You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Although digital chairside technology (ie, CAD/CAM) has been available for many years in dentistry, it has provoked mixed reviews in the eyes of clinicians. Dental professionals have perceived multiple barriers to it, including those related to cost, access, accuracy, support, and indications, among others. Consequently, this has led to a delayed adoption of the technology. More recently, the profession has seen numerous changes and offerings that have altered perceptions, and we are now seeing more rapid adoption. One of the many reasons posited for this increase in adoption is the increased availability of materials for milling, including zirconia.
CAD/CAM dentistry was first introduced in 1971 by François Duret, DDS, DSO, MS, PhD; however, Werner Mörmann, BMD, DDS, was the first to bring the concept into clinical practice. Mörmann placed the first inlay in 1985, and the CEREC 1 was brought to market in 1987. This original CEREC system was limited to inlays and onlays.1 The goal of CAD/CAM dentistry was to scan, design, and mill a restoration in a single visit. At the outset, the material choices available to fulfill this goal were limited. In addition, the dental laboratory was removed from the equation. Much has changed since 1971. During the past several years, the landscape has become more diverse as many other dental manufacturers have developed digital products. Multiple scanners, mills, and material choices have been introduced, and multiple indications are also now available. The end result is that from 2017 to 2023, the global dental CAD/CAM market is predicted to experience a compounded annual growth rate of 9.4%.2
CAD/CAM Material Progression
Since the inception of CAD/CAM dentistry, multiple generations of ceramics have become available. The first documented restoration (an inlay) placed using CAD/CAM chairside technology in 1985 utilized a feldspathic porcelain block (VITABLOCS® Mark I, VITA Zahnfabrik).1 Throughout the years, feldspathic porcelains have undergone numerous compositional changes, and the success of these restorations has been well documented. In 1991, the second generation feldspathic porcelain block (VITABLOCS Mark II, VITA Zahnfabrik) was released and proven to be very successful as well.3-7
In 1998, a leucite-reinforced ceramic (Pro CAD, Ivoclar Vivadent) was introduced. The addition of leucite was found to increase the strength when compared with the previously introduced blocks.4,5 Increased strength was one of the many advancements; however, possibly the most substantial introduction to the ceramic family also occurred in the same year with the introduction of IPS Empress® II (Ivoclar Vivadent). This newer ceramic boasted an improved strength of 350 MPa and a greater translucency than the previous versions of leucite-reinforced glass ceramics.
Empress II was eventually replaced by a lithium disilicate glass ceramic (IPS e.max® CAD, Ivoclar Vivadent), which had an even greater strength (≥ 360 MPa), as well as improved optical properties.8 Despite the greater strengths of these newer ceramics, they remained brittle. In other words, the compressive strength was improved, but the tensile strength remained low, which led to the potential for fracture under low strain.9 The final strength is determined after a firing cycle, according to the manufacturer's recommendations.
In 1999, a new classification of materials for CAD/CAM milling systems was introduced. These materials were composite resin blocks, the first of which was Paradigm™ MZ100 (3M). This material served many of the needs of the CAD/CAM dentist. The block was easy to use, easy to adjust, and did not require firing. The strength of these blocks (approximately 130 MPa) was less than what was initially desired when compared with other ceramics, but they were less brittle and more wear-friendly to the opposing dentition.10,11
It was not until several years later that a new classification of materials was introduced-hybrid ceramics. These materials employ ceramic particles that are suspended in a resin matrix. The development of the first hybrid ceramic was unique in that it was designed in an attempt to develop a material that behaved similarly to human dentin.12 The first documented material of this classification was VITA ENAMIC® (VITA Zahnfabrik). Similar to the previously released composite blocks, hybrid ceramics were attractive to clinicians as well. These blocks were esthetically appealing and did not need to be fired after milling to maximize their strength.
During the next several years, many manufacturers would produce their own versions of a hybrid ceramic. The goals of these materials were all the same, and they all had very similar characteristics. They only varied in terms of the percentage of filler used and the actual composition of the filler and the resin matrix. The flexural strength of these materials was found to range from as low as 150 to 160 MPa (eg, VITA ENAMIC) to as high as 238 MPa (eg, CERASMART®, GC America).12,13
The aforementioned materials have been in service for many years, and there has been great success reported with their use in chairside CAD/CAM dentistry. However, newer demands from clinicians have placed newer demands on materials. Clinicians have long been seeking a material that is strong, tooth-colored, biocompatible, and a suitable replacement for gold and porcelain-fused-to-metal restorations. Zirconia, an oxide ceramic, is a robust material with the potential to meet these demands.
Zirconia as a Chairside CAD/CAM Material
Zirconia (zirconium dioxide [ZrO2]) was introduced as a material for traditional crown and bridge dentistry in the late 1990s; however, it did not really take off as a predominant material used by clinicians until several years later.14 In 2017, Glidewell Laboratories reported that both zirconia and zirconia-based restorations comprised more than 75% of all restorations fabricated by their laboratory.15
Along with its predecessor alumina, zirconia is a member of a larger group of ceramics that are often referred to as polycrystalline ceramics. Zirconia differs from alumina in that it transforms crystalline states when fired. Zirconia exists in the following three states: monoclinic, tetragonal, and cubic. The addition of stabilizing oxides, such as ceria (CeO2), yttria (Y2O3), alumina (Al2O3), magnesia (MgO), and calcia (CaO), minimizes fractures during heat processing and renders the material stable post-firing. This transformation increases both the fracture toughness and strength of the material.16,17
Since its introduction, several generations of dental zirconia have been created. The difference in the generations of zirconia lies mainly in the content of yttria (Y2O3), and thus is referred to in that manner. The first generation contains 3 molar percentage (3 mol%) yttria, and the other popular generations contain 4 mol% yttria and 5 mol% yttria, respectively. The first generation offered many great attributes, including a low cost of fabrication, high strength, a low potential to be clinically problematic, biocompatibility, and reduced wear on the opposing dentition.18 Although their strength is slightly less than the 3 mol% yttria-stabilized zirconia, the 4 mol% and 5 mol% are still stable and desirable for dental restorations. Other than strength, the main difference is that the additional yttria composition provides a more favorable translucency and improved optics because the phase of the material leans toward being more cubic and less tetragonal. A fully cubic phase is considered unstable because it does not exhibit transformation toughening, rendering the material weak.19
Although the most favorable feature that zirconia offers is strength, it also provides a tooth-colored restoration and other characteristics that are desirable to both the dentist and the patient. It was not until 2013 that a solution was developed to enable dentists to provide zirconia restorations to patients using a same-day procedure. At that time, several companies, such as Glidewell Dental, Kuraray Noritake Dental, 3M, Dentsply Sirona, and Ivoclar Vivadent, developed materials that made zirconia a valid offering in the chairside CAD/CAM setting, including the following:
BruxZir® NOW
BruxZir® NOW (Glidewell Laboratories) was introduced in 2013. Available in 14 VITA classical shades, this material was the first of its kind in the classification of chairside zirconia. The restorations produced with these blocks can be designed, fabricated, and made ready for placement in less than 45 minutes. These blocks are pre-sintered, which means that they are milled in the final state and that no firing of the restoration is necessary after milling. In addition, the restorations do not need to be stained or glazed, so any characterization is entirely at the discretion of the dentist. Regarding strength, the flexural strength achieved has been measured to be at greater than 1,100 MPa.20
The material is only available for single-unit, full-coverage restorations, and the minimum depth of preparation recommended by the manufacturer is 0.7 mm (Figure 1).20
KATANA™ Zirconia Block
The KATANA™ Zirconia Block (Kuraray Noritake Dental Inc.) also does not require staining. It consists of four layers of zirconia in graduated shades that allow for a more natural appearance. The manufacturer claims that restorations can be scanned, designed, milled, and sintered in less than 35 minutes. It is available in 15 VITA classical shades, and its flexural strength is approximately 763 MPa.21
KATANA is indicated for anterior crowns, posterior crowns, veneers, inlays, and onlays. The preparation can be as minimal as 0.4 mm for a veneer; however, a full 1.0 mm is recommended for a posterior crown. KATANA is milled in its non-sintered state, and it is recommended that clinicians mill it in dry mode (ie, for approximately 15 minutes). The restoration is then finished by firing it in an oven (ie, for 18 minutes if the walls are less than 3 mm in thickness).21
3M™ Chairside Zirconia
The newest member to this category of zirconia is 3M™ Chairside Zirconia (3M). The material was released in 2019. It is unique among the others in this category in that it boasts high strength and translucency, being 75% tetragonal, 25% cubic, and a 4 mol% yttria-stabilized zirconia. For thinner restorations, the estimated firing time post-milling is 20 minutes, which results in a design-to-seat time of less than 1 hour. It is available in 8 VITA classical shades, and the flexural strength of the material is greater than 1,000 MPa.19,22
3M™ Chairside Zirconia is indicated for single-unit crowns and 3-unit bridges. Per the manufacturer, the minimal thickness of preparation required is 0.8 mm. In addition, the blocks are available in 39 mm and 20 mm, based on whether or not a bridge is the desired restoration.19,22
Case Presentation
A 61-year-old female patient presented with a failed alloy restoration and missing the entire lingual surface of tooth No. 19 (Figure 2 and Figure 3). The argument could have been made to use either an onlay or a crown to replace the affected tooth. With the extent of the missing tooth structure, the malocclusion, and the patient's history of bruxism, treatment with a full-coverage restoration was selected to maximize longevity.
When contemplating material choices, zirconia seemed to be an optimal choice for this case. As previously mentioned, the material has an immense amount of strength, is tooth colored, and is friendlier to the opposing dentition than glazed glass ceramics.23-25
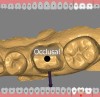
After the patient was anesthetized, the failing alloy restoration was removed along with the recurrent decay. A buildup was placed using bulk-fill composite and an adhesive bonding agent. Following preparation (Figure 4 and Figure 5), a No. 1 cord was placed in the sulcus, and then the preparation, working quadrant, opposing quadrant, and bite were scanned using an intraoral scanner.
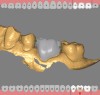
Following the digital impression, the digital design was created in the design software and sent to the in-office mill (Figure 6 through Figure 8). The milling process took 38 minutes, and there was no need to add glaze to or fire the restoration because the material was milled in a fully sintered phase.
After milling, the sprue was easily removed, and the restoration was polished in a matter of minutes using polishers in the appropriate sequence (Figure 9). Prior to cementation, the intaglio surface of the restoration was air abraded with 30-µm aluminum oxide particles coated in silica and then silanated using a universal primer.
Once the restoration was prepared, it was placed with a self-adhesive resin cement (Figure 10 and Figure 11). With zirconia restorations, multiple cements can be used. They can either be luted with resin-modified glass ionomers or bonded with dual-cure self-adhesive or adhesive resins. All cements and bonding agents should be used according to the manufacturer's recommendations. Zirconia restorations that lack retentive properties (eg, < 3 to 4 mm in height, 5º to 6º taper) should be adhesively bonded; all others can be luted.
Conclusion
Multiple material choices for chairside CAD/CAM restorations exist that can provide patients with favorable results. Factors such as strength, translucency, fabrication requirements, and more need to be taken into consideration when choosing between these materials for same-day restorations. Zirconia provides clinicians with a newer alternative that possesses both strength and esthetic properties. Dental materials are constantly advancing, and chairside zirconia has proven to be a great addition to the clinician's armamentarium.
About the Author
Chad C. Duplantis, DDS
Fellow
Academy of General Dentistry
Private Practice
Fort Worth, Texas
References
1. Mörmann WH, Bindl A. All-ceramic, chair-side computer aided design/computer-aided machining restorations. Dent Clin North Am. 2002;46(2):405-426.
2. Allied Market Research. Dental CAD/CAM Materials & Systems Market by Product - Global Opportunity Analysis and Industry Forecast, 2017-2023. Allied Market Research web site. https://www.alliedmarketresearch.com/dental-CAD-CAM-materials-and-systems-market. Published June 2017. Accessed July 24, 2019.
3. Li R, Kim W. Ceramic dental biomaterials and CAD/CAM technology: state of the art. J Prosthodont Res. 2014;58(4):208-216.
4. Fasbinder DJ. Restorative material options for CAD/CAM restorations. Compend Contin Educ Dent. 2002;23(10):911-916, 918, 920 passim; quiz 924.
5. Chen HY, Hickel R, Setcos JC, et al. Effects of surface finish and fatigue testing on the fracture strength of CAD-CAM and pressed-ceramic crowns. J Prosthet Dent. 1999;82(4):468-475.
6. Zimmer S, Göhlich O, Rüttermann S, et al. Long-term survival of Cerec restorations: a 10-year study. Oper Dent. 2008;33(5):484-487.
7. Otto T, de Nisco S. Computer-aided direct ceramic restorations: a 10-year prospective clinical study of Cerec CAD/CAM inlays and onlays. Int J Prosthodont. 2002;
15(2):122-128.
8. Zarone F, Ferrarri M, Mangano FG, et al. Digitally oriented materials: focus on lithium disilicate ceramics. Int J Dent. 2016;2016:9840594. doi: 10.1155/2016/9840594.
9. Shenoy A, Shenoy N. Dental ceramics: an update. J Conserv Dent. 2010;13(4):195-203.
10. 3M Dental Products. 3M Paradigm™ MZ100 Block Technical Product Profile. 3M web site. http://multimedia.3m.com/mws/media/77596O/3m-paradigm-mz100-block-for-cerec-technical-product-profile.pdf.Published 2000 Accessed July 24, 2019.
11. Lawson NC, Bansal R, Burgess JO. Wear, strength, modulus and hardness of CAD/CAM restorative materials. Dent Mater. 2016 Nov;32(11):e275-e283.
12. VITA Zahnfabrik. VITA ENAMIC - the first hybrid dental ceramic in the world. VITA Zahnfabrik web site. https://www.vita-zahnfabrik.com/en/VITA-ENAMIC-the-first-hybrid-dental-ceramic-in-the-world-4682,57329.html. Published September 24. 2012. Accessed July 24, 2019.
13. GC America. CERASMART® force absorbing, flexible nano ceramic CAD/CAM block. GC America web site. http://www.gcamerica.com/products/digital/CERASMART/index2.php. Accessed July 24, 2019.
14. Vagkopoulou T, Koutayas SO, Koidis P, et al. Zirconia in dentistry: part 1. Discovering the nature of an upcoming bioceramic. Eur J Esthet Dent. 2009;4(2):130-151.
15. Data on file, Glidewell Dental Laboratories. (2018). Newport Beach, CA.
16. Kelly JR, Benetti P. Ceramic materials in dentistry: historical evolution and current practice. Aust Dent J. 2011;56(Suppl 1):84-96.
17. Bona AD, Pecho OE, Alessandretti R. Zirconia as a dental biomaterial. Materials (Basel). 2015;8(8):4978-4991.
18. Christensen, GJ. What type of crown should I use? Dental Economics. www.dentaleconomics.com/science-tech/article/16386239/what-type-of-crown-should-i-use. Published February 2, 2019. Accessed July 15, 2019.
19. Poticny DJ. A new chairside zirconia for chairside manufacture. Cerecdoctors.com web site. http://cdocs-magazine.s3-website-us-east-1.amazonaws.com/2019/Q2/#{"issue_id":583360,"page":30}. Published 2019. Accessed July 24, 2019.
20. Glidewell Laboratories. BruxZir® NOW. BruxZir web site. http://bruxzir.com/bruxzir-now. Accessed July 24, 2019.
21. Kuraray Noritake Dental, Inc. KATANA™ zirconia block. Kuraray Noritake Dental Inc web site. https://kuraraydental.com/wp-content/uploads/2019/01/KATANA-Zirconia-Block-Brochure.pdf. Published January 2019. Accessed July 24, 2019.
22. 3M United States. 3M™ chairside zirconia for CEREC. 3M United States web site. https://www.3m.com/3M/en_US/company-us/all-3m-products/?N=5002385+3289969996+3293786499&rt=rud. Accessed July 24, 2019.
23. Burgess JO, Janyavula S, Lawson NC, et al. (2014). Enamel Wear Opposing Polished and Aged Zirconia. Operative Dentistry. 2014;39(2):189-194.
24. Lawson NC, Janyavula S, et al. Wear of enamel opposing zirconia and lithium disilicate after adjustment, polishing and glazing. J Dent. 2014;42(12):1586-1591.
25. Janyavula S, et al. The wear of polished and glazed zirconia against enamel. J Prosthet Dent. 2013;109(1):22-29.