You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Dental fusion is defined as the embryologic union of two separately developing tooth buds to form one tooth, with a confluence of dentin and/or enamel.1-4 The pulp chambers and canal may be joined or separate depending on the degree of development when the union occurs.5-7 Although the etiology is unknown, a force or physical pressure produces contact of the developing teeth that results in subsequent fusion and necrosis of the intervening tissues.8,9 Genes have been suggested as a cause.2,3,10 The extent of fusion depends on the degree of tooth development. The earlier fusion occurs, the more complete it is.3,9 If fusion occurs before the beginning of calcification, the union is complete, resulting in the formation of a single large tooth.11
In contrast, gemination is caused by the incomplete division of a single tooth bud, which results in a complete or incomplete crown with a single root and root canal system.10,12 Fusion can be clinically differentiated from gemination by a reduced number of teeth in the arch, unless fusion occurs with a supernumerary tooth.2,5,13 A full complement of teeth is indicative of gemination, whereas one tooth less than a full arch indicates fusion.5-7,10,13-16 The broad fused tooth may display clinically as a groove delineating two crowns, a bifid crown, or an incisal notch,1,6 and geminated teeth display clinically as mirror images of the joined crown.4,15 Radiographically, fused teeth tend to have a double pulpal space, while geminated teeth have an undivided pulp.6,14 The interdental cementum is generally absent between the fused roots.6
The incidence of these anomalies is more common in the primary dentition with an occurrence of 0.5% in contrast to 0.1% in permanent dentition.13-15,18 An investigation of 3517 plaster casts revealed 57.2% with this anomaly were fused and 42.9% were geminated.1,13 Dental fusion is more common in the anterior region and the mandible, and central incisors are most commonly affected, with an occurrence of 3.6%.12 Males and females are affected at equal rates.6,14,13,19
Tooth agenesis is one of the most common developmental anomalies. Agenesis occurs more frequently in permanent rather than primary teeth, with an occurrence of 1.6% to 10%, excluding third molars.20-22 Premolars and maxillary laterals are most commonly affected.23 Permanent maxillary laterals are absent in 1% to 2% of the population22 and account for approximately 20% of all cases of agenesis.21 Maxillary lateral incisors also display the highest genetic variability in the general population.20
The clinical problems associated with dental fusion and congenitally missing lateral incisors are both esthetic and functional and can include a lack of arch symmetry, diastemas, malocclusion, crowding, and protrusion, as well as dental caries.4,11,12,14 Periodontal problems can occur because of the presence of fissures or grooves in the union between fused teeth, and subgingival fissures can result in bacterial plaque accumulation.11Treatment in both cases requires a multidisciplinary approach.1,12,14,24-28
This case report reflects the 10-year documentation of a patient with both a fused central-lateral incisor and congenitally missing lateral incisor. The conservative, multidisciplinary treatment employed to restore esthetics and function is also described.
Clinical Report
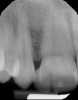
A 9-year-old girl, referred to a prosthodontic office by her pediatric dentist, presented with her mother’s chief complaint: “The kids are teasing her about her big front tooth.” Findings from radiographic and clinical examinations revealed fused maxillary central-peg lateral incisors, teeth Nos. 7 and 8, and a congenitally missing lateral incisor, tooth No. 10 (Figure 1 through Figure 3). An implant was selected as the ideal treatment to replace tooth No. 10 when somatic growth was complete. A diagnostic wax-up was fabricated to determine if the fused tooth could be made to resemble two teeth, using pink composite to give the illusion of an interproximal papilla. The patient was referred for an orthodontic consultation to plan for closure of the diastema between teeth Nos. 8 and 9 and achievement of proper alignment for implant No. 10. The patient was also referred to a periodontist for pretreatment assessment of the tooth No. 10 site. An endodontist was consulted should exposure of the large pulp occur during tooth preparation.
Using the wax-up as a guide, a composite restoration was fabricated for fused teeth Nos. 7 and 8 by roughening the affected area without pulpal exposure, etching the enamel, and applying primer and adhesive. Composite shade A1 was bonded to the mesial and distal surfaces, with gingival dark composite applied to the cervical “interproximal” region. The tooth was then carved to resemble two teeth, matching the width of the created tooth central to tooth No. 9 (Figure 4 and Figure 5). The patient and her family were very pleased with the result, and no postoperative sensitivity was reported.
The patient saw her pediatric dentist for regular maintenance, returning to the orthodontist for yearly assessments until she reached the age of 12 years, 1 month, at which time orthodontic therapy commenced. Fixed edgewise orthodontic therapy was performed for 2 years and 7 months to create an ideal space for implant tooth No. 10, close the diastema between teeth Nos. 8 and 9, and coordinate the facial-to-maxillary dental midlines (Figure 6). When the appropriate coronal and apical mesial-distal space was created by the orthodontist for implant placement (age 14 years, 3 months), a resin-bonded retainer was fabricated for optimal stability of coronal and root position,29 and cemented with a resin cement (Figure 7 and Figure 8). Also, a conventional removable retainer was delivered.
When the patient was age 17 years and 5 months, a cone-beam computed tomography (CBCT) scan30 was taken that revealed she had only 4.5-mm thickness of buccal/palatal alveolar ridge. The periodontist recommended lateral ridge augmentation to provide an additional 3 mm to 4 mm to achieve a stable long-term result.22,31 A root concavity on fused teeth Nos. 7 and 8 was also detected, which was thought to pose a complication for achievement of optimal gingival health.11 Alveolar bone augmentation of the buccal ridge at site No. 10 was performed. Following 6 months of healing, the second lateral cephalometric radiograph was taken by the orthodontist to verify cessation of somatic growth.29,31-33 Alginate impressions were taken by the prosthodontist to construct a surgical stent,34 and the final treatment plan was confirmed. As a result of the esthetic success achieved by the interim composite restoration, a lithium disilicate veneer35 using gingival porcelain to restore the missing interproximal papilla was proposed for fused teeth Nos. 7 and 8. The patient also requested a veneer for the adjacent central incisor, tooth No. 9. A ceramic implant crown and custom abutment were planned for site No. 10.
When the patient was 18 years old, an implant was placed in site No. 10 with no complications (Figure 9 and Figure 10). Three months later, a periapical radiograph was taken, the implant was torque tested, and a healing abutment (3 mm by 4 mm by 4 mm) was placed.
Two-and-a-one-half weeks later, the prosthodontist made an open-tray implant-level impression, which was sent to the laboratory for creation of a soft-tissue model, custom abutment, provisional, and zirconia coping. The 3-mm custom abutment was inserted with a resin jig and, on verification with a periapical radiograph, torqued to 15 Ncm, according to the manufacturer’s recommendation. The provisional was placed and modified following initial tissue blanching to raise and scallop the tissue, develop a proper emergence profile, and prosthetically guide the soft-tissue development.34 After the screw-access hole was filled with polytetrafluoroethylene tape, the provisional was cemented by carefully painting a thin layer of temporary cement to minimize excess and meticulously checked for complete cement removal.
Following soft-tissue maturation, the desired shades with characterization were selected including the gingival shade for the pink porcelain, and fused teeth Nos. 7 to 8 and tooth No. 9 were prepared for veneers (Figure 11). Care was taken to dip into the preparation facially at the interface between the proposed central-lateral teeth, and shorten the distal-incisal to provide room for the laboratory to create the appearance of two separate teeth with a shorter lateral incisor. Retraction cord was placed for gingival displacement, the zirconia coping was inserted on the implant abutment, and an impression of the fused teeth Nos. 7 and 8 and tooth No. 9 was made, picking up the zirconia coping (Figure 12).
When the patient was 19 years old, the lithium-disilicate veneers and the ceramic crown were tried in and evaluated. Following modification, the veneers were carefully cemented with an adhesive resin cement following application of silane to the intaglio surfaces, etch of the enamel, and application of primer and adhesive. The intaglio surface of the implant crown was treated with a porcelain etch product and silane, and the crown was cemented with carboxylate luting cement with 1 drop of water for retrievability. A paintbrush was used to apply a thin layer of cement to minimize excess. Any excess cement on the veneers and crown was meticulously removed, and the margins and occlusion were carefully checked. The patient returned 2 weeks later (Figure 13 through Figure 18) for a review of her oral hygiene and for fabrication of a nightguard. The patient was happy with the esthetic result and exclaimed she had been stopped on the street and told she had a beautiful smile.
Discussion
This clinical report describes a conservative approach to restoring esthetics, function, and occlusion in cases of dental fusion and congenitally missing lateral incisors. An interdisciplinary approach in treatment planning and execution is essential to provide the patient with optimal care.11,13,18,25,27,29,36
Treatment alternatives for patients with congenitally missing lateral incisors have included orthodontic treatment with canine substitution, conventional fixed bridgess, cantilevered fixed partial dentures, resin-bonded bridges, removable partial dentures, autotransplantation, and single-tooth implants.26,29,31,35-37 Canine substitution can be considered in cases of angle class II malocclusion with no crowding in the mandibular arch, angle class I malocclusion with mandibular crowding necessitating extractions, and canines with similar width and convexity to the lateral incisor and similar color to the central incisor.22,29
While minimal reduction is necessary for resin-bonded bridges, a shallow overbite with moderate thickness of the abutment teeth is preferable to allow a maximum surface for bonding and a reduction of lateral forces.31,38 Contraindications for placement of resin-bonded fixed partial dentures include mobility of the abutment teeth, parafunction, deep overbite, and proclined teeth.31,38 The failure rates range from 54% for 11 months to 10% for 11 years, with debonding being the most frequent cause.22,39,40
A cantilevered fixed partial denture is an option using the canine as an abutment, which can be ideal given its root length and crown dimensions.39 This restoration is independent of the degree of proclination or mobility of the abutment tooth, and can employ partial coverage with pins for retention and resistance if the size and location of the pulp permit. The success of a cantilevered fixed partial denture is dependent on the control of occlusal forces on the pontic, and all excursive contacts on the cantilever must be eliminated. If eccentric contact is present on the cantilever, risks include loosening of the restoration, migration of the abutment tooth, and/or fracture.22,31,39
Autotransplantation of a premolar is another treatment alternative, but is technique sensitive and the timing is critical. The optimal time for autotransplantation is when the premolar root has reached two-thirds to three-quarters of its final length, usually in a patient 9 to 12 years old. This results in periodontal healing of more than 90%, with continuation of root growth after transplantation.22,37 Reports of autotransplantation success are 79% to 90%.37,38 However, any damage to the periodontal ligament can result in ankylosis.22,37
The least conservative restoration is a conventional full-coverage fixed partial denture, which may be considered when adjacent teeth require full-coverage restorations because of extensive caries or fractures.22,31 Placing crowns on adjacent teeth for young patients in cases of agenesis is considered by many to be inappropriate if these teeth have no restorations or wear.21,22
Ideally, the treatment selected to restore congenitally missing laterals should be the least invasive option that satisfies esthetic and functional criteria.31 Implant-supported restorations offer high success rates with a survival rate of 96.8% at 5 years,41 maintain the alveolar ridge, enhance function and esthetics, and may be regarded as the most conservative approach by leaving the adjacent teeth untouched.22,32,35
When implants are selected, they should be placed only after the completion of somatic growth,21,22,31-34,40 which is generally finished in females at ages 16 to 17 years and in males ages 20 to 21 years.31 If an implant is placed and restored too early, the adjacent teeth may continue to erupt while the implant mimics an ankylosed tooth, resulting in a discrepancy in the gingival margins and the creation of periodontal, occlusal, and restorative problems.31-34,40 If the canine has erupted into the site of the missing lateral, distal movement of the canine through “orthodontic site development” will create adequate buccolingual alveolar width through stretching of the periodontal ligament.21,33,34 When the canine has not erupted into the lateral site, the osseous ridge will not fully develop.22,33,38 The alveolar ridge thickness may need to be augmented to provide implant support and a stable esthetic soft-tissue framework for the implant restoration.27,31 The use of CBCT scans can improve the assessment of the implant receptor site, and interactive virtual treatment software enhances surgical and prosthetic treatment planning.30
Many approaches have been suggested to restore cases of dental fusion to enhance esthetic display. These include extraction of the fused tooth, followed by orthodontic therapy and a resin-bonded retainer with possible future implants;16 endodontic therapy with periodontal surgery to reduce the root diameter and narrow the emergence profile, followed by a cast post and metal-ceramic crown;10 and endodontic therapy and veneering with tooth-colored and pink composite.28
When the fusion involves a supernumerary tooth, treatment options have included extraction with orthodontic therapy and lateral substitution for a fused central, followed by a porcelain veneer;42 a mucoperiosteal flap with separation and removal of the supernumerary tooth (although this can result in gingival inflammation and periodontal pocketing); or extraction of the fused tooth, with extraoral separation and reimplantation.1 Risks for this latter technique include periodontal inflammation and probing depth, but with a high risk for pulpal necrosis, ankylosis, and external or internal resorption.1,42,43 Additional treatment options have included endodontic therapy or partial pulpotomy, hemisection of the supernumerary tooth, restoration with composite, free gingival graft, and orthodontic therapy.1,44
One of the challenges in esthetically restoring a broad tooth in cases of dental fusion involves replication of the missing dental papilla. Adhesive dentistry has been employed to bond pink composite cervically between the fused central and lateral incisors, followed by closure of a diastema with composite resin and orthodontic therapy.13 Endodontic therapy with a labial access, followed by preparation and veneering with resin using pink composite in the gingival embrasure region, has also been used.28 A metal-ceramic crown with pink porcelain in the gingival embrasure following endodontic therapy, a periodontal flap to reduce the root diameter and narrow the emergence profile, and a cast post and core have been suggested.10 Recently, application of a ceramic veneer with pink porcelain to replicate the interdental papilla and simulate the presence of two teeth has been reported.45
The advantage of a porcelain veneer versus a less conservative approach is that it achieves excellent esthetics without extensive tooth removal.46,47 A minimally invasive procedure allows preservation of enamel to optimize the adhesive bond of the luting agent between the tooth and ceramic restoration.35 Porcelain veneers also offer higher fracture strength because of the bond of resin cement to enamel, resulting in high survival rates with low failure rates.47-52 Lithium disilicate provides a high flexural strength (350 MPa to 400 MPa) and excellent esthetics and can be milled using computer-aided design/computer-aided manufacturing.35 In addition, the bond strength of lithium-disilicate restorations is increased when resin-luting cements are employed.35
Conclusion
A conservative multidisciplinary approach has been presented to restore a case of dental fusion and a congenitally missing lateral incisor. Treatment included tooth-colored and pink composite resin to improve dental esthetics, orthodontic co-therapy, a resin-bonded retainer to maintain the space created for an implant, a series of lateral cephalometric radiographs to confirm completion of bone growth, a CBCT scan to evaluate the alveolar ridge thickness, bone graft, and implant placement. The final prostheses employing a lithium disilicate veneer using gingival porcelain to give the illusion of two teeth with a papilla and a ceramic implant crown reflect a conservative approach to improvement of the patient’s occlusion, dental esthetics, and self-esteem.
Acknowledgments
The authors would like to thank Noriyuki Kajita, CDT, and Cusp Dental Laboratory for their outstanding care; Patricia Heller, head librarian at the University of Pennsylvania School of Dental Medicine, for her invaluable help; and Francine Paladino, DMD, Louis E. Rossman, DMD, and Carole Hildebrand, DDS (deceased), for their contributions.
About the Authors
Leslie Stone Hirsh, DDS
Clinical Assistant Professor of Restorative Dentistry, University of Pennsylvania School of Dental Medicine, Philadelphia, Pennsylvania; Prosthodontist, Private Practice, Philadelphia, Pennsylvania
Peter M. Greco, DMD
Clinical Professor, Co-Clinical Director, Department of Orthodontics, University of Pennsylvania School of Dental Medicine, Philadelphia, Pennsylvania; Adjunct Instructor, Department of Oral and Maxillofacial Surgery, Thomas Jefferson University Hospital, Philadelphia, Pennsylvania; Orthodontist, Private Practice, Philadelphia, Pennsylvania, and Ardmore, Pennsylvania
Jay B. Laudenbach, DMD
Periodontist, Private Practice, Philadelphia, Pennsylvania
Alan M. Atlas, DMD
Clinical Professor of Restorative Dentistry, University of Pennsylvania School of Dental Medicine, Philadelphia, Pennsylvania; Private Practice, Philadelphia, Pennsylvania
Queries to the authors regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Karacay S, Guven G, Koymen R. Management of a fused central incisor in association with a macrodont lateral incisor: a case report. Pediatr Dent. 2006;28(4):336-340.
2. Chipashvili N, Vadachkoria D, Beshkenadze E. Gemination or fusion?—challenge for dental practitioners (case study). Georgian Med News. 2011;(194):28-33.
3. Ballal NV, Kundabala M, Acharya S. Esthetic management of fused carious teeth: a case report. J Esthet Restor Dent. 2006;18(1):13-17; discussion 18.
4. Mohan RP, Verma S, Singh AK, Singh U. Double tooth in mandibular incisor region: a case report. BMJ Case Rep. 2013; doi:10.1136/bcr-2013-008647.
5. Duncan WK, Helpin ML. Bilateral fusion and gemination: a literature analysis and case report. Oral Surg Oral Med Oral Pathol. 1987;64(1):82-87.
6. Schuurs AH, van Loveren C. Double teeth: review of the literature. ASDC J Dent Child. 2000;67(5):313-325.
7. Killian CM, Croll TP. Dental twinning anomalies: the nomenclature enigma. Quintessence Int. 1990;21(7):571-576.
8. Shafer WG, Hine MK, Levy BM. A Textbook of Oral Pathology. 3rd ed. Philadelphia, PA: W.B. Saunders Co.; 1974.
9. Lowell RJ, Solomon, AL. Fused teeth. J Am Dent Assoc. 1964;68:762.
10. Trebilcock CE, Mealey BL, Dickson SS. Multidisciplinary restoration of fused maxillary incisors: a case report. Pract Periodontics Aesthet Dent. 1995;7(4):47-53; quiz 54.
11. Hans MK, Shetty S, Chopra H. Bilateral fusion of permanent maxillary incisors. Indian J Dent Res. 2011;22(4):603-605.
12. Kalwitzki M, Krastl G. A minimally invasive approach in the interdisciplinary treatment of four fused maxillary incisors: a case report. J Adhes Dent. 2007;9(3):341-347.
13. Knezevic A, Travan S, Tarle Z, et al. Double tooth. Coll Antropol. 2002;26(2):667-672.
14. Tuna EB, Yildirim M, Seymen F, et al. Fused teeth: a review of the treatment options. J Dent Child (Chic). 2009;76(2):109-116.
15. Kelly JR. Gemination, fusion, or both? Oral Surg Oral Med Oral Pathol. 1978;45(4):655-656.
16. Crawford NL, North S, Davidson LE. Double permanent incisor teeth: management of three cases. Dent Update. 2006;33(10):608-610.
17. Marechaux SC. The treatment of fusion of a maxillary central incisor and a supernumerary: report of a case. ASDC J Dent Child. 1984;51(3):196-199.
18. Iodice G, Paduano S, Cioffi I, et al. Multidisciplinary management of double-tooth anomalies. J Clin Orthod. 2009;43(7):463-469.
19. Nik-Hussein NN. Double teeth—fusion or gemination? Odontostomatol Trop. 1992;15(1):16-18.
20. Park JH, Okadakage S, Sato Y, et al. Orthodontic treatment of a congenitally missing maxillary lateral incisor. J Esthet Restor Dent. 2010;22(5):297-312.
21. de Avila ED, de Molon RS, de Assis Mollo F Jr, et al. Multidisciplinary approach for the aesthetic treatment of maxillary lateral incisors agenesis: thinking about implants? Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114(5):e22-e28.
22. Krassnig M, Fickl S. Congenitally missing lateral incisors—a comparison between restorative, implant, and orthodontic approaches. Dent Clin North Am. 2011;55(2):283-299.
23. Mangano C, Levrini L, Mangano A, et al. Esthetic evaluation of implants placed after orthodontic treatment in patients with congenitally missing lateral incisors. J Esthet Restor Dent. 2014;26(1):61-71.
24. Martinez-Rus F, Rivera B, Ozcan M, Pradies G. Prosthodontic considerations in the implant-supported all-ceramic restoration of congenitally missing maxillary lateral incisor: a clinical report. J Prosthodont. 2014;23(3):232-235.
25. Muller TP, Hill IN, Peterson AC, Blayney JR. A survey of congenitally missing permanent teeth. J Am Dent Assoc. 1970;81(1):101-107.
26. Gautam G, Kumari VS, Jayashankar CM, et al. Interdisciplinary management of dental anomalies: fusion and supernumerary teeth. Orthodontics (Chic). 2011;12(2):140-147.
27. Patil PG, Karemore V, Chavan S, et al. Multidisciplinary treatment approach with one piece implants for congenitally missing maxillary lateral incisors: a case report. Eur J Prosthodont Restor Dent. 2012;20(2):92-96.
28. Veeraiyan DN, Fenton A. Dental fusion: a case report of esthetic conservative management. Quintessence Int. 2009;40(10):801-803.
29. Kokich VO Jr, Kinzer GA. Managing congenitally missing lateral incisors. Part I: Canine substitution. J Esthet Restor Dent. 2005;17(1):5-10.
30. Ganz SD. Defining new paradigms for assessment of implant receptor sites: the use of CT/CBCT and interactive virtual treatment planning for congenitally missing lateral incisors. Compend Contin Educ Dent. 2008;29(5):256-258, 260-262, 264-267; quiz 268.
31. Kokich VO Jr, Kinzer GA, Janakievski J. Congenitally missing maxillary lateral incisors: restorative replacement. Am J Orthod Dentofacial Orthop. 2011;139(4):435, 437, 439, 441, 443, 445.
32. Richardson G, Russell KA. Congenitally missing maxillary lateral incisors and orthodontic treatment considerations for the single-tooth implant. J Can Dent Assoc. 2001;67(1):25-28.
33. Kokich VG. Maxillary lateral incisor implants: planning with the aid of orthodontics. J Oral Maxillofac Surg. 2004;62(9 suppl 2):48-56.
34. Kinzer GA, Kokich VO Jr. Managing congenitally missing lateral incisors. Part III: Single-tooth implants. J Esthet Restor Dent. 2005;17(4):202-210.
35. Fradeani M, Barducci G, Bacherini L. Esthetic rehabilitation of a worn dentition with a minimally invasive prosthetic procedure (MIPP). Int J Esthet Dent. 2016;11(1):16-35.
36. Polder BJ, Van’t Hof MA, Van der Linden FP, Kuijpers-Jagtman AM. A meta-analysis of the prevalence of dental agenesis of permanent teeth. Community Dent Oral Epidemiol. 2004;32(3):217-226.
37. Zachrisson BU, Stenvik A, Haanaes HR. Management of missing maxillary anterior teeth with emphasis on autotransplantation. Am J Orthod Dentofacial Orthop. 2004;126(3):284-288.
38. Janakievski J. Avulsed maxillary central incisors: the case for autotransplantation. Am J Orthod Dentofacial Orthop. 2012;142(1):9, 11, 13, 15, 17.
39. Kinzer GA, Kokich VO Jr. Managing congenitally missing lateral incisors. Part II: Tooth-supported restorations. J Esthet Restor Dent. 2005;17(2):76-84.
40. Beyer A, Tausche E, Boening K, Harzer W. Orthodontic space opening in patients with congenitally missing lateral incisors. Angle Orthod. 2007;77(3):404-409.
41. Jung RE, Pjetursson BE, Glauser R, et al. A systematic review of the 5-year survival and complication rates of implant-supported single crowns. Clin Oral Implants Res. 2008;19(2):119-130.
42. Brook AH, Winter GB. Double teeth. A retrospective study of ‘geminated’ and ‘fused’ teeth in children. Br Dent J. 1970;129(3):123-130.
43. Rajab LD, Hamdan MA. Supernumerary teeth: review of the literature and a survey of 152 cases. Int J Paediatr Dent. 2002;12(4):244-254.
44. Beier US, Dumfahrt H, Widmann G, Puelacher W. Surgical resection technique of a fused supernumerary lateral incisor: a clinical report and review of the literature. Gen Dent. 2012;60(4):e268-e273.
45. Cordeiro WJ, do Couto CF, Barros RN, et al. Esthetic management of double tooth associated with talon cusp using a laminate veneer. J Dent Child (Chic). 2014;81(3):161-170.
46. Reshad M, Geller W, Cascione D. An ultraconservative approach to porcelain veneers in the 21st century. Quintessence Dent Technol. 2011;34:193-199.
47. Pimentel W, Teixeira ML, Costa PP, et al. Predictable outcomes with porcelain laminate veneers: a clinical report. J Prosthodont. 2016;25(4):335-340.
48. Gurel G, Sesma N, Calamita MA, et al. Influence of enamel preservation on failure rates of porcelain laminate veneers. Int J Periodontics Restorative Dent. 2013;33(1):31-39.
49. Edelhoff D, Sorensen JA. Tooth structure removal associated with various preparation designs for anterior teeth. J Prosthet Dent. 2002;87(5):503-509.
50. Piemjai M, Arksornnukit M. Compressive fracture resistance of porcelain laminates bonded to enamel or dentin with four adhesive systems. J Prosthodont. 2007;16(6):457-464.
51. Peumans M, Van Meerbeek B, Lambrechts P, Vanherle G. Porcelain veneers: a review of the literature. J Dent. 2000;28(3):163-177.
52. Cotert HS, Dundar M, Ozturk B. The effect of various preparation designs on the survival of porcelain laminate veneers. J Adhes Dent. 2009;11(5):405-411.