You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Five Underused Dental Codes That Dentists Should Consider
Adam Burr, DDS
Proper coding is essential for a successful dental practice. Dentists should learn to use dental procedures and nomenclature (CDT) codes that enhance their ability to discuss treatment options with patients rather than limiting treatment due to certain procedures not being covered by insurance or patient financial constraints. Most dentists struggle with treating extensive cases when the patient has an average income. When presented with a comprehensive treatment plan, many patients will ask what is covered by insurance. This may greatly affect their decision to accept treatment. It is important to: a) advocate for patients to ensure that they receive the best dental care possible; b) consider their financial health so that they are more likely to accept proposed treatments; and c) offer a properly phased treatment plan that facilitates a realistic timeline for this type of care. Five dental codes that many dentists may not currently use may aid patients in paying for care and also increase the chance that a patient will accept a dentist's recommended treatment plan, especially in the case of same-day dentistry.
The Patient Conversation to Facilitate Case Acceptance
The dentist should take part in a pre-examination interview with every patient who visits the practice. This interview provides an opportunity to discuss the patient's expectations, questions, and concerns without undue obligation. The interview also allows the dentist to inform the patient that time is available to start treatment if needed. This preemptively increases the likelihood of patient case acceptance.1 It is important to set this pre-examination interview apart from the post-examination discussion.
Patient Case Example
A male patient entered the author's practice complaining of tooth pain, saying he had been suppressing that pain because of limited income. He was married with two young children, worked an average-income job in construction, and had an average dental insurance plan. He had not visited a dentist for several years because he did not have insurance at the time and the cost seemed prohibitive.
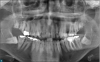
During the pre-examination interview, the patient complained about pain and said he was aware of cavities. He knew his mouth needed attention, but he noted financial concerns. Although he wanted to fix any potential condition, his main concern was maintaining a nice smile. Panoramic x-rays showed some challenges in this case due to the limitations set forth by the patient (Figure 1). He had multiple unsalvageable teeth, generalized periodontal disease, one stainless-steel crown and fillings that were failing, rampant initial and recurrent decay, and impacted third molars.
It was possible to simply use the entire insurance benefit and budget in this case by extracting the hopeless teeth and proceeding with final restorations on one or two teeth that were bothering the patient, but that would have left rampant decay and periodontal disease untreated. That approach could have hindered the patient from coming back. Instead, it was important to make more progress in this challenging case, focusing on the broader scenario of overall health rather than fixing only one or two immediate concerns. An extended approach would also help increase case acceptance because the patient would see tangible progress throughout treatment.2
Challenges and the Post-Examination Discussion
The first challenge was a limited budget. The patient's desire for a nice smile at a low price was not realistic, and his home care habits may have complicated the treatment.
Having completed x-rays and the initial examination, the author was now prepared for a post-examination discussion. At this point, the dentist should come to an agreement with the patient about the level of necessary treatment and acknowledge that his finances are a concern. The dentist should ask how much the patient can invest outside of the available insurance benefit. The different payment arrangements available in the practice should be discussed to make treatment possible; the patient should be introduced to the financial coordinator or specialist to go over the details. This conversation will make it easier to discuss the treatment possibilities within budget.
In this case, the patient said he could afford $2,000 out of pocket. This discussion took place in November; his insurance plan offered $1,500 per calendar year. Between 2 years of treatment starting in November and picking up again early the following year, along with $2,000 out of pocket, the total available for treatment was $5,000.
Based on the treatment plan, the patient could not be restored completely for $5,000, but he could become disease-free, and further treatment would be possible in future years. It is important to set expectations about the amount of time needed to fully restore all teeth and explain that there will be further treatment after the initial phase. In this case, the initial treatment phase focused on pain relief and disease management.
Pulpal Debridement
Code 3221, or pulpal debridement, is used for relief of acute pain before a conventional root canal. This code cannot be used on the same day as final endodontic treatment.3 For the patient in this case, this code was used on teeth Nos. 6, 7, and 30. Using a rubber dam, the author accessed the pulp chamber and removed all inflamed and otherwise accessible nerve tissue. Some practitioners may choose to irrigate if necessary and place calcium hydroxide in the canals and pulp chamber. Next, filling the accesses took place with an interim restorative material. This procedure can be completed in 10 to 15 minutes.
Aside from the extraction of hopeless teeth, performing the pulpal debridements allowed the patient to initiate curative treatment while planning for the remaining phases of disease control. Most insurance carriers will typically cover the pulpal debridement as long as it is not done on the same day as definitive root canal therapy.
Interim Caries-Arresting Medicaments
The next underused code is 1354, for interim caries-arresting medicaments. These are intended to arrest or stop decay from progressing. The main product used in this case was silver diamine fluoride (SDF). This is not the only medicament that can be used with this code.4 SDF will stop the gross decay but will also stain the tooth a dark silver or brown color, which the patient should be informed of before this procedure is performed. It will not eliminate the need for pulpal or endodontic therapy, but it may allow the patient time to plan for the definitive treatment.
This code can be used simultaneously with code 3221 and should be reported by the tooth treated, not by the number of lesions.4 Together these codes can be used for treatment of the patient's immediate pain. In most states code 1354 can be performed by auxiliary personnel. The cost to deliver these treatments is low, thereby allowing a reasonable fee to be charged while simultaneously being attainable for most average-income patients.
Protective Restorations
The third underused code is 2940, for protective restorations. Most dentists do not realize that they can place a protective restoration and receive compensation for it. Protective restoration protects the tooth structure from further deterioration and promotes healing. This code should not be used for typical endodontic access closure and is not the base or buildup for the definitive restoration.5 There are no limitations on the type of material that may be used. In the author's case, a reinforced glass-ionomer was used. It is important to highlight the temporary nature of this treatment because additional final restorative treatment will be needed in the future.
In the patient case, using these three codes conjointly relieved pain, improved function and esthetics, and showed the patient that his expectations were possible. There were several teeth for which all three codes were used. Most importantly, the patient saw solid progress. This visual progress often makes a patient excited to complete additional treatment to further improve the function and esthetics of his or her smile.
Provisional Crowns
Another underused code is 2799, for provisional crowns. The author's patient had recurrent decay under a stainless-steel crown. Although this tooth was not a priority in the treatment plan, it would be financially devastating to emergently retreat a root canal while still in the disease control phases of his treatment. This code can be more complicated than the others in that it does require a documented, future diagnosis be performed prior to definitive treatment. Generally, there is no limitation on what material constitutes a provisional crown. Therefore, it is acceptable to use any material with the ability to withstand the function for as long as needed. CAD/CAM restorations can be used. Dental auxiliaries can do much of the work in designing and seating these temporary restorations. Most CAD/CAM suppliers have inexpensive materials that can be used for this application. Similar to the first three codes, 2799 can be used with the others on the same tooth, although it is the author's opinion that 2799 and 2940 should not be used simultaneously on the same tooth.6
Other Drugs or Medicaments
The final code is 9630, for other drugs or medicaments, which include oral antibiotics, oral analgesics, and topical fluoride.7 Proper maintenance and follow-up are essential to the success of any extensive treatment plan and patient progress. The patient was diagnosed with a high caries risk, which warranted a risk-reduction protocol, including prescription-strength fluoride toothpaste. Other options that fit within this category include remineralizing dental creams, or calcium phosphopeptide amorphous calcium phosphate (CPP-ACP), fluoride, and chlorhexidine varnishes applied more frequently in the dental office. Daily xylitol use and more SDF interim caries-arresting medicament applications are also possible. A cost is associated with these products, and proper instruction and demonstration of their use is needed.
The patient was charged a reasonable fee for that service; most insurance companies will not reimburse for this code, but it easily fit into his budget.
Case Summary
As shown in Table 1, the patient had $5,000 to spend, including insurance, on an extensive and challenging treatment plan. After the initial examination and x-rays, the author extracted eight teeth and completed scaling and root planing in all four quadrants. The patient's decay and periodontal disease were treated; the large, carious lesions on his anterior teeth were filled with protective restorations; several periodontal maintenance appointments were needed; and all five codes were used to move his treatment forward. The patient's total out-of-pocket cost was $1,948, with an insurance contribution of $2,924.
Through the use of these lesser-known CDT codes, the patient became satisfied with his treatment and more confident in his smile while staying within his budget. He has since returned for phased, definitive treatment because his financial needs were taken into consideration and his expectations were reasonably managed while tangible progress was made with his dental health.
About the Author
Adam Burr, DDS
Private Practices
Salt Lake City, Utah
References
1. Palmer J. Pre-consultation interview. Case Acceptance Academy. https://www.caseacceptanceacademy.com/your-dental-office-pre-consultation-interview/. Published November 7, 2016. Accessed August 15, 2018.
2. Cranham J. Increasing case acceptance with mindset shift. The Dawson Academy. http://dental.thedawsonacademy.com/increasing-case-acceptance. Published May 31, 2016. Accessed August 15, 2018.
3. Guide to dental claims submission and payment. American Association of Endodontists. https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/07/2017claimsguide_vfinal.pdf. Published 2017. Accessed August 15, 2018.
4. D1354: Guide to interim caries arresting medicament application (aka silver diamine fluoride). American Dental Association. https://www.ada.org/en/publications/cdt/coding-education. Accessed August 15, 2018.
5. Bauer B. Sedative filling dental code d2940. Bauer & Bauer. https://www.bauersmiles.com/2017/05/sedative-filling-dental-code-d2940.html/. Published May 16, 2017. Accessed August 15, 2018.
6. CDT Coding Companion.American Dental Association. https://ebusiness.ada.org/productcatalog/48165/Coding/J449BT. Accessed January 21, 2019.
7. Code Maintenance Committee. CDT-2017 Substantive action request inventory. American Dental Association. http://www.ada.org/~/media/ADA/Publications/Files/CDT_2017_Substantive_Inventory_March2016.pdf?la=en. Published March 2017. Accessed August 15, 2018.