You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Restoration of endodontically treated teeth is complex,1 and success requires analysis of the situation and forces applied.2 Restored teeth must resist the forces of the oral environment, or failure occurs. Restoration design includes up to five components and their interfaces, all of which may fail.3 Failure occurs with restoration or tooth fracture, dislodgement of a restoration, leakage (which results in caries and restoration removal), or catastrophic failure (eg, root fracture resulting in tooth extraction).4
Endodontically treated teeth fracture more often than vital teeth, with fracture occurrence more so in posterior teeth than anterior teeth because forces are higher and the teeth are weaker.5 Endodontic treatment eliminates pulp tissue and, therefore, nutrients to the tooth. For many years, it was assumed that weak, devitalized dentin led to increased tooth fracture; however, devitalized dentin is as strong as vital dentin and is not a contributory factor.6,7 Increased tooth fracture in endodontically treated teeth is a result of structural breakdown caused by endodontic access.8 The roof of a chamber space within the tooth crown creates an internal arch of tooth structure. An arch provides structural support for a tooth similar to an arch sustaining a highway bridge. Access through a chamber space destroys an arch, resulting in weak, unsupported tooth structure and increased fracture potential. Thin tooth structure from existing restoration, caries, and preexisting cracks further contribute to fracture.
Restorative Classifications of Endodontically Treated Teeth
A restorative design relies on what presents in a tooth, including the number of canals available, the amount of tooth structure remaining, and secondary factors such as chamber space retention or divergent canal interlocking.9 Placing a post within a canal increases the chance of root fracture from drilling and the stresses that a post places on a root. It is most desirable to place no posts for this reason. Retention is critical to success, and an increased number of posts improves retention. Using the least number of posts required is desirable in order to resist maximum forces applied on a tooth and their repetitive application.10
Classifying endodontically treated teeth helps the clinician evaluate restorative situations.9 Classes are determined by the number of canals—Class I is a one canal, Class II is two canals, and Class III is three or more canals. Each class is subdivided by the amount of remaining tooth structure—C is complete tooth structure, P is partial tooth structure, and N is no tooth structure. The amount of tooth structure is determined by the least of two factors, including tooth height and cross section at the gingival third of remaining tooth structure after endodontic treatment. A cross section in the gingival third is used, as a tooth may have full height but be a hollow shell providing little support. The amount of remaining tooth structure is divided into thirds such that N is less than one third, P is between one third and two thirds, and C is greater than two thirds.9 For example, a Class IIP is a two-canal tooth with partial tooth structure remaining.
The amount of remaining coronal tooth structure determines how much force is applied to a post, cement, and root structure. Increased amounts of coronal tooth structure to accept force decrease force onto other components. Remaining tooth structure reduces force onto a post, so maintaining as much as possible during tooth preparation is desirable.10,11 The strength of the remaining tooth structure is difficult to determine. Dentin or enamel may be weak or cracked. Ascertaining the amount of force applied to a tooth is even more complicated. Failure occurs if inadequate resistance to forces is provided, so restorative design must assume maximum forces and more-than-adequate resistance.12,13
Case 1
A Class IN maxillary bicuspid was previously restored with a fiber post and an all-porcelain crown (Figure 1). The forces of the oral environment resulted in fracture of the fiber post and crown failure. The remaining fiber post in the root was removed, and anti-rotational areas were prepared for a cast post (Figure 2). A gold cast post was constructed at a dental laboratory, using an indirect technique (Figure 3). A porcelain-fused-to-metal (PFM) crown was constructed with a bevel finish to provide a ferrule and reduce forces on the post (Figure 4 and Figure 5).
Forces of the Oral Environment
Chewing, clenching, grinding, and parafunctional habits such as chewing fingernails or pens create forces on teeth. Analysis of force includes intensity, frequency, duration, and direction. Intensity is the amount of force applied, frequency is how often force is applied, duration is how long force is applied to a tooth, and direction is dictated by where force is applied on a tooth. Pressure straight down or straight up creates compressive, tensile, or shear force on components. Force on a tipped tooth or cusp incline creates lateral forces, and off-center force on a tooth results in rotational force. The most customary forces are intermittent of various frequencies but not always of maximum intensity or duration.14
Force frequency, intensity, and duration are hard to determine. Certain indicators can be used to judge force intensity, which include tooth position, muscle size, jaw angle, mouth area, diet, habits, general health, and longevity of the existing restorations.15
Tooth position contributes to force intensity when applied to a tooth. For example, a normally positioned central incisor does not generate as much force biting into a bagel as a central incisor that is labially tipped.16 A larger biting surface increases force; large muscles generate more than small ones.17 Jaw angle determines leverage force such that a low-angle case generates more force than a high-angle case.18 Posterior teeth produce more force than anterior teeth—a second molar creates as much as five times more pressure than a first bicuspid in the same mouth.
Dietary habits are contributory factors. Different foods require various amounts of chewing force;19 soft foods necessitate less force than hard foods do. Tooth size and periodontal health affect force intensity; a tooth with a large coronal portion creates larger leverage force while tooth mobility lessens force. Night bruxism intensifies normal pressure 10 times because proprioception is lost in REM sleep.20,21
The longevity of existing restorations is a good indicator of force. A long-lasting large amalgam or composite with weak tooth structure surrounding it indicates there are minimal forces because the tooth structure or restoration would have fractured if there were intense forces.
Restoration Components
Overall restoration strength is determined by the strength of its components and their interfaces. Five components are used to restore endodontically treated teeth, although not all are used in each case. Each component varies by material, method of manufacturing, technique, and/or shape. The five basic restorative components include tooth, cement, post, core, and restoration. Components have interfaces that must resist forces in the oral environment.
Each component’s resilience is defined by its material strength, including compressive, shear, tensile, modulus of elasticity, fatigue, modulus of deformation, and material thickness.22,23 A tooth crown and root have a specific, predetermined size, and components fit these dimensions. As one component increases in size, another component decreases. For example, as a post is made wider, tooth structure is removed and the root cross section decreases. The post strengthens, but the root weakens. A component is further weakened by shrinkage, contraction or expansion, impurities, cracks, fabrication stress, fatigue, and altering of shape.
Component interfaces further define restoration strength. Forces on teeth create component separation and breakdown. The most common interface breakdown is cement-to-root or cement-to-post interfaces, especially when there is no coronal tooth structure.24,25 A round preformed post is placed in a round root canal space. Rotational forces break cement-to-post or cement-to-root interfaces as a post wants to spin. Creating areas out of round such as slots or pins help resist rotation.
Case 2
A Class IIIN maxillary left second molar required restoration (Figure 6). Four canals, a chamber space, and little cross section of tooth structure were in the gingival third. Gutta-percha was removed with a Peeso reamer supplied in the C-1 kit. The canal was shaped with a bur in the kit, which was the same size as the corresponding post (Figure 7). The tooth structure was bonded with Brush & Bond™ (Parkell, www.parkell.com), and then the resin cement was spun into the canal with a lenticulo spiral. A C-1 white post was placed in the palatal canals (Figure 8). The C-1 White Post is a fiber-reinforced composite post, which flexes at the same rate as dentin to minimize root stresses.
Core build-up was completed with Absolute Dentin™ (Parkell, www.parkell.com) dual-cure high-strength core composite. There are variations on color and how materials cure. For example, Light-Core™ (Bisco, www.bisco.com) is a light-cured blue material, Encore® (Centrix, www.centrixdental.com) is a self-cure white material, and Para Core (Coltène Whaledent, www.coltene.com) is a dual-cure white or dentin-colored material. Material was placed directly and light-cured for 40 seconds (Figure 9). Final preparation for a PFM was completed (Figure 10). The final crown was placed (Figure 11).
Tooth structure is evaluated in the coronal and root areas. Coronal tooth structure provides maximum resistance to forces in comparison to posts, cores, and cements, so maintaining as much as possible is desirable. Root structure and canals have specific sizes and shapes. Both the root and canal are tapered in the coronal to apical directions. A tapered post fitting into a tapered canal maintains maximal tooth structure for root strength but creates a wedging effect that may fracture roots.26 Materials such as fiber posts with flex and compression similar to dentin minimize wedging. A parallel post removes tooth structure decreasing root strength, increasing the chance of root fracture but eliminating a tapered wedging effect.27
Bonding to dentin in a canal improves the cement strength to tooth structure interface; however, bonding in a canal is difficult. This is because endodontic and temporary cements may contain eugenol (which inhibits resin set), dentin tubules are often sealed with endodontic materials, and excess amounts of moisture are hard to eliminate.28,29 Bonding is also challenging when collagen fibers compress, blocking access to dentin. It is not advisable to depend on root canal bonding. Bonding coronal dentin close to endodontic areas is effective; however, it is less so than to dentin in other areas of teeth. Dentin close to a chamber space has less dentin for bonding because of the large number and size of the dentin tubules.
Cement is used to retain a post and restoration. Cement failure occurs from forces shearing or compressing cement and interface separation. Cements may shrink or expand during curing, which creates internal and interface stresses, and some dissolve in saliva if leakage occurs. The most commonly used are glass ionomer, resin ionomer, resin, polycarboxylate, and zinc phosphate. Resin and resin-ionomer cements have become the most popular with their ability to bond to tooth structure, creating strong interfaces.30,31 Resin cements shrink while resin ionomers expand on curing.
Posts are comprehensively categorized by shape, material, design, and method of construction. Two basic post categories are cast and preformed. Cast posts are constructed of gold or non-precious alloys in a dental laboratory and formed from direct or indirect techniques. Cast posts are useful when no coronal tooth structure exists and forces are high. They eliminate the need for core materials and interfaces of core-to-post and core-to-cement-and-crown interfaces. Cast posts are also useful to incorporate slots or out-of-round areas in tooth structure that resist rotational forces.32,33
Preformed posts are tapered or parallel. They are further distinguished as metal, ceramic, or fiber. Fiber posts have become popular because they flex at rates similar to tooth structure. A post that does not flex similar to tooth structure creates stresses on roots that may cause root fracture.34-36 Preformed posts are passive or engage root structure. A post that engages root structure is more retentive, however; stress points create more factures.
Preformed posts consist of a portion that goes into a root and portion that extends above a root into a coronal area. The root portion of a post ideally is designed to resist rotation, provide retention, allow cement venting, and leave room for cement.24,25 Cement-to-post interfaces are directly improved by grooves, roughness, and shaping. A drill prepares a root canal space to accept a post. A parallel post requires a drill to be slightly larger than a post to provide for cement and cement can vent out during post placement. A tapered post allows easy cement venting.
The coronal portion of a post requires a mechanical resistance and/or an adhesive design to hold core material. The amount of remaining coronal tooth structure that resists forces determines how strong this post to core resistance must be.37 A post-to-core interface should resist all directions of force. Core material is retained by a post, interface adhesion such as bonding to tooth structure, and mechanical tooth retention as occurs with multiple posts or using chamber space.
Core materials transfer strength from tooth structure to a restoration such as a crown. It is used with or without a post. Core material ideally has characteristics similar to tooth structure. Core material characteristics are critical when no coronal tooth structure exists. A core material that is very hard places excessive force onto a post. One that is too soft allows a restoration to move, causing microleakage and breakdown at the margins. Core material retention and resistance are improved by the number of posts, pins, adhesion to tooth structure, mechanical retention of a chamber space, interlocking of a post to chamber space or diverging/converging posts or core material placed into canals.30,38
Restorations are required to close access holes and support weak tooth structure. Endodontically treated anterior teeth are not significantly weakened by access holes and do not require crowning for support.39 Anterior teeth with existing restorations combined with lost tooth structure from endodontic access may be weak and require crowning.39 Posterior teeth have a high incidence of tooth fracture following endodontic treatment, so crowning is recommended.40 Analysis of force is important, and teeth that receive minimal forces may not require crowns.
Crown selection is important to restoration success. A collar of metal on a PFM or an all-metal crown reduces forces onto posts. The ferrule effect is a mechanical engineering design that distributes lateral forces onto a collar, reducing forces onto a post by approximately 30%.41 An all-porcelain crown does not allow for a collar and therefore has no ferrule effect, so it requires adequate support from the tooth structure, post, core, and cement.
Case 3
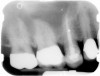
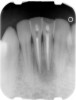
Class IC mandibular central incisors had extensive amounts of tooth structure remaining following endodontic treatment (Figure 12 and Figure 13). Restoration of the access holes was completed with bonded composite (Figure 14).
Failure of Endodontic Restoration
Restorations of endodontically treated teeth provide health, function, and esthetics. A restoration that no longer provides those elements is a failure. Catastrophic failure happens if the tooth structure fractures or caries occurs in such a manner that restoration is impossible. Restoration, core, post, and tooth fracture; cement breakdown; and core-to-post separation are the most common causes of failure.
Many factors contribute to tooth fracture after endodontic treatment, including lost tooth structure from endodontic access and tooth preparation, endodontic instrumentation and irrigation, obturation, post preparation, post stress on insertion and in function, and coronal restoration.42
Case 4
A terminally ill patient presented an abscess on the maxillary right central incisor. Endodontic treatment was completed with a composite restoration placed to restore the access hole. The crown fractured off within 1 week (Figure 15 and Figure 16). Gutta-percha was removed, and the canal prepared to accept a C-1 white post (Figure 17). The root was bonded with BRUSH and BOND™ (Parkell, www.parkell.com) and the post was cemented with a resin cement (Figure 18). Absolute Dentin core build-up material was applied (Figure 19). There are many different build-up materials, including glass ionomers such as Ketac-Silver™ (3M ESPE, www.3mespe.com) or Miracle Mix® (GC America, www.gcamerica.com), pastes that are mixed such as Zenith (Carson Dental, www.carsondental.com), and automix syringes such as Absolute Dentin. The material was of a consistency that allows placement without sagging or running (Figure 20). It was light-cured and prepared for temporization (Figure 21) and the final all-composite restoration was delivered (Figure 22).
Conclusion
Restoration of endodontically treated teeth is complex. Understanding intraoral forces, restoration design, components, and component interfaces is critical for long-term success.
References
1. Vârlan C, Dimitriu B, Vârlan V, et al. Current opinions concerning the restoration of endodontically treated teeth: basic principles. J Med Life. 2009;2(2):165-172.
2. Chalifoux PR. Esthetic restoration of endodontically treated teeth: factors that affect prognosis. J Esthet Dent. 1998;10(2):75-83.
3. Ree M, Schwartz RS. The endo-restorative interface: current concepts. Dent Clin North Am. 2010;54(2):345-374.
4. Zarow M, Devoto W, Saracinelli M. Reconstruction of endodontically treated posterior teeth—with or without post? Guidelines for the dental practitioner. Eur J Esthet Dent. 2009;4(4):312-327.
5. Tang W, Wu Y, Smales RJ. Identifying and reducing risks for potential fractures in endodontically treated teeth. J Endod. 2010;36(4):609-617.
6. Sedgley CM, Messer HH. Are endodontically treated teeth more brittle? J Endod. 1992;18(7):332-335.
7. Carter JM, Sorensen SE, Johnson RR, et al. Punch shear testing of extracted vital and endodontically treated teeth. J Biomech. 1983;16(10):841-848.
8. Goto Y, Ceyhan J, Chu SJ. Restorations of endodontically treated teeth: new concepts, materials, and aesthetics. Pract Proced Aesthet Dent. 2009;21(2):81-89.
9. Chalifoux PR. Restoration of endodontically treated teeth: review, classification, and post design. Pract Periodontics Aesthet Dent.1998;10(2):247-254.
10. Cobankara FK, Unlu N, Cetin AR, et al. The effect of different restoration techniques on the fracture resistance of endodontically-treated molars. Oper Dent. 2008 ;33(5):526-533.
11. Al-Wahadni AM, Hamdan S, Al-Omiri M, et al. Fracture resistance of teeth restored with different post systems: in vitro study [published online ahead of print June 13, 2008]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(2):e77-e83.
12. Torabi K, Fattahi F. Fracture resistance of endodontically treated teeth restored by different FRC posts: an in vitro study. Indian J Dent Res. 2009;20(3):282-287.
13. Al-Wahadni AM, Hamdan S, Al-Omiri M, et al. Fracture resistance of teeth restored with different post systems: in vitro study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(2):e77-e83.
14. Jung SH, Min KS, Chang HS, et al. Microleakage and fracture patterns of teeth restored with different posts under dynamic loading. J Prosthet Dent. 2007;98(4):270-276.
15. Al-Omiri MK, Mahmoud AA, Rayyan MR, et al. Fracture resistance of teeth restored with post-retained restorations: an overview. J Endod. 2010;36(9):1439-1449.
16. Garbin CA, Spazzin AO, Meira-Júnior AD, et al. Biomechanical behaviour of a fractured maxillary incisor restored with direct composite resin only or with different post systems [published online ahead of print August 18, 2010]. Int Endod J.
17. Paphangkorakit J, Osborn JW. Effects on human maximum bite force of biting on a softer or harder object. Arch Oral Biol. 1998;43(11):833-839.
18. Fields HW, Proffitt WR, Case JC, et al. Variables affecting measurements of vertical occlusal force. J Dent Res. 65(2):135-138.
19. Svensson KG, Trulsson M. Regulation of bite force increase during splitting of food. Eur J Oral Sci. 2009;117(6):704-710.
20. Shigeyuki S, Masahiko I, Hiroshi K, et al. Analysis of bruxism occlusal force concerning formation of facet on occlusal splint for estimation of bruxism. Japanese Journal of Conservative Dentistry. 2006;49(1):6-16.
21. Schindler HJ, Türp JC, Blaser R, et al. Differential activity patterns in the masseter muscle under simulated clenching and grinding forces. J Oral Rehabil. 2005;32(8):552-563.
22. Tapley BD, ed. Eshboch’s Handbook of Engineering Fundamentals. 4th ed. New York, NY: Wiley-Interscience Publication; 1990.
23. Hick T. Standard Handbook of Engineering Calculations. 3rd ed. New York, NY: McGraw-Hill; 1995.
24. Mayhew JT, Windchy AM, Goldsmith LJ, et al. Effect of root canal sealers and irrigation agents on retention of preformed posts luted with a resin cement. J Endod. 2000;26(6):341-344.
25. Nergiz I, Schmage P, Ozcan M, et al. Effect of length and diameter of tapered posts on the retention. J Oral Rehabil. 2002;29(1):28-34.
26. Theodosopoulou JN, Chochlidakis KM. A systematic review of dowel (post) and core materials and systems. J Prosthodont. 2009;18(6):464-472.
27. Sorensen JA, Martinoff JT. Clinically significant factors in dowel design. J Prosthet Dent. 1984;52(1):28-35.
28. Wu H, Hayashi M, Okamura K, et al. Effects of light penetration and smear layer removal on adhesion of post-cores to root canal dentin by self-etching adhesives. Dent Mater. 2009;25(12):1484-1492.
29. Demiryürek EO, Külünk S, Saraç D, et al. Effect of different surface treatments on the push-out bond strength of fiber post to root canal dentin. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108(2):e74-e80.
30. Baldissara P, Ozcan M, Melilli D, et al. Effect of cyclic loading on fracture strength and microleakage of a quartz fiber dowel with different adhesive, cement and resin core material combinations. Minerva Stomatol. 2010;59(7-8):407-414.
31. Demiryürek EO, Külünk S, Yüksel G, et al. Effects of three canal sealers on bond strength of a fiber post. J Endod. 2010;36(3):497-501.
32. Gómez-Polo M, Llidó B, Rivero A, et al. A 10-year retrospective study of the survival rate of teeth restored with metal prefabricated posts versus cast metal posts and cores. J Dent. 2010;38(11):916-920.
33. Mou YB, Chen YM, Smales RJ, et al. Optimum post and tooth root diameters for a cast post-core system. Am J Dent. 2009;22(5):311-314.
34. Magne P, Oganesyan T. Premolar cuspal flexure as a function of restorative material and occlusal contact location. Quintessence Int. 2009;40(5):363-370.
35. Liu CL, Gao X, Lan J, et al. Fracture behavior of mandibular premolars with flared root canals restored with different post-and-core systems and root rehabilitation [article in Chinese]. Hua Xi Kou Qiang Yi Xue Za Zhi. 2010;28(3):286-289.
36. Santos AF, Meira JB, Tanaka CB, et al. Can fiber posts increase root stresses and reduce fracture? J Dent Res. 2010;89(6):587-591.
37. Nam SH, Chang HS, Min KS, et al. Effect of the number of residual walls on fracture resistances, failure patterns, and photoelasticity of simulated premolars restored with or without fiber-reinforced composite posts. J Endod. 2010;36(2):297-301.
38. Al-harbi F, Nathanson D. In vitro assessment of retention of four esthetic dowels to resin core foundation and teeth. J Prosthet Dent. 2003;90(6):547-555.
39. D’Arcangelo C, De Angelis F, Vadini M, et al. Fracture resistance and deflection of pulpless anterior teeth restored with composite or porcelain veneers. J Endod. 2010;36(1):153-156.
40. Gogna R, Jagadish S, Shashikala K, et al. Restoration of badly broken, endodontically treated posterior teeth. J Conserv Dent. 2009;12(3):123-128.
41. Pereira JR, Valle AL, Shiratori FK, et al. Influence of intraradicular post and crown ferrule on the fracture strength of endodontically treated teeth. Braz Dent J. 2009;20(4):297-302.
42. Baba NZ, Goodacre CJ, Daher T. Restoration of endodontically treated teeth: the seven keys to success. Gen Dent. 2009;57(6):596-603; quiz 604-5, 595, 679.
About the Author
Paul R. Chalifoux, DDS, Private Practice, Wellesley, Massachusetts