You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Although crown cementation may seem to be a trivial appointment for patients, most clinicians realize that an error during this final step can lead to a poor esthetic outcome, future debonding occurrences, or possibly fracture of a restoration. The clinician must balance the esthetic and retention needs of the restoration with the clinical environment around the tooth preparation. This article will present the important clinical factors to consider when choosing a cement and cementation method for fixed prostheses.
Decision 1: The Choice to Bond With Resin Cement vs Cement With a Glass-Ionomer-based Cement
Glass-ionomer and resin-modified glass-ionomer (RMGI) cements are used for the majority of single-tooth crown cementations in the United States. The decision to choose a resin cement instead of a glass-ionomer or RMGI cement is dependent on the ability to isolate the tooth, the need for crown retention, the esthetic requirements of the case, and the strength of the crown restorative material.
A minimally retentive or non-retentive preparation benefits from the use of adhesive bonding with a resin cement because resin cements have been shown to produce greater crown retention than RMGI cements.1 Examples of minimal retention include inlays, onlays, and short or over-tapered crown preparations; examples of non-retention include veneers, overlays ("vonlays"), and Maryland bridges. Although bonding to dentin with a resin-based material in a well-isolated field can produce much higher bond than using an RMGI, if dentin becomes contaminated with saliva, the bond to the resin-based material will drop below that of the RMGI.2 Therefore, the primary contraindication for the use of a resin cement would be the inability to achieve adequate isolation. Achieving isolation when bonding a fixed prosthesis may be challenging. If the margins are supragingival, as in the case of many onlays, it may be possible to use a rubber dam (Figure 1). A technique for achieving isolation for posterior mandibular teeth is to lay a cardboard cheek retractor both lingual and buccal to the tooth (Figure 2).
Although saliva is detrimental to a bonded restoration, an even more harmful contaminant is the presence of blood, which may leave a film of fibrinogen and platelets on the surface of dentin. Blood will not only decrease the bond strength to the resin cement, it may also discolor the restoration. Ideally, patients should have healthy gingival tissue before a restoration is bonded. If necessary, a chlorhexidine rinse could be prescribed 1 week before the final restorations are bonded. If minor bleeding occurs when the temporary crown is removed, a ferric sulfate or aluminum chloride-containing astringent can be used to stop the bleeding. Although ferric sulfate is very effective at stopping bleeding, it can leave iron-containing precipitates that will interfere with the bond to tooth structure. Cleaning these precipitates can be achieved with either phosphoric acid or ethylenediaminetetraacetic acid (EDTA) followed by water rinsing.3
For some dental ceramics, it is necessary to bond the ceramic restoration to tooth structure to reinforce the restoration. Feldspathic porcelain must be bonded to tooth structure to transfer force to the underlying tooth. Glass-ceramics (such as lithium disilicate and lithium silicate) have shown similar crown fracture strength when cemented with RMGI and when bonded with resin cement if the crown thickness is 1.5 mm or greater.4,5 A laboratory study reported that 0.8-mm-thick lithium-disilicate crowns cemented with RMGI failed during fatigue, whereas those bonded with resin cement did not.6 Some studies have shown that the strength of traditional zirconia (3 mol% yttria) is not affected by cementing with an RMGI cement, even at a 0.5-mm thickness.5,7
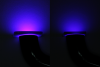
A final consideration when using RMGI cements is that they are typically white opaque, which suggests they may increase the brightness and decrease the translucency of a translucent ceramic crown. A recent study of 0.6-mm translucent zirconia (5 mol% yttria) reported that the use of RMGI cement caused color change in the direction of higher value (brighter) and within a visually perceptible range.8 Interestingly, the use of RMGI cement caused less color change and equivalent change in translucency than a resin cement.8 Many resin cements are available, with several different colors and translucencies that may be used to affect the esthetics of the final crown. Several cured cements are shown in Figure 3.
Decision 2: The Choice of What Type of Resin Cement to Use
If the clinical scenario calls for the use of a resin cement, two general options are available: a conventional resin cement or a self-adhesive resin cement. A conventional resin cement is used in combination with either a dedicated self-etch primer or a self-etch or total-etch bonding agent on the tooth (Figure 4). A self-adhesive resin cement, on the other hand, is used without applying any type of primer or adhesive to the tooth structure before bonding. Self-adhesive resin cements contain acidic resin monomers that are capable of simultaneously demineralizing dentin and infiltrating the collagen matrix. Some laboratory research has indicated conventional resin cements provide a superior bond strength when bonding to dentin.9,10 However, other studies have shown equal bond strength with self-adhesive and conventional resin cements.11,12 Pre-etching with phosphoric acid may increase the bond strength when using a self-adhesive resin cement during bonding to enamel.11,12 In summary, the benefit of using a self-adhesive resin cement is that it requires fewer steps and therefore a shorter amount of time for which isolation is necessary; conventional resin cement, on the other hand, may produce a higher bond. Self-adhesive resin cements are well suited for full-mouth fixed restorations due to the time required to maintain isolation and bond multiple restorations.
Although self-adhesive resin cements do not require treatment of the tooth surface before bonding, surface treatment of a ceramic surface before bonding should be accomplished identically for self-adhesive and conventional resin cements. Glass-containing ceramics should be etched with hydrofluoric acid and primed with a silane-containing solution. Zirconia ceramics should be particle abraded and primed with a 10-methacryloxydecyl dihydrogen phosphate (MDP)-containing solution. Some self-adhesive resin cements have been modified to contain MDP to eliminate the need for an MDP primer, thereby further simplifying the bonding procedure. A systematic review reported that MDP-containing cements presented higher bond than MDP-free cements.13Another study showed that the separate application of an MDP primer was more effective than incorporating MDP into the cement.14
Another consideration when selecting a conventional resin cement is whether to light-polymerize the primer/adhesive that is used on the tooth (Figure 5). Many clinicians fear that light-curing the adhesive under an indirect restoration will produce a film thickness that will prevent complete seating of the restoration. Figure 6 presents a cross-section of a cured, highly filled adhesive that was stained pink on an extracted tooth prepared for a crown with a rounded and sharp internal finish line. The greatest film thickness was measured as 100 μm in the sharp internal line angle (Figure 7) and 30 μm on the side with the rounded internal line angle (Figure 8). This film thickness should not prevent the seating of a crown with a 100-μm die spacer. Some resin cements contain an initiator for the adhesive within the cement that allows the adhesive to polymerize via "contact cure." One study demonstrated that separate light-curing of the adhesive produced a greater bond than when the adhesive was allowed to cure along with the cement.15
Decision 3: The Choice of How to Cure the Cement Under the Crown
Resin cements are formulated in self-cure, light-cure, and dual-cure modes. Light-cure resin cements offer the clinician increased working time and cure on demand, which is particularly beneficial for ceramic veneers. Dual- and self-cure resin cements are advantageous for clinical situations in which light-curing cannot access the cement, such as thick or opaque restorations.
With the use of dual-cure cements, the clinician has the option of light-curing the cement to initiate the cement polymerization. The opacity of some ceramics (particularly zirconia) has left clinicians to question the advantage of curing through the crown (Figure 9). Laboratory studies have reported that curing light will pass through traditional zirconia (3 mol% yttria) restorations, albeit with an irradiance that decreases significantly with darker shades and thicker restorations.16 The author suggested that A1- or B1-shade zirconia benefited from light polymerization up to 1.5-mm thickness, whereas darker shades benefited only up to 0.5-mm thickness. An additional advantage of light-curing dual-cure cements is that it has been shown to impart improved wear resistance at the marginal gap for some cements.17
One disadvantage of self- or dual-cure cements is that the benzoyl peroxide/amine redox initiator system traditionally used to initiate a chemical cure causes these materials to change color over time.18 Additionally, this amine-based initiator system can become inactivated when used in combination with an acidic primer/adhesive. In other words, if the clinician uses a self-etching adhesive on the tooth preparation before using a self-cure or dual-cure cement, the adhesive could prevent the cement from curing and bonding to the tooth. Some adhesives come with a separate bottle, called a dual-cure activator, which makes the adhesive compatible with dual-cure and self-cure materials.19 Another solution to avoid both these unwanted effects is to use an amine-free cement.
Conclusions
Resin cements should be used only after all blood contamination has been removed and isolation from saliva is achieved. Resin cements are necessary to increase crown retention but are also necessary for lithium-disilicate restorations that are thinner than 1.5 mm. Self-adhesive resin cements allow a simplified procedure, but the highest crown retention may be achieved with use of a separate primer/adhesive and a conventional resin cement; the optimum bond is achieved when the primer/adhesive is cured under the conventional resin cement. Light-curing of the cement should be performed through ceramic crowns; however, the effect of the light diminishes with thicker and darker zirconia crowns. Light-curing the cement at the margin helps prevent against cement wear. Amine-free resin cements are more color stable and can be used with self-etching (acidic) primers/adhesives.
About the Authors
Celin Arce, DDS, MS
Assistant Professor
Restorative Sciences Department
School of Dentistry
University of Alabama at Birmingham
Birmingham, Alabama
Augusto Robles, DMD, MS
Associate Professor
Director of Operative Dentistry Curriculum
School of Dentistry
University of Alabama at Birmingham
Birmingham, Alabama
Nathaniel C. Lawson, DMD, PhD
Director, Division of Biomaterials
School of Dentistry
University of Alabama at Birmingham
Birmingham, Alabama
References
1. Heintze SD. Crown pull-off test (crown retention test) to evaluate the bonding effectiveness of luting agents. Dent Mater. 2010;26(3):193-206.
2. Shimazu K, Karibe H, Ogata K. Effect of artificial saliva contamination on adhesion of dental restorative materials. Dent Mater J. 2014;33(4):545-550.
3. Bernades Kde O, Hilgert LA, Ribeiro AP, et al. The influence of hemostatic agents on dentin and enamel surfaces and dental bonding: a systematic review. J Am Dent Assoc. 2014;145(11):1120-1128.
4. Preis V, Behr M, Hahnel S, Rosentritt M. Influence of cementation on in vitro performance, marginal adaptation and fracture resistance of CAD/CAM-fabricated ZLS molar crowns. Dent Mater. 2015;31(11):1363-1369.
5.Zesewitz TF, Knauber AW, Nothdurft FP. Fracture resistance of a selection of full-contour all-ceramic crowns: an in vitro study. Int J Prosthodont. 2014;27(3):264-266.
6. Kwon S, Lawson NC, Burgess JO, Morris GP. Fracture load of zirconia and lithium disilicate crowns [abstract]. J Dent Res. 2018;97(spec iss A). Abstract 247.
7. Nakamura K, Mouhat M, Nergård JM, et al. Effect of cements on fracture resistance of monolithic zirconia crowns. Acta Biomater Odontol Scand. 2016;2(1):12-19.
8. Malkondu O, Tinastepe N, Kazazoglu E. Influence of type of cement on the color and translucency of monolithic zirconia. J Prosthet Dent. 2016;116(6):902-908.
9. Viotti RG, Kasaz A, Pena CE, et al. Microtensile bond strength of new self-adhesive luting agents and conventional multistep systems. J Prosthet Dent. 2009;102(5):306-312.
10. Rippe MP, Amaral R, Oliveira FS, et al. Evaluation of tensile retention of Y-TZP crowns cemented on resin composite cores: effect of the cement and Y-TZP surface conditioning. Oper Dent. 2015;40(1):E1-E10.
11. Hikita K, Van Meerbeek B, De Munck J, et al. Bonding effectiveness of adhesive luting agents to enamel and dentin. Dent Mater. 2007;23(1):71-80.
12. Rodrigues RF, Ramos CM, Francisconi PA, Borges AF. The shear bond strength of self-adhesive resin cements to dentin and enamel: an in vitro study. J Prosthet Dent. 2015;113(3):220-227.
13. Özcan M, Bernasconi M. Adhesion to zirconia used for dental restorations: a systematic review and meta-analysis. J Adhes Dent. 2015;17(1):7-26.
14. Zhao L, Jian YT, Wang XD, Zhao K. Bond strength of primer/cement systems to zirconia subjected to artificial aging. J Prosthet Dent. 2016;116(5):790-796.
15. Lührs AK, Pongprueksa P, De Munck J, et al. Curing mode affects bond strength of adhesively luted composite CAD/CAM restorations to dentin. Dent Mater. 2014;30(3):281-291.
16. Ilie N, Stawarczyk B. Quantification of the amount of light passing through zirconia: the effect of material shade, thickness, and curing conditions. J Dent. 2014;42(6):684-690.
17. Tsujimoto A, Barkmeier WW, Takamizawa T, et al. Relationship between simulated gap wear and generalized wear of resin luting cements. Oper Dent. 2017;42(5):E148-E158.
18. Smith DS, Vandewalle KS, Whisler G. Color stability of composite resin cements. Gen Dent. 2011;59(5):390-394.
19. Gutiérrez MF, Sutil E, Malaquias P, et al. Effect of self-curing activators and curing protocols on adhesive properties of universal adhesives bonded to dual-cured composites. Dent Mater. 2017;33(7):775-787.