You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Oropharyngeal cancers (OPSCC) are a subset of head and neck squamous cell carcinomas (HNSCC); the sixth most common cancer globally with an incidence of 45,000 annually in the United States.1 Head and neck squamous cell carcinomas have been traditionally associated with tobacco and alcohol exposure. However, surveillance data show that as tobacco use has declined, so has the incidence of tobacco- associated HNSCC.2 Concurrently, there has been an increase in the incidence of HNSCC in oropharyngeal sites including the base of the tongue, soft palate, uvula, palatine tonsil fossa, and oropharynx.2-4 In particular, the incidence of oropharyngeal cancer is occurring disproportionately in white, non-smoking males, of moderate to upper income, between the ages of 35-55.5 This epidemiological difference has been attributed to the human papilloma virus (HPV), a sexually transmitted infection (STI), particularly HPV-16, which accounts for 90% of HPV-positive oropharyngeal squamous cell carcinomas (OPSCC).1 The prevalence of HPV-positive OPSCC in the United States has increased more than 300% in the past 30 years and is estimated to surpass the numbers of HPV-related cervical cancers by 20201 as well as being predicted to become the most common cancer of the upper aerodigestive tract.1
Three U. S. Food and Drug Administration (FDA)-approved HPV vaccinations have been found to be safe and effective against the oncogenic and non-oncogenic types of HPV associated with genital warts and cervical and other anogenital cancers.6 Although there is a lack of direct evidence supporting the efficacy of the vaccine in the prevention of oropharyngeal cancers, it is predicted that vaccination against HPV-16 prior to an initial infection can prevent HPV-positive OPSCC.5 The Advisory Committee on Immunization Practices (ACIP) has been recommending routine HPV vaccination for girls between the ages of 9 and 26 since 2006. However, it wasn't until 2011 that the vaccine was recommended for boys, who are also most at risk for HPV-positive OPSCC. In 2016, the ACIP, FDA, and Centers for Disease Control and Prevention (CDC) released a recommendation for a two-dose schedule of a 9-valent HPV vaccine (Gardasil®9, Merck & Co, Inc.) for both boys and girls, ages 9-14, aiming to increase compliance.7 Individuals being vaccinated between the ages of 15-26 require three doses of the vaccine.
Recent CDC statistics show that while 60% of adolescents aged 13-17 have received at least one dose of the vaccine, only 43% are up to date on all recommended doses.8 Vaccination uptake is still far below the Healthy People 2020 goal of 80% for both males and females.9 In examining the slow uptake of the vaccine, a number of factors have been identified including a lack of awareness and knowledge of HPV, misconceptions regarding the susceptibility to and implications of HPV infections, unawareness regarding the availability, safety, efficacy and cost of the vaccine, and lack of perceived risk factors.10,11 However, research has repeatedly shown that the most compelling positive influence on increasing vaccination uptake is provider recommendation.12-14
Patients have been shown to trust and follow their healthcare providers' advice when given decisively.15 Dorell et al study of 8,652 adolescents and their parents in the United States found that over three-fourths of parents (78%) reported that their healthcare providers played a role in their child's vaccine uptake.15 These findings were supported in subsequent studies by Small et al and Moss et al.11,16 Despite support from these studies, many healthcare providers are hesitant to make strong recommendations regarding the HPV vaccination. Many providers are reluctant to discuss sexual activity with their patients.17 Other providers stratify patients into perceived risk categories, discussing and recommending vaccination for HPV only for persons perceived to be high risk,18 creating an ethical challenge in terms of beneficence towards all patients.
Dental professionals are also reluctant to discuss HPV with their patients. At the core is the dilemma of communicating with patients about the risk factors and oral manifestations of a STI.19 Some dentists perceive it is their professional and ethical responsibility to include discussing the HPV-oropharyngeal cancer link, while others believe any discussion involving sensitive topics, such as STIs, should be entrusted to medical professionals.19,20 Daley et al found that dentists and dental hygienists believed HPV discussions were inappropriate in the dental setting due to confidentiality issues, especially in open-designed clinics.20 Additionally, some male practitioners worried that discussions about sexual practices would put them at risk for sexual harassment accusations. Dental professionals also report a lack of confidence in their knowledge of oral HPV infections, including HPV+ OPSCC, and the HPV vaccination, resulting in an avoidance of the topic completely.19,20,21 Finally, the lack of standard of care guidelines, by professional organizations, has been cited as a barrier to communicating about HPV.20,21 The overall result has been a lack of clearly defined roles with many dental professionals taking a "wait and see" attitude.20,21
Dental professionals are well positioned to influence HPV vaccination uptake.11 According to the CDC, 85% of children ages 2-17 had at least one visit to the dentist during 2015, presenting an opportunity to advocate for the HPV vaccine.22 The purpose of this study was to ascertain the knowledge, attitudes, and practices of Minnesota dentists and dental hygienists regarding HPV+ OPSCC and HPV vaccination.
Methods
This study received an exempt status from the University of Minnesota Institutional Review Board (IRB). A mailing list consisting of a randomized sample of the 4015 dentists and 5688 dental hygienists holding a current Minnesota license was purchased by the principle investigator (PI) from the Department of Administration. The sample size was determined based on a 5% margin of error, for a study sample size of 369 out of approximately 9600 professionals. Assuming a response rate of approximately 25%, 1500 paper questionnaires (750 dentists and 750 dental hygienists) were mailed to the target population.
No validated instrument specifically designed to assess the attitudes of dental professionals toward HPV and HPV vaccination was found in the literature; therefore, a survey instrument originally targeted to head and neck surgeons was selected for use.23 Questions were modified with profession-specific vocabulary, as needed. The survey was pilot tested with dental and dental hygiene faculty members and revisions were made based on their feedback. The 32-item paper questionnaire was formatted into five sections: demographics, current practices, knowledge of HPV+ OPSCC and the HPV vaccine, attitudes toward vaccination advocacy, and awareness efforts. A cover letter and information sheet explaining the purpose of the survey, how the respondents' information was obtained, the voluntary and confidential nature of the survey, and contact information for the PI along with the University of Minnesota IRB were attached to the questionnaire and mailed to the sample population. Survey participation was confidential; no personal identifiers were obtained. Questionnaires were coded for tracking purposes to ensure only non-responders received a second mailing sent one month after the initial mailing.
Descriptive statistics were used to summarize the data. Two group t-tests or analysis of variance (ANOVA) was used to compare mean knowledge and attitude scores between question responses. If the overall test for ANOVA was statistically significant, Tukey adjusted pairwise comparisons were performed. A Pearson correlation coefficient was calculated between the knowledge and attitude scores. P-values less than 0.05 were considered statistically significant. SAS V9.3 (SAS Institute Inc.; Cary, NC) was used for the analysis.
Results
A total of 111 dentists and 207 dental hygienists (n=318) returned completed surveys for an overall response rate of 21%. Over two-thirds (67%) identified as female and 33% identified as male, with a non-response rate of .94%. A majority of the respondents (82%) worked in private practices, while the others were practicing in academic institutions (6%), public health settings (6%), and managed care practices (1%). Non-responses to questions were unweighted. Demographic information, including profession, age, gender, practice type, and year of graduation from professional school, is presented in Table I.
Current Practices
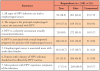
While the majority of respondents (92%) perform oral cancer screenings, only 44% discuss risk factors for oropharyngeal cancer, with even fewer (21%) discussing HPV as a risk factor. Only 9% of respondents discuss the HPV vaccination for persons (both male and female) between ages 11 and 26. Respondents were asked to select the two most important factors for not discussing vaccination. The most common factors include not remembering (41%), not feeling qualified (35%), and the belief that discussing the vaccine is not within their role as a healthcare professional (22%). There were no statistically significant differences between demographics and current practices (p>0.05). Responses rates are shown in Table II.
Knowledge
The mean knowledge score was 61%; differences between profession, practice type, or gender were not statistically significant. Overall, mean knowledge scores differed between graduation years (p=0.0079). In pairwise comparisons, mean knowledge scores for graduations years in the 1960s was lower when compared to the 1980s (p=0.18), 1990s (p=0.044), 2000s (p=0.018), and 2010s (p=0.006). Analysis of variance (ANOVA) or two group t-tests or were used to compare mean knowledge between genders, professions, graduation years, and practice types. Tukey adjusted pairwise comparisons were performed when the overall test for ANOVA was statistically significant. Knowledge question response rates are displayed in Table III.
Attitudes
Slightly more than half (57%) of respondents strongly agree or somewhat agree that medical professionals should remain the sole appropriate source of information regarding the HPV vaccine. A majority also strongly agree or somewhat agreed (66%) that they were uncomfortable in discussing HPV with their patients and/or their parents, however 82% disagreed with the statement, "Discussing the HPV vaccination is not appropriate in my practice because it cannot help my patients." Over half (57%) of respondents believed that it is necessary to discuss issues relating to sexuality before recommending the HPV vaccination. Over two-thirds (70%) of respondents disagreed with the statement stating that the safety of the HPV vaccination has not been established while 67% disagreed with the statement that since the efficacy of the vaccine has not been established for oropharyngeal cancer, it is inappropriate to discuss vaccination with their patients (Table IV).
Attitude scores were analyzed by demographic characteristics. Mean attitude scores did not differ for gender, (p=0.0619), graduation year (p=0.0716), or practice type (p=0.1650). However, mean attitude scores were higher for dentists when compared to dental hygienists (p=0.0021). Mean attitude scores by demographics are shown in Table V. Overall, there was a statistically significant difference between questions (p<.0001). Question 2.7 had the highest mean and question 2.4 had the smallest mean. In pairwise comparisons (Tukey adjusted for multiple comparisons), all pairwise comparisons were significant (p<0.05) except 2.1 vs 2.4 (p=0.1335) and 2.5 vs 2.6 (p=0.9917). Pairwise comparisons of scores by attitude statement are shown in Table VI.
Future Awareness Efforts
Respondents were overwhelmingly in favor of efforts by dental professional organizations to raise awareness of HPV+ OPSCC and HPV vaccination. This included supporting efforts by professional organizations in educating dental professionals regarding advocacy for HPV vaccination (80%), raising public awareness of the relationship between HPV infection and oropharyngeal cancer (76%), HPV vaccination (70%), patient education by dental professionals (75%), and distributing printed material on HPV infection (90%). Respondents also indicated they would follow HPV vaccination advocacy guidelines issued by dental professional organizations. The majority of respondents (90%) reported they would use printed information on HPV+ OPSCC to educate patients if the materials were made available through professional organizations. When asked whether or not dentists in Minnesota should be licensed to administer the HPV vaccine, the majority of respondents were either opposed (33%) or unsure (40%). Those who were opposed or unsure had a lower mean attitude score when compared to those who were in favor (p<.0001 and p=0.0163, respectively). Respondents' beliefs toward future efforts to raise awareness of HPV related cancers and HPV vaccination are shown in Table VII.
Discussion
HPV is thought to be responsible for 70% of OPSCC cases,24 a 300% increase from the 1980s, and the most recent statistics reported by the CDC show that HPV oropharyngeal cancer is now the most common HPV-associated cancer.25 Despite the increased prevalence of HPV+ OPSCC, several studies have shown that few dentists or dental hygienists discuss HPV infection as a risk factor for OPSCC.19,20,21 The majority (92%) of the Minnesota dentists and dental hygienists in this study reported practicing secondary cancer prevention practices through visual and tactile examinations or oral cancer screenings, however only 21% discussed HPV as a risk factor, consistent with other studies.19,20,21 While considered the standard of care by both the American Dental Association and the American Dental Hygienists' Association, there is limited evidence that oral cancer screenings reduce the incidence of morbidity.26,27 Early detection can be difficult, particularly for HPV+ OPSCC, which develop in areas of the oral cavity that are difficult to visualize, even with the use of adjunctive screening tools.26,27 Additionally, no precursor lesion exists for HPV+ OPSCC as in cervical cancer.
The opportunity exists for a primary prevention activity for HPV+ OPSCC in vaccine advocacy. While the efficacy of HPV vaccines in prevention of oral HPV is unknown, it is well known that the vaccines are effective against HPV-16, which is implicated in 90% of HPV+ OPSCC. With the increase in HPV+ OPSCC, it can be argued that dental providers have a professional and ethical obligation to discuss HPV infections with patients and promote the vaccine for eligible patients.4,20 Only 9% of the respondents in this study discussed the vaccine with their patients. Barriers to HPV communication and vaccine advocacy within the Minnesota dental community were identified. The most common reasons cited included forgetting to discuss the vaccine (41%), not feeling qualified (35%), denying vaccine advocacy as within their professional role (22%), and not wanting to discuss how HPV is transmitted (13%). Further, 66% of respondents reported feeling discomfort in HPV discussions with patients and/or parents. Barriers identified in this study support the findings of other researchers that identified practitioners expressing discomfort in discussing sexual behaviors with patients, perceiving such discussions as not within a dental professional's role, and a lack of knowledge of the HPV disease process and vaccination.20,28-30 An overwhelming majority of respondents in this study indicated an interest in increased educational and policy support for HPV awareness and vaccine advocacy by professional organizations, presenting an educational opportunity for academic institutions, foundations, and professional organizations.
In response to the increased incidence of HPV+ OPSCC, the American Dental Association and the American Academy of Pediatric Dentistry have been encouraging dental providers to discuss the connection between HPV and OPSCC.4,30 In addition, recently, the number articles related to HPV+ OPSCC in dental journals and continuing education courses has increased, signaling the important role oral health professionals play in HPV+ OPSCC.4,30 Dental hygienists are well trained in prevention counseling activities, such as tobacco cessation, diabetes prevention, and motivational interviewing.28 These skills can be easily transferred to HPV prevention and risk factor management activities.28 Just as tobacco cessation efforts focus on the prevention of cancer, HPV discussions can be presented within the framework of cancer prevention. Adjusting the attitude of dental providers toward HPV may serve to improve the practice of HPV prevention in the dental setting. By framing HPV as cancer-causing virus rather than a STI, dental professionals may be more comfortable and inclined to developing protocols regarding HPV including communication scripting and referrals to other healthcare providers.
Re-framing the conversation to cancer prevention has the potential to change at-risk behaviors and increase HPV vaccine uptake.4 With the increasing public awareness of HPV and its association with OPSCC, patients will expect their dental providers to not only be knowledgeable on the topic but to also initiate conversations on risk factors and prevention.20 The recommended HPV vaccine's two dose schedule, administered between 6 to 12 months apart, is concurrent with the American Academy of Pediatric Dentistry's periodicity of examination guidelines for children and adolescents.31,32 This provides an opportunity for oral health professionals to collaborate in the prevention of HPV+ cancers through reinforcement of health promotion and disease prevention messages promulgated by other healthcare providers.33 Parental attitudes toward vaccination also influences vaccine uptake.34 Underwood et al reported that parents who received information on HPV vaccination from three or more sources have a more positive attitude when compared to parents who receive information from less than three sources.34 It has also been found that educational materials alone do not increase vaccine uptake. However, when education is received through trusted sources, such as healthcare professionals, uptake increases.11,34
Furthermore, to increase vaccine uptake, innovative approaches to vaccine delivery are currently being discussed. McRee et al found adolescent boys and their parents were amenable to alternative settings other than the traditional medical setting for receiving the HPV vaccine.35 Minnesota State Statute currently allows trained dentists to administer the influenza vaccine.36 A similar opportunity exists to petition the Minnesota State Board of Dentistry to support administration of the HPV vaccine by dentists during adolescent preventive dental visits, potentially increasing vaccine uptake. However, in a recent study investigating parental attitudes toward HPV vaccination in the dental setting, parents expressed low comfort levels in regards having a dentist vaccinate their children.37 Lack of trust in a dentist's role as vaccinator and the staff's ability to manage adverse events were cited as the primary reasons,36 highlighting the need for better patient education in regards to dentists' training.
Limitations of this study include the small sample size and low response rate. The sample size was limited to 750 dentists and 750 dental hygienists from candidate pools of 4,015 dentists and 5,688 dental hygienists for an overall response rate of 21%. Paper surveys were mailed to the sample population and were limited to the random sample of 1,500 for financial reasons. Results of this survey are limited to dental professionals licensed in Minnesota. Additionally, the survey used was not validated.
Future research should investigate providing HPV vaccines in the dental setting. Researchers have used the health literacy framework to gather baseline data to inform the development of health literacy interventions for dental hygienists and dentists.30 Further study is needed to investigate effective strategies and tools for HPV communication in the dental setting; perhaps using the health literacy framework or other health communication theories. Collaboration with other healthcare providers may also increase HPV vaccine uptake. A number of sources including the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) provide HPV communication tools that can be adapted to the dental setting.38,39
Conclusion
Research shows that HPV vaccine uptake can be improved when there is a stronger provider recommendation. Advocacy of the HPV vaccine by dental providers may prompt an increase in vaccine uptake among adolescents. However, there are barriers including lack of knowledge about HPV and HPV vaccination, discomfort in discussing HPV infection with patients, and denying that vaccine advocacy is within their professional role that prevent most dental providers from discussing HPV with patients. Findings in this study suggest dentists and dental hygienists would support the promotional efforts of their professional associations to increase public awareness of HPV+ OPSCC and HPV vaccine advocacy. Dental providers are looking to their professional associations for leadership, direction, and training in HPV patient communication. These findings highlight an opportunity for schools and professional associations to better educate dental providers in HPV communication and vaccine advocacy as it relates to cancer prevention.
About the Authors
Cynthia L. Stull, RDH, MDH is a clinical assistant professor in the Department of Primary Care, Division of Dental Hygiene in the University of Minnesota School of Dentistry; Scott Lunos, MS is a biostatistician in the Biostatistical Design and Analysis Center, Clinical and Translational Science Institute; both at the University of Minnesota, Minneapolis, MN
Corresponding Author: Cynthia L. Stull, RDH, MDH; stul0045@umn.edu
References
1. Smith TJ, Mendez A, Donald C, Nagel TH. HPV-associated oropharyngeal squamous cell carcinoma. JAAPA. 2017 Jan;30(1):14-9.
2. D'Souza G, Dempsey A. The role of HPV in head and neck cancer and review of the HPV vaccine. Prev Med. 2011 Oct;53(Suppl 1):1-16.
3. Javadi P, Sharma A, Zahnd WE, Jenkins WD. Evolving disparities in the epidemiology of oral cavity and oropharyngeal cancers. Cancer Causes Control. 2017 Jun;28(6):635-45.
4. Minassian M, Fried JL, Ord RA. HPV-positive head and neck cancers: a review of the literature. J Dent Hyg. 2014 Aug;88(4):194-201.
5. Pytynia KB, Dahlstrom KR, Sturgis EM. Epidemiology of HPV-associated oropharyngeal cancer. Oral Oncol. 2014 May;50(5):380-6.
6. Chattopadhyay A, Weatherspoon D, Pinto A. Human papillomavirus and oral cancer: a primer for dental public health professionals. Community Dent Health. 2015 Jun;32:117-28.
7. Centers for Disease Control and Prevention. Vaccines and preventable diseases [Internet]. Atlanta: Centers for Disease Control and Prevention; 2016 [cited 2018 Mar 1]. Available from: https://www.cdc.gov/vaccines/vpd/hpv/hcp/administration.html
8. Centers for Disease Control and Prevention. Vaccines and preventable diseases: HPV vaccination coverage data [Internet]. Atlanta: Centers for Disease Control and Prevention; 2017 [cited 2018 Mar 1]. Available from: https://www.cdc.gov/hpv/hcp/vacc-coverage.html
9. U.S. Department of Health and Human Services. Healthy people 2020: immunization and infectious diseases [Internet]. Washington, DC: U.S. Department of Health and Human Services; 2014 [updated 2018 Mar 13; cited 2018 Mar 1]. Available from: https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives
10. Healy CM, Montesinos DP, Middleman AB. Parent and provider perspectives on immunization: are providers overestimating parental concerns? Vaccine. 2014 Jan;32:579-84.
11. Small SL, Sampselle CM, Martyn KK, Dempsey AF. Modifiable influences on female HPV vaccine uptake at the clinic encounter level: a literature review. J Am Assoc Nurse Pract. 2014 Sep;26(9):519-25.
12. Allen JD, Othus MKD, Shelton RC, et al. Parental decision making about the HPV vaccine. Cancer Epidemiol Biomarkers Prev. 2010 Sep;19(9):2187-98.
13. McRee AL, Gilkey MB, Dempsey AF. HPV vaccine hesitancy: findings from a statewide survey of healthcare providers. J Pediatr Heal Care. 2014 Nov;28(6):541-9.
14. Moss JL, Gilkey MB, Rimer BK, Brewer NT. Disparities in collaborative patient-provider communication about human papillomavirus (HPV) vaccination. Hum Vaccin Immunother. 2016 Jun;12(6):1476-83.
15. Dorell C, Yankey D, Kennedy A, Stokley S. Factors that influence parental vaccination decisions for adolescents, 13 to 17 years old: national Immunization survey-teen, 2010. Clin Pediatr (Phila). 2013 Feb;52(2):162-70.
16. Moss JL, Reiter PL, Rimer BK, Brewer NT. Collaborative patient-provider communication and uptake of adolescent vaccines. Soc Sci Med. 2016 Jun;159:100-7.
17. Gilkey MB, McRee AL. Provider communication about HPV vaccination: A systematic review. Hum Vaccin Immunother. 2016 Jun;12(6):1454-68.
18. Gilkey MB, Malo TL, Shah PD, et al. Quality of physician communication about human papillomavirus vaccine: findings from a national survey. Cancer Epidemiol Biomarkers Prev. 2015 Nov;24(11):1673-9.
19. Northridge ME, Manji N, Piamonte RT, et al. HPV, oropharyngeal cancer, and the role of the dentist: a professional ethical approach. J Health Care Poor Underserved. 2012 Nov;23(4 Suppl):47-57.
20. Daley E, Debate R, Dodd V, et al. Exploring awareness, attitudes, and perceived role among oral health providers regarding HPV-related oral cancers. J Public Health Dent. 2011 Spring;71(2):136-42.
21. Daley EM, Thompson EL, Vamos CA, et al. HPV-related knowledge among dentists and dental hygienists. J Cancer Educ. 2018 Aug;1-6.
22. Centers for Disease Control and Prevention. Oral and dental health [Internet]. Atlanta; Centers for Disease Control and Prevention; 2017 [cited 2018 Mar 1]. Available from: https://www.cdc.gov/nchs/fastats/dental.htm
23. Malloy KM, Ellender SM, Goldenberg D, Dolan RW. A survey of current practices, attitudes, and knowledge regarding human papillomavirus-related cancers and vaccines among head and neck surgeons. JAMA Otolaryngol Head Neck Surg. 2013;139(10):1037-42.
24. Centers for Disease Control and Prevention. Cancers associated with human papillomavirus, United States 2011-2015. Atlanta (GA): Centers for Disease Control and Prevention (US); 2018 Aug. 2 p. USCS data brief, No. 4
25. Chaturvedi AK, Engels EA, Pfeiffer RM, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011 Nov;29(32):4294-301.
26. Cleveland JL, Junger ML, Saraiya M, et al. The connection between human papillomavirus and oropharyngeal squamous cell carcinomas in the United States. J Am Dent Assoc. 2011 Aug;142(8):915-24.
27. Rethman MP, Carpenter W, Cohen EEW, et al. Evidence-based clinical recommendations regarding screening for oral squamous cell carcinomas. J Am Dent Assoc. 2010 May;141(5):509-20.
28. Daley E, Dodd V, DeBate R, et al. Prevention of HPV-related oral cancer: assessing dentists' readiness. Public Health. 2014 Mar;128(3):231-8.
29. Thompson EL, Daley EM, Vamos CA, et al. Health literacy approaches to improving communication between dental Hygienists and patients for HPV-related oral cancer prevention. J Dent Hyg. 2017 Aug;91(4):37-45.
30. Vázquez-Otero C, Vamos CA, Thompson EL, et al. Assessing dentists' human papillomavirus-related health literacy for oropharyngeal cancer prevention. J Am Dent Assoc. 2018 Jan;149(1):9-17.
31. Centers for Disease Control and Prevention. HPV vaccine recommendations [Internet]. Atlanta; Centers for Disease Control and Prevention; 2016 [cited 2018 Mar 1]. Available from: https://www.cdc.gov/vaccines/vpd/hpv/hcp/recommendations.html
32. American Academy of Pediatric Dentistry. Periodicity of examination, preventive dental services, anticipatory guidance/counseling, and oral treatment for infants, children, and adolescents [Internet]. Chicago: American Academy of Pediatric Dentistry; ©2002 - 2018 [cited 2018 Mar 1]. Available from: http://www.aapd.org/media/Policies_Guidelines/BP_Periodicity.pdf
33. Kaste LM, Wilder JR, Halpern LR. Emerging topics for dentists as primary care providers. Dent Clin North Am. 2013 Apr;57(2):371-6.
34. Underwood NL, Gargano LM, Jacobs S, et al. Influence of sources of information and parental attitudes on human papillomavirus vaccine uptake among adolescents. J Pediatr Adolesc Gynecol. 2016 Dec;29(6):617-22.
35. McRee AL, Reiter PL, Pepper JK, Brewer NT. Correlates of comfort with alternative settings for HPV vaccine delivery. Hum Vaccin Immunother. 2013 Feb;9(2):306-13.
36. Minnesota legislature. 2018 Minnesota statutes: administration of influenza vaccinations [Internet]. St Paul; Revisor of statutes, State of Minnesota; 2018 [cited 2018 Mar 1]. Available from: https://www.revisor.mn.gov/statutes/?id=150A.055
37. Lazalde GE, Gilkey MB, Kornides ML, McRee AL. Parent perceptions of dentists' role in HPV vaccination. Vaccine. 2018 Jan;36:461-6.
38. Centers for Disease Control and Prevention. Vaccines and preventable diseases [Internet]. Atlanta (GA): Centers for Disease Control and Prevention; 2017 [cited 2018 Mar 1]. Available from: https://www.cdc.gov/hpv/hcp/index.html
39. World Health Organization. HPV vaccine communication [Internet]. Geneva; 2016 [cited 2018 Mar 1]. Available from: http://www.who.int/immunization/documents/WHO_IVB_16.02/en/