-supported single-tooth restorations in esthetically demanding regions: 4-year results of a prospective clinical study. Int J Prosthdont. 2004;17(3):285-290.
9. Obermeier M, Ristow O, Erdelt K, Beuer F. Mechanical performance of cement- and screw-retained all-ceramic single crowns on dental implants. Clin Oral Investig. 2018;22(2):981-991.
10. Fabbri G, Fradeani M, Dellificorelli G, et al. Clinical evaluation of the influence of connection type and restoration height on the reliability of zirconia abutments: a retrospective study on 965 abutments with a mean 6-year follow-up. Int J Periodontics Restorative Dent. 2017;37(1):19-31.
11. Garg P, Pujari M, Prithviraj DR, Khare S. Retentiveness of various luting agents used with implant-supported prosthesis: an in vitro study. J Oral Implantol. 2014;40(6):649-654.
12. Lowe RA. Dental cements: an overview. Dent Today. 2011;30(10):138-143.
13. Dehghan M, Braxton AD, Simon JF. An overview of permanent cements. Inside Dent. 2012;8(11).