You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
An influx of new and improved technology and materials is helping dentists become more efficient and effective in their practice. Technological advancements in diagnostic capabilities include digital radiography, digital cameras, and caries detection aids. Dental materials have also developed at an extraordinary rate, affecting the options dentists have for restorative materials.
Every dental office can benefit from incorporating technological aids in day-to-day practice. For example, the development of new technologies for early detection and quantitative monitoring of dental decay at an early stage of formation can provide health and economic benefits.1
A variety of innovative technologies have been developed and introduced in the last several years to aid clinicians not only in early caries detection but in making a firm diagnosis and treating cases conservatively. Furthermore, the differences in caries presentations and behavior in different anatomical sites make it unlikely that any one diagnostic modality will have adequate sensitivity and specificity of detection for all sites.2
At the same time, restorative materials have evolved and continue to evolve both functionally and esthetically. Improved esthetics are due to the gradual replacement of dental amalgam with dental composite and all-metal and porcelain-fused-to-metal indirect restorations with reinforced dental ceramics, all made possible by the rapid improvements in dental adhesive materials. The next frontier in dental restorative materials may be the evolution of bioactive materials.
These advancements in technology and material provide a plethora of options for dentists to choose from on the market. It is important that dentists understand this evolution and resulting options to select the ideal technique, technology, and materials for each dental procedure.
Modern Diagnostics
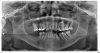
Digital radiography, since its introduction in the mid-1980s, has overtaken conventional screen-film radiography, making it one of the most significant advancements in the dental industry.3 It allows dental offices to acquire a quality image within a matter of seconds (Figure 1). It is a valuable, reliable diagnostic tool for patients of all ages. In children, for example, the primary reasons radiographs are used are for the detection of caries, dental injuries, disturbances in tooth development, and the examination of pathologic conditions other than caries.4 Additionally, 3-dimensional reconstruction of radiographic images is of importance for diagnosis and treatment planning concerning malformations, trauma, tumor investigation, and surgery planning.
Digital radiographic images can be indirect, direct, or semi-direct. Radiographic images produced by flatbed scanners with a transparency adapter, slide scanners, and digital cameras are referred to as indirect digital radiographs. Direct digital images are acquired using a solid-state sensor. Semi-direct images are obtained using a phosphor plate charge-coupling system, which transfers the number of electrons deposited in each pixel from one well to the next in a sequential manner to a readout amplifier for image display on the monitor.5
Digital radiography allows a large decrease in radiation exposure, requiring 90% less of a dose on average compared with E-speed film. Despite the advancements in digital radiography, in 2012 the American Dental Association (ADA) revised its recommendations for patient selection and limiting radiation exposure. The ADA also joined with more than 80 other healthcare organizations to promote a program called Image Gently, an initiative to "child-size" radiographic examination of children and adult patients throughout dental practices.6 Furthermore, patients themselves often request a limited exposure to radiation. Therefore, it is prudent to consider diagnostic technologies other than digital radiography.
The diagnosis of early caries lesions has been considered the cornerstone of cost-effective healthcare delivery and quality dental care.7 Cutting-edge caries detection systems are changing the way some practices screen and treat patients.8 Capable of detecting and assessing carious lesions earlier and in more locations, caries detection units include some featuring lasers that cause fluorescence of the tooth and others that employ transillumination to see through the enamel. Some are integrated into intraoral cameras, and other systems are standalone units. Advances in caries detection devices aim to overcome the limitations of traditional diagnostic methods and facilitate identification of caries at an earlier age.
Light fluorescence is commonly used in caries detecting devices. The visible light spectrum makes up the colors the human eye can see. A caries detection device that uses light fluorescence will distinguish healthy tooth from carious structures because carious tooth structure will fluoresce, whereas healthy tooth structure will not.9
The disadvantage of using fluorescence technology is that any plaque, calculus, stain, or residual prophylaxis (prophy) paste can interfere with the caries detection, causing areas to fluoresce when caries is not present. This is known as a false positive.10 To prevent false positives from occurring with fluorescence technology, a tooth must be thoroughly cleaned with either sodium bicarbonate or pumice and rinsed thoroughly.
Alternatively, some devices do not require a clear tooth surface or calibration.11 Some use near-infrared transillumination technology to detect occlusal and interproximal carious lesions in their earliest form. Infrared transillumination technology employs longer wavelengths, allowing deeper penetration into the tooth. Enamel will appear translucent, and carious lesions will appear dark. This technology incorporates non-ionizing radiation; therefore, if a patient is adamantly opposed to any radiographs, it is a good tool to use with that patient to assess their caries risk.
Digital Photography
Digital photography is an important component of dental diagnostics. It facilitates visual learning, making it one of the best tools to involve patients in their own diagnosis and care. Digital images can help motivate a patient to accept treatment by visually demonstrating what is occurring both inside the mouth and externally. Thus, both an intraoral camera and extraoral digital photography are important tools in any practice. Additionally, images can limit or reduce a dentist's liability if, for example, there is a discrepancy between what the patient remembers regarding the circumstances of pre-interventions. In such a case, the dentist and patient could each look at the images taken pre-procedure. For the majority of patients, a standard orthodontic set of photographs should be taken, including the following views: smiling, retracted anterior, left and right buccal, and occlusal of both the maxillary and mandibular arch. Thus, digital dental photography provides three main benefits: communication is significantly enhanced, trust is built, and documentation is created. There is a learning curve with digital photography and an initial investment cost. However, a variety of options are on the market, enabling an office to pick the camera that works best for it. With the right training, techniques, and equipment, dental photography can enhance diagnostic and communication capabilities.12
Restorative Technology and Materials
In addition to digital diagnostic developments, restorative technology has greatly improved. One of the earliest advancements in restorative science and technology was in adhesives. The development and regular use of adhesive materials has revolutionized many aspects of restorative and preventive dentistry. Dental adhesives are solutions of resin monomers that make resin dental substrate interaction achievable.13 A plethora of adhesives are on the market-so many that the choices may be overwhelming. When choosing an adhesive, efficacy, integrity, durability, and the reduction of sensitivity are important. The right adhesive allows conservation of tooth structure and is easy to use.
Adhesives came into existence around 1949; since then, there have been various generations of adhesives.14 With changing technologies, dental adhesives have evolved from no-etch to total-etch (4th and 5th generation) to self-etch (6th, 7th, and 8th generation) systems. Each generation has attempted to reduce the number of bottles involved in the process, minimize the number of procedural steps, provide faster application techniques, and offer improved chemistry to facilitate stronger bonding. Bonding to dental substrates is based on three different strategies: 1) etch-and-rinse, 2) self-etch, and 3) resin-modified glass-ionomer; these three differ significantly in the way in which they deal with tooth tissue.15More recently, a new family of dentin adhesives has been introduced; known as universal adhesives, these can be used either as etch-and-rinse or self-etch adhesives.16-19
A component in the majority of universal adhesives is methacryloxydecyl dihydrogen phosphate (MDP), which due to its acidic nature aids in etching and demineralization.20 This monomer also enables bonding to metal, glass, ceramic, and resin composites. In addition, to increase bond strength, components include 2-hydroxyethyl methacrylate (HEMA), dodecanediol dimethacrylate (D3MA), and bisphenol A-glycidyl methacrylate (bis-GMA), which allow the reaction between the hydrophilic tooth and hydrophobic resin restorative.20 Depending on the manufacturer, universal adhesives may also require a dual-cure activator. Some studies have shown that the application of an etching step before applying universal adhesives improves their dentine penetration but does not affect the strength of their bond to dentine after 24 hours or after thermocycling for 5,000 cycles.21 In addition, similar bond strength values have been observed for universal adhesives regardless of application mode, which makes them reliable for working under different clinical conditions.21 However, in total-etch mode, a slight increase in the strength of the bond to enamel has been observed.21
Professional preferences and differences in manufacturers' instructions regarding the selection of an adhesive strategy and the number of steps allow dentists the opportunity to select a bonding agent and technique best suited for each individual clinical treatment. A variety of restorative materials are now on the market. When choosing a restorative material, a dentist will want to consider polishability, handling properties, and bioactive properties.
The development and introduction to market of new restorative materials, especially in the past half century, has occurred at a rapid pace. For a long time, amalgam was the material of choice for dental restorations. The first dental composites were introduced in the 1950s as self-cure polymethyl methacrylate22 but did not become popular for clinical use until the early 1970s.23 The introduction of dental composite materials was then transformational, producing esthetic restorations for all intraoral applications. Composites continue to be useful on a day-to-day basis.
Bioactive restorative materials are a relatively new concept in restorative dentistry; they have evolved over the last 4 decades from being relatively specialized, highly biocompatible but low-strength dental materials to emerging over the last decade in product compositions for expanded clinical uses in restorative dentistry.24Although there are various accepted definitions, bioactive restorative materials can be explained as a bioactive material that forms a surface layer of an apatite-like material in the presence of an inorganic phosphate solution.25 A simpler definition would be a material that has a biologic effect on surrounding tissues. This could be by creating a bond, allowing remineralization, or creating a calcium precipitate to occlude margins, gaps, or pores.26
A wide range of calcium-based or calcium-containing materials have demonstrated bioactivity, such as mineral trioxide aggregate (MTA) and calcium hydroxide-containing materials (eg, various cements, pulp liners, pulp caps, root dressings). In addition to the aforementioned bioactive materials, Giomer technology is rather new to the bioactive classification of restorative materials. This new technology combines the fluoride-releasing capabilities of a glass-ionomer and the durability of a composite-resin restoration. The three main benefits of Giomer technology are fluoride release and recharge (Figure 2), decrease in acid production by creating an acid-resistant layer, and creating an anti-plaque effect. The release of fluoride is just one attribute; other ions are strontium, natrium/sodium, aluminum, silicate, and borate. Further developments to meet additional restorative clinical needs are anticipated in the newly emerging category of bioactive dental materials.
Conclusion
Modern diagnostic capabilities, digital technology, and restorative materials are all developing at a rapid pace. They are affording dentists improved materials that will provide long-lasting, esthetically appealing, and beneficial restorations-improvements in both physical and mechanical properties. They are providing technology and techniques that, when understood well, can be used to provide efficient, effective dental services and long-lasting, esthetically pleasing restorations. To enhance the delivery of personalized, precision dental care and to fill the translational gap for research findings to be incorporated into practice by general practitioners, a strong collaboration between researchers, clinicians, and educators is needed.27
About the Author
Chad C. Duplantis, DDS
Private Practice
Fort Worth, Texas
References
1. Amaechi BT. Emerging technologies for diagnosis of dental caries: the road so far. J Appl Phys. 2009;105(10):1020-1047.
2. Bader JD, Shugars DA, Bonito AJ, et al. Systematic reviews of selected dental caries diagnostic and management methods. J Dent Educ. 2001;65(1162):960-968.
3. Bansal GJ. Digital radiography. A comparison with modern conventional imaging. Postgrad Med J. 2006; 82(969):425-428.
4. Espelid I, Mejàre I, Weerheijm K; EAPD. EAPD guidelines for use of radiographs in children. Eur J Paediatr Dent. 2003;4(1):40-48.
5. Jayachandran S. Digital imaging in dentistry: a review. Contemp Clin Dent. 2017;8(2):193-194.
6. American Dental Association. Image Gently campaign expands to dentistry: urges dental professionals to use child-size radiation dose [news release]. Published September 26, 2014.
7. Verdonschot EH, Angmar-Månsson B, ten Bosch JJ, et al. Developments in caries diagnosis and their relationship to treatment decisions and quality of care. ORCA Saturday Afternoon Symposium 1997. Caries Res. 1999;33(1):32-40.
8. Levato CM. Intraoral digital radiology: a safe, cost-efficient imaging solution. Compend Contin Educ Dent. 2011; 32(spec no 4):48-50.
9. Graye M, Markowitz K, Strickland M, et al. In vitro evaluation of the Spectra early caries detection system. J Clin Dent. 2012;23(1):1-6.
10. Diniz MB, Rodrigues JA, Lussi A. Traditional and novel caries detection methods. In: Contemporary Approach to Dental Caries. Rijeka, Croatia: Intech; 2012.
11. Karlsson L. Caries detection methods based on changes in optical properties between healthy and carious tissue. Int J Dent. 2010;2010:270729. doi: 10.1155/2010/270729.
12. McLaren EA, Garber DA, Figueira J. The Photoshop Smile Design technique (part 1): digital dental photography. Compend Contin Educ Dent. 2013;34(10):772-776.
13. Perdigão J. New developments in dental adhesion. Dent Clin North Am. 2007;51(2):333-357.
14. Söderholm KJ. Dental adhesives… how it all started and later evolved. J Adhes Dent. 2007;9(suppl 2):227-230.
15. De Munck J, Van Landuyt K, Peumans M, et al. A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res. 2005;84(2):118-132.
16. Sofan E, Sofan A, Palaia G, et al. Classification review of dental adhesive systems: from the IV generation to the universal type. Ann Stomatol (Roma). 2017;8(1):1-17.
17. Hanabusa M, Mine A, Kuboki T, et al. Bonding effectiveness of a new "multi-mode" adhesive to enamel and dentine. J Dent. 2012;40(6):475-484.
18. Perdigão J, Sezinando A, Monteiro PC. Laboratory bonding ability of a multi-purpose dentin adhesive. Amer J Dent. 2012;25(3):153-158.
19. Muñoz MA, Luque I, Hass V, et al. Immediate bonding properties of universal adhesives to dentine. J Dent. 2013; 41(5):404-411.
20. Alex G. Universal adhesives: the next evolution in adhesive dentistry? Compend Contin Educ Dent. 2015;36(1):15-26.
21. Wagner A, Wendler M, Petschelt A, et al. Bonding performance of universal adhesives in different etching modes. J Dent. 2014;42(7):800-807.
22. Bayne SC, Ferracane JL, Marshall GW, et al. The evolution of dental materials over the past century: silver and gold to tooth color and beyond. J Dent Res. 2019;98(3):257-265.
23. Rupp NW. Clinical placement and performance of composite resin restorations. J Dent Res. 1979;58(5):1551-1557.
24. Jefferies SR. Bioactive and biomimetic restorative materials: a comprehensive review. Part I. J Esthet Restor Dent. 2014;26(1):14-26.
25. Kokubo T, Kushitani H, Sakka S, et al. Solutions able to reproduce in vivo surface-structure changes in bioactive glass-ceramic A-W. J Biomed Mater Res. 1990; 24(6):721-734.
26.Lawson N. Examining bioactive restorative materials: what the evidence says about their clinical application in restorative dentistry. Decisions in Dentistry. 2018;4(4):24-27.
27. Dragan IF, Dalessandri D, Johnson LA, et al. Impact of scientific and technological advances. Eur J Dent Ed. 2018;22(suppl 1):17-20.