You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The ADAA has an obligation to disseminate knowledge in the field of dentistry. Sponsorship of a continuing education program by the ADAA does not necessarily imply endorsement of a particular philosophy, product, or technique.
Radiography involves the use of ionizing radiation and thus is potentially dangerous if mishandled. For the sake of the dental profession, patients, and the public, it is essential that licensed dental radiographers gain and maintain required knowledge of radiographic techniques and radiation health and safety, prior to performing clinical procedures.
This course is intended to provide current, vital information on receptor and tube head placement, serve as a guide to acquire new skills or refine current skills, and allow for progressive self-assessment throughout the course.
With the advent of reusable phosphor plates and solid-state detectors (digital sensors) we have adopted language, which will address all receptor types - film, phosphor plates, and electronic or digital sensors. It is inappropriate to call the image produced by using x radiation an "x-ray." Even the term radiograph(s) now becomes "radiographic image(s)", and the device used to capture the information should now be called an "image receptor" or simply "receptor."
Intraoral Procedures
The intraoral radiographic image, when correlated with the case history and clinical examination, is one of the most important diagnostic aids available to the dental practitioner. When examined under proper conditions, diagnostic-quality intraoral images reveal evidence of disease that cannot otherwise be found. They also play a major role in forensic identification.
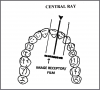
Two of the fundamental rules of radiography are that 1) the central beam should pass through the area to be examined, and 2) the radiographic receptor should be placed in a position to record the image with the least amount of image distortion. Three types of intraoral radiologic examinations commonly used in dental practice-periapical, bitewing (interproximal), and occlusal examinations-depend on the operator's adherence to these two rules even though specific techniques, processes, and indications differ widely among them.
Another aspect that these three examinations have in common pertains to the traditional radiographic receptor. The radiographic receptor has two sides; a tube side and a tongue side. The tube side may be plain or textured. When placed intraorally, the tube side always faces the radiation source which is the tube head. The tongue side may be colored and has a flange to open the packet and remove the receptor. When placed intraorally, the tongue side always faces the patient's tongue, except in the case of the mandibular occlusal examination.
As technology advances, digital imaging is replacing traditional radiographic receptors in the dental office. The conveniences associated with digital imaging make it an attractive alternative to traditional films, while the basic mechanics and principles of radiographic technique remain the same. Digital radiographic receptors/sensors and modified receptor holders are employed to obtain images. Like traditional radiographic imaging, the clinician is responsible for the majority of errors and retakes that occur in dental imaging.
Patient anatomic variations such as narrow arches, missing teeth, or the presence of tori, coupled with limitations of the patient's ability to open sufficiently, or maintain the receptor placement, are reasons a clinical examination must precede the taking of radiographic images. After the clinical examination, the operator can determine the number and size of radiographic images to expose, the technique modifications necessary, and the type of receptor holding devices to be employed.
Advancements are continually being made in the development and manufacturing of the traditional film packet. These advancements have helped to decrease radiation exposure. When using traditional radiographic film, the "fastest" speed should be used.
Periapical Radiographic Images
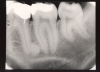
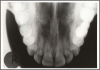
The purpose of the intraoral periapical examination is to obtain a view of the entire tooth and its surrounding structures, as in Figure 1. Two exposure techniques may be employed for periapical radiography: the paralleling technique and the bisecting angle technique. The paralleling technique is the preferred method. This technique provides less image distortion and reduces excess radiation to the patient. The paralleling technique should always be attempted before other techniques. The bisecting technique can be employed for patients unable to accommodate the positioning of the paralleling technique. Candidates may include those with low palatal vaults and children. Disadvantages to the bisecting technique include image distortion and excess radiation due to increased angulations involving the eye and thyroid glands. Regardless of the technique, however, the rules of radiography referred to earlier must be followed.
Bitewing Radiographic Images
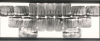
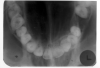
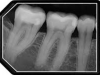
Bitewing examinations were introduced by Dr. Raper in 1925. Bitewing images focus on the clinical crowns of both the maxillary and mandibular teeth. Bitewings do not show the apices of the tooth and cannot be used to diagnose in this area. The greatest value of bitewing radio- graphic images is the detection of interproximal caries in the early stages of development, before it is clinically apparent. The arrows in Figure 2 indicate areas of interproximal caries. Bitewing images also reveal the size of the pulp chamber and the relative extent to which proximal caries have penetrated.
Bitewings also provide a useful adjunct to evaluating periodontal conditions. They offer a good view of the septal alveolar crest, and in addition, permit changes in bone height to be accurately assessed by comparison with adjacent teeth.
Occlusal Radiographic Images
Occlusal radiography is a supplementary radiographic examination designed to provide a more extensive view of the maxilla and mandible.
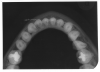
The occlusal image, as seen in Figure 3, is very useful in determining the buccolingual extension of pathologic conditions and provides additional information as to the extent and displacement of fractures of the mandible and maxilla. Occlusal radiographic images also aid in localizing unerupted teeth, retained roots, foreign bodies, and calculi in the submandibular and sublingual salivary glands and ducts. It should be noted that when imaging soft tissues, exposure time needs to be appropriately reduced.
Dentulous Adult Survey
The number of radiographic images needed for a full mouth series varies greatly. Some practitioners may prefer 10 exposures, while others may prefer 18, 20, or more exposures.
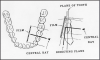
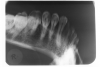
The selection of receptor sizes used in a full mouth series also varies. A full survey can consist of narrow anterior (type 1); standard adult (type 2); type 2 bitewing or long bitewing (type 3) (Figure 4) and may include anterior bitewings. It is generally recommended to use twenty radiographic images --- four bitewings and sixteen periapical images. Eight anterior type 1 radiographic images will allow for ease of receptor placement on patients with narrow palates. However, in some cases six anterior periapical images will cover the area needed.
When using type 3 receptors, only one longer bitewing is used on each side. Opening both the premolar and molar contacts on one radiographic image can be very difficult (Figure 5). With the use of type 2 receptors for bitewings, the operator uses a total of four images. Each image is assigned either premolars or molars (Figure 6). Use of the type 2 instead of type 3 radiographic receptors for bitewings is not only more comfortable for the patient but is easier for the operator to open the contacts.
Edentulous Adult Survey
By definition, an edentulous patient is one without the natural dentition, and a partially edentulous patient is one who retains some, but not all of the natural dentition. Merely because a patient's clinical exam reveals an edentulous state does not disqualify him or her from a diagnostic radiographic examination. In fact, it is commonly accepted that certain areas of the patient's jaws may contain tooth roots or impacted teeth. Residual infection, tumors, cysts, or related pathology may also be found, which, while not visible to the clinician, would hinder the effectiveness and comfort of an appliance such as a denture and could potentially cause life threatening conditions to the patient. In addition to the hidden pathology mentioned above, edentulous surveys reveal the position of the foramina and the type of bone present.
In the case of the partially edentulous patient, placement of the radiographic receptor holding device may be complicated by its tendency to tip or slip into the voids which would normally be occupied by the crowns of the missing teeth. This can usually be overcome by placing cotton rolls between the patient's alveolar ridge and the holder, thereby supporting it in position.
A fourteen or sixteen intraoral periapical survey, as seen in Figure 7, will usually examine the tooth bearing regions in most edentulous patients. Bitewings are not needed because there are no interproximal areas to be examined.
The use of radiographic receptor holders allows the paralleling technique to be used with edentulous patients. The operator may be able to reduce radiation exposure in the edentulous patient by 25% by using the paralleling technique. The radiographic receptor can be held in bite- blocks to which cotton rolls have been taped. To prevent patient discomfort on biting due to missing teeth and resultant over-closing of the arches, the cotton rolls can be attached to the upper and lower surfaces of the biteblocks. Opposing arch denture or partial denture appliances can be left in place to make contact with the biteblock.
The receptor should be positioned with approximately one-third of the vertical dimension protruding beyond the alveolar ridge; that is, the radiographic image should occupy two-thirds of the space. The horizontal angulation of the central beam is perpendicular to the receptor in the horizontal plane. If bisecting, the vertical angulation of the central beam is much increased for an edentulous patient with minimal ridges. The receptor placement may be similar to that of an occlusal image, and this flat receptor placement is the principal cause of dimensional distortion. To determine vertical angulation, it is necessary to estimate the long axis of the ridge instead of the tooth.
Mixed Dentition Survey
The full mouth survey for pediatric patients may vary, depending on the patient's age, eruption pattern, behavior, and the size of the child's mouth. In the six to nine-year-old group, a twelve-image survey, using type 1 narrow receptors is recommended, and would include:
Maxillary:
Central incisors
Right and left lateral incisors and canines
Right and left primary/permanent molars
Mandibular:
Central incisors
Right and left lateral incisors and canines
Right and left primary/permanent molars
Bitewings:
Right and left primary/permanent molars
An adult-sized periapical receptor is used in the posterior region if the child's first permanent molar is fully developed. The size of the tooth requires the use of a large periapical receptor to capture the complete image.
Pre-School Child Survey
Since pre-school children have smaller mouths, reduced size pediatric receptors (type 0) are used to examine the posterior teeth, and adult receptors are used for anterior examinations in children who have only primary (deciduous or "baby") teeth. For this group, an eight-image survey is recommended.
Maxillary:
Central incisors
Right and left primary molars
Mandibular:
Central incisors
Right and left primary molars
Bitewings:
Right and left primary molars
The paralleling technique should be used whenever possible. This technique delivers the lowest dose of radiation possible. The bisecting angle technique is a viable alternative for pediatric radiography because the apices of the permanent molar teeth tend to lie above the palate and below the floor of the mouth in the undeveloped mandible. These positions prevent the image of the apices of the teeth from being projected into the oral cavity when the central beam is perpendicular to the long axis of the teeth as it is when using the paralleling technique.
Quiz
- What should be done before any radiographic examination?
- What are the fundamental rules of radiography?
- What is the purpose of the intraoral periapical examination?
- What are the two primary techniques used in periapical radiography?
- What is the primary purpose of bite wing radiographic images?
- What else can be accurately assessed with bitewings?
- List five indications for taking occlusal radiographic images.
- What sizes of periapical image receptors are commonly used in a dentulous adult survey?
- Why should a radiographic examination be performed for a clinically edentulous patient?
- How should image receptors be positioned relative to the alveolar ridge?
Answers
- A good clinical examination should be carried out before every radiographic examination.
- The central beam should pass through the area to be examined and the image receptor should be placed in position to record the image with the least amount of distortion.
- The purpose of the intraoral periapical examination is to obtain a view of the entire tooth and surrounding structures.
- The two primary techniques used in periapical radiography are paralleling and bisecting angle technique.
- The primary purpose of bitewing radiographic images is for the detection of caries in the early stages of development, especially interproximally.
- Bitewing radiographic images can also be used for the detection of periodontal disease in the early stages.
- Occlusal radiographic images can be used for detection of pathological lesions; fractures of the mandible and maxilla; foreign bodies; salivary calculi; localizing unerupted teeth.
- Type 1, 2, and 3 periapical image recepetors are typically used in a dentulous adult survey.
- It is commonly accepted that certain areas in the jaws may contain roots, impacted teeth, residual infections, tumors, cysts, etc.
- The receptor should be placed with approximately one-third of the vertical dimension protruding beyond the alveolar ridge.
Safety and Infection Control
The CDC published guidelines in 2003 that specifically relate to dental radiography safety and infection control. Operator safety includes wearing all personal protective equipment (PPE) - gloves, mask, eyewear, and protective clothing - to prevent contamination from blood and other bodily fluids that can spatter. Patient protection includes the use of a protective (usually lead lined) apron that must be large enough to cover the sitting patient from neck to knees. The use of a protective thyroid collar is also recommended to reduce exposure to scatter radiation. The protective apron and thyroid collar must be place correctly. If it interferes with the central beam, the radiographic image could be distorted or even undiagnostic. The apron and collar must be disinfected after each use. Each state has determined if a lead apron is required or recommended.
Before any radiographic images can be exposed, the operator must understand the infection control protocols. Potential cross contamination between patient, equipment, and environmental surfaces can happen before, during, and after radiographic image exposure. The use of barriers on machinery and electrical switches are necessary to prevent transmission as they cannot be easily disinfected or could receive an electrical short from a chemical spray.
Each office must establish a protocol from preparation, to exposure, to processing in order to maintain the aseptic chain. Collection and transportation of contaminated receptors from the patient room to the dark room must occur in a way that office surfaces are not contaminated. Contaminated gloves must be removed before entering the daylight loader of an automatic processor to prevent contamination. Contaminated receptors that enter a processor will contaminate the processor and solutions and still exit the machine contaminated, so a spill-technique protocol must be established to maintain the aseptic chain. The spill technique involves opening and spilling out the radiographic receptor while only touching the outer surface of the packet with contaminated gloves, thereby never contaminating the receptor itself. Several steps from beginning to end are involved and each one should be examined by the dental team to prevent possible cross contamination.
Quiz
- What PPE should be worn by the operator?
- How often should the protective apron be disinfected?
- Why are barriers placed on electrical switches?
- Why must contaminated gloves be removed before entering the daylight loader of a processor?
Answers
- The operator should wear gloves, masks, eyewear, and protective clothing.
- The apron should be disinfected after each use.
- Electrical switches are covered to maintain the aseptic chain and to prevent damage such as an electrical short.
- Contaminated gloves must be removed because they will contaminate the sleeves and, therefore, the machine and all radiographic images thereafter.
Paralleling Technique
Basic Principles
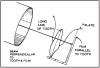
The paralleling technique of intraoral radiography was developed by Gordon M. Fitzgerald, and is so named because the tooth, receptor, and end of the position indicating device (PID) are all kept on parallel planes. Its basis lies in the principle that image sharpness is primarily affected by focal-receptor distance (distance from the focal spot within the tube head and the receptor), object receptor distance, motion, and the effective size of the focal spot of the tube.
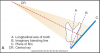
Successfully using the paralleling technique depends largely on maintaining certain essential conditions as illustrated in Figure 8. These are: 1) the receptor should be flat; 2) the receptor must be positioned parallel to the long axis of the teeth; and 3) the central ray of the radiographic beam must be kept perpendicular to the teeth and receptor.
To achieve parallelism between the receptor and tooth (i.e., to avoid bending or angling the receptor) there must be space between the object and receptor. However, remember that as the object-to-receptor distance increases, the image magnification or distortion also increases. To compensate, manufacturers are recessing the target (focal spot) into the back of the tube head. Depending on the machine's age, and placement of the focal spot within the tube head, you may encounter long, medium, or short cones/PIDs. The goal is to have the focal spot at least 12" or 30 cm from the receptor to reduce image distortion.
The anatomic configuration of the oral cavity determines the distance needed between receptor and tooth and varies among individuals. However, even under difficult conditions, a diagnostic quality image can be obtained provided that the receptor is not more than 20 degrees out of parallel with the tooth, and that the face of the PID is exactly parallel to the receptor to produce a central beam which is perpendicular to the long axis of the tooth and the receptor.
The major advantage of the paralleling technique, when done correctly, is that the image formed on the receptor will have both linear and dimensional accuracy. The major disadvantages are the difficulty in placing the receptor and the relative discomfort the patient must endure as a result of the receptor holding devices used to maintain parallelism. The latter is particularly acute in patients with small mouths and in children. In certain circumstances, the receptor and holder may be slightly tipped toward the palate to accommodate oral space and patient comfort. Too much palatal tipping will throw off all parallel planes.
Beam Angulation
The position of the tube head is usually adjusted in two directions: vertically and horizontally. The vertical plane is adjusted by moving the tube head up and down. The horizontal plane is adjusted by moving the tube head from side to side. By convention, deflecting the head so that it points downward is described as positive vertical angulation or + vertical. Correspondingly, an upward deflection is referred to as negative vertical angulation or - vertical. The degree of vertical angulation is usually described in terms of plus or minus degrees as measured by a dial on the side of the tube head.
When applying the paralleling technique, the vertical angulation is the only component to maintaining the parallel plane. There is no set degree number to follow. As stated earlier under basic principles, the tooth, the receptor, and end of the position indicating device (PID) are all kept on parallel planes. If the vertical angulation is excessive, the image will appear foreshortened. Insufficient vertical angulation produces an elongated image.
The beam's horizontal direction determines the degree of overlap among the tooth images at the interproximal spaces. When radiographing relatively aligned teeth, if the central beam is not perpendicular to the interproximal spaces, the teeth will overlap and the spaces between the contacts will close on the image. Imagine a flashlight beam approaching a picket fence at a perpendicular 90-degree angle. The spaces between the pickets will remain open in the shadow image unless the beam angle varies from perpendicular. The degree of overlapping will increase or decrease as the beam angle increases or decreases from perpendicular.
Receptor Holding Devices
The paralleling technique requires the use of receptor holding devices to maintain the relatively precise positioning needed. A great variety of holding devices are commercially available-simple, complex, light, heavy, reusable, disposable, autoclavable, and non-autoclavable. A few of the more common include XCP® (extension cone paralleling) with localizing rings, Snap-a-ray®, Precision rectangular paralleling device, Uni-Bite®, and Stabe bite-block®. Having several options available will provide the operator different opportunities for enhanced patient comfort. It is not uncommon to employ more than one option during the same radiographic survey.
It is the responsibility of the operator to understand how to use and assemble the holding devices. The devices come with directions for putting them together and how to orient the receptor within the holder. The dental radiographer should be able to assess which holder best conforms to the technical and diagnostic requirements of the job, the needs of the patient, and infection control protocols within the office.
Quiz
- What is the basic principle of the paralleling technique?
- What is the major advantage of the paralleling technique?
- What are the major disadvantages?
- What must be done to achieve parallelism between the tooth and receptor?
- List several devices available to position the receptor properly when using the paralleling technique.
Answers
- When using the paralleling technique, the receptor must be positioned parallel to the long axis of the teeth and the central x-ray beam must be kept perpendicular to the teeth and receptor.
- The major advantages of the paralleling technique are linear and dimensional accuracy.
- The major disadvantages of the paralleling technique are difficulty in placement of the receptor, relative discomfort to the patient caused by the receptor holding devices.
- In order to achieve parallelism, the receptor must be placed away from the tooth.
- XCP® with localizing rings, Snap-a-ray®, Precision rectangular devices, Uni-bite®, and Stabe® bite-block are all devices used to position the receptor correctly.
Paralleling Technique Methodology
When taking a full mouth survey, the radiographer should always attempt to follow the same exposure sequence. Since patients tolerate anterior images better, they should be done first. Starting with the maxillary central incisors and proceeding distally, first along one side, then the other, is recommended. The radiographic parameters or exposure factors should also be determined prior to placing receptors in the patient's mouth.
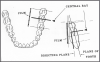
Patient Positioning
When positioning a patient, there are two imaginary planes that must be considered. The occlusal plane runs horizontally, dividing the patient's head into upper and lower portions. It can be visualized by imagining the patient holding a ruler between his or her teeth. A midsagittal plane divides the patient's head or body on a vertical dimension into equal right and left portions (Figure 12).
When using the paralleling technique to examine the maxillary region, the patient is positioned so that the occlusal plane of the maxilla is parallel to the floor and the sagittal plane of the patient's head is perpendicular to the floor.
When paralleling the mandibular region, the patient's position must be modified slightly so that when the mouth is open, the mandible is parallel to the floor and the sagittal plane is perpendicular. This means that the patient might need to be tilted back in the chair.
Before any radiographs are exposed, the patient must be draped with a protective apron and thyroid collar as determined by the state radiation agency. The apron must be properly placed to avoid interference with the radiographic exposure.
Full Mouth Exposure with the Use of XCP Device
It is important to note that the number of exposures can slightly vary between patients. This is due to the number of teeth and the overall size of the oral cavity. Also, some dentists will either include or eliminate the need for bitewing exposures according to the last time these were obtained.
Procedure for the Maxillary Central/Lateral Incisors
- Assemble the anterior receptor holding device and insert the receptor vertically on the anterior biteblock. Use a type 1 receptor.
- Center the receptor on the central/lateral incisors (Figure 14). Position the receptor in the palate as posteriorly as possible so that the entire tooth length will appear on the radiographic image, with approximately a one-eighth inch border on the receptor extending below the incisal edge of the teeth. Position the biteblock on the incisal edges of the teeth to be radiographed (Figure 15). Proper positioning in this step will place the central ray of the radiographic beam between the central and lateral incisors.
- A cotton roll may be inserted between the mandibular teeth and the biteblock for patient comfort. Ask the patient to slowly, but firmly bite onto the block to maintain the correct position.
- Slide the aiming ring down the indicator rod; it should be as close to the skin as possible without actually touching the patient. Align the tube head close to the aiming ring, and center (Figure 16).
- Follow the receptor and equipment manufacturer's recommendation concerning exposure factors. Make the exposure.
- This procedure should be followed for the opposite side central and lateral incisors if needed.
Procedure for the Maxillary Canines
- Assemble the anterior receptor holding device and insert the receptor vertically on the anterior biteblock. Use a type 1 receptor.
- Center the receptor on the canine and first premolar (Figure 17). Position the receptor in the palate as posteriorly as possible so that the entire tooth length will appear on the radiographic image with approximately a one-eighth inch border below the incisal edge of the canine. Position the biteblock on the incisal edges of the teeth to be radiographed (Figure 18). Proper positioning in this step will place the central ray of the x-ray beam between the canine and first premolar.
- A cotton roll may be inserted between the mandibular teeth and the biteblock for patient comfort, especially if the patient has a shallow palate. Ask the patient to slowly, but firmly bite onto the block to maintain the correct position.
- Slide the aiming ring down the indicator rod; it should be as close to the skin as possible without actually touching the patient. Align the tube head close to the aiming ring, and center (Figure 19).
- Follow the receptor and equipment manufacturer's recommendation concerning exposure factors. Make the exposure.
- This procedure should be followed for the opposite side canine radiographic image.
Procedure for the Maxillary Premolars
- Assemble the posterior receptor holding device and insert the receptor horizontally in the posterior biteblock. Use a type 2 receptor.
- Center the receptor on the premolars (Figure 20). The receptor should be parallel with the long axis of the tooth (Figure 21). Position the receptor in the palate so that the entire tooth length will appear on the radiographic image with approximately a one-eighth inch border below the cuspal ridge. Align the anterior edge of the receptor with the canine so that the image captured on the anterior border of the receptor will include the distal third of the canine. Position the biteblock on the occlusal surfaces of the teeth to be radiographed. Proper positioning in this step will place the central ray of the x-ray beam between the premolars.
- A cotton roll may be inserted between the mandibular teeth and the biteblock for patient comfort. Ask the patient to slowly, but firmly bite onto the block to maintain the correct position. (The occlusal border of the receptor tends to slip lingually.)
- Slide the aiming ring down the indicator rod; it should be as close to the skin as possible without actually touching the patient. Align the tube head close to the aiming ring, and center (Figure 22).
- Follow the receptor and equipment manufacturer's recommendation concerning exposure factors. Make the exposure.
- This procedure should be followed for the opposite side premolars.
Procedure for the Maxillary Molar Region
- Assemble the posterior receptor holding device and insert the receptor horizontally in the posterior biteblock. Use a type 2 receptor.
- Center the receptor on the molars (Figure 23). The receptor should be parallel with the long axis of the tooth (Figure 24). Position the receptor in the palate so that the entire tooth length will appear on the radiographic image with approximately a one-eighth inch border below the cuspal ridge. Align the anterior border of the receptor with the second premolar so that the image captured on the anterior edge of the receptor will be the distal third of the second premolar. Position the biteblock on the occlusal surfaces of the teeth to be radiographed. Proper positioning in this step will place the central ray of the x-ray beam between the molars.
- A cotton roll may be inserted between the mandibular teeth and the biteblock for patient comfort. Ask the patient to slowly, but firmly bite onto the block to maintain the correct position.
- Slide the aiming ring down the indicator rod; it should be as close to the skin as possible without actually touching the patient. Align the tube head close to the aiming ring, and center (Figure 25).
- Follow the receptor and equipment manufacturer's recommendation concerning exposure factors. Make the exposure.
- This procedure should be followed for the opposite side molars.
Procedure for the Mandibular Central/Lateral Incisors
- Assemble the anterior receptor holding device and insert the receptor vertically on the anterior biteblock. Use a type 1 receptor.
- Center the receptor on the mandibular central and lateral incisors (Figure 26). It may be necessary to displace the tongue distally and depress the receptor onto the floor of the mouth so that the entire tooth length will show with approximately a one-eighth inch border above the incisal edges. The receptor must be as posterior as the anatomy allows and the biteblock should be positioned on the edges of the incisors to be radiographed (Figure 27). Proper positioning in this step will place the central ray of the x-ray beam between the central and lateral incisors.
- A cotton roll may be inserted between the maxillary teeth and the biteblock for patient comfort. Ask the patient to slowly, but firmly bite onto the block to maintain the correct position. The receptor should be adjusted as the patient closes and the floor of the mouth relaxes.
- Slide the aiming ring down the indicator rod; it should be as close to the skin as possible without actually touching the patient. Align the tube head close to the aiming ring, and center (Figure 28).
- Follow the receptor and equipment manufacturer's recommendation concerning exposure factors. Make the exposure.
Procedure for the Mandibular Canines
- Assemble the anterior receptor holding device and insert the receptor vertically on the anterior biteblock. Use a type 1 receptor.
- Center the receptor on the mandibular canine (Figure 29). It may be necessary to displace the tongue distally and depress the receptor onto the floor of the mouth so that the entire tooth length will show with approximately a one-eighth inch border above the cuspal edge. The receptor must be as posterior as the anatomy allows and the biteblock should be positioned on the edges of the teeth to be radiographed (Figure 30). Proper positioning in this step will place the central ray of the x-ray beam at center of the canine.
- A cotton roll may be inserted between the maxillary teeth and the biteblock for patient comfort, especially if the patient has a shallow floor. Ask the patient to slowly, but firmly bite onto the block to maintain the correct position. The receptor should be adjusted as the patient closes and the floor of the mouth relaxes.
- Slide the aiming ring down the indicator rod; it should be as close to the skin as possible without actually touching the patient. Align the tube head close to the aiming ring, and center (Figure 31).
- Follow the receptor and equipment manufacturer's recommendation concerning exposure factors. Make the exposure.
- This procedure should be followed for the opposite side canine.
Procedure for the Mandibular Premolars
- Assemble the posterior receptor holding device and insert the receptor horizontally on the posterior biteblock. Use a type 2 receptor.
- Center the receptor on the premolars (Figure 32). The receptor should be parallel with the long axis of the tooth (Figure 33). The object-to-receptor distance in both the mandibular premolar and molar regions is minimal since the oral anatomy only allows the receptor to be positioned very close to the teeth and still remain parallel. Align the anterior border of the receptor with the canine so that the image captured on the anterior edge of the receptor will be the distal third of the canine. Position the biteblock on the occlusal surfaces of the teeth to be radiographed. Proper positioning in this step will place the central ray of the x-ray beam between the premolars.
- A cotton roll may be inserted between the maxillary teeth and the biteblock for patient comfort. Ask the patient to slowly, but firmly bite onto the block to maintain the correct position. The receptor should be adjusted as the patient closes and the floor of the mouth relaxes.
- Slide the aiming ring down the indicator rod; it should be as close to the skin as possible without actually touching the patient. Align the tube head close to the aiming ring, and center (Figure 34).
- Follow the receptor and equipment manufacturer's recommendation concerning exposure factors. Make the exposure.
- This procedure should be followed for the opposite side premolars.
Procedure for the Mandibular Molars
- Assemble the posterior receptor holding device and insert the receptor horizontally on the posterior biteblock. Use a type 2 receptor.
- Center the receptor on the molars (Figure 35). The receptor should be parallel with the long axis of the tooth (Figure 36). Depress the receptor onto the floor of the mouth so the entire length of the teeth will appear with approximately a one-eighth inch border above the occlusal surface. Align the anterior border of the receptor with the second premolar so that the image captured on the anterior edge of the receptor will be the distal third of the second premolar. Position the biteblock on the occlusal surfaces of the mandibular teeth. Proper positioning in this step will place the central ray of the x-ray beam between the molars, to catch the distal edge of the second premolar.
- A cotton roll may be inserted between the maxillary teeth and the biteblock for patient comfort. Ask the patient to slowly, but firmly bite onto the block to maintain the correct position. The receptor should be adjusted as the patient closes and the floor of the mouth relaxes.
- Slide the aiming ring down the indicator rod; it should be as close to the skin as possible without actually touching the patient. Align the tube head close to the aiming ring, and center (Figure 37).
- Follow the receptor and equipment manufacturer's recommendation concerning exposure factors. Make the exposure.
- This procedure should be followed for the opposite side molars.
Quiz
- What is the recommended patient positioning for examining the maxillary region using the paralleling technique?
- What is the recommended patient positioning for examining the mandibular region using the paralleling technique?
Answers
- When examining the maxillary region, the occlusal plane of the maxilla is parallel to the floor and the sagittal plane of the patient's head is perpendicular to the floor.
- When examining the mandibular region, the mandibular occlusal plane is parallel to the floor, when the mouth is open, and the sagittal plane of the patient's head is perpendicular to the floor.
The Bisecting Angle Technique
Basic Principles
The bisecting-the-angle or bisecting angle technique is based on the principle of aiming the central ray of the x-ray beam at right angles to an imaginary line which bisects the angle formed by the longitudinal axis of the tooth and the plane of the receptor. While it is not necessary to go into a long dissertation on plane geometry to understand this concept, a quick review will help make the technique more clear. To bisect is to divide a line or angle into two equal portions. A bisector is a plane or line that divides a line or angle into two equal portions. Figure 38 shows an equilateral triangle, with legs AB=BC=CA, and the angles ABC=60 degrees, CAB=60 degrees and BCA=60 degrees. We see in Figure 38 the following:
- The dotted line BD bisects the triangle, dividing it exactly in half. Thus, two equal triangles are formed from the original. Legs AB and BC were unchanged and thus are still equal.
- The original line CA was divided in half by D, and thus the lines AD and CD are equal.
- We know that the angle at point B was 60 degrees, and since it was bisected (divided equally), it now is 30 degrees at the intersections of AD and BD.
- We also know that bisecting the angle did not affect the angle at the old point A which was 60 degrees, and still is.
- The angle at the bisecting point DC must be 90 degrees because the sum of all the angles in any triangle is 180 degrees, and thus 180-(60+30)=90.
- Cyzynski's Rule of Isometry states that two triangles are equal when they share one complete side and have two equal angles. We can see that triangles ADB and BDC share the common side BD.
- We know further that the angles ADB and BDC are equal because D was defined as a bisector of the old angle ABC.
- Lastly, we know that the angles CAB and BCA were unchanged by bisecting and are still equal. Therefore, under Cyzynski's theorem, we can prove the triangles ABD and CBD are equal.
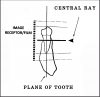
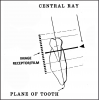
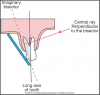
In dental radiography, the theorem is applied in the following manner. The receptor is positioned resting on the palate or on the floor of the mouth as close to the lingual tooth surfaces as possible. The plane of the receptor and the long (vertical) axis of the teeth to be radiographed form an angle with the apex at the point where the receptor contacts the teeth. The apex in Figure 39 is located at the point labeled B.
In Figure 39, the long axis through the tooth forms one leg of a triangle (AB), the plane of the receptor another leg (BC), both of which intersect at the apex, point B. A line representing the central x-ray beam will form the third leg of the triangle, AC. If an imaginary line bisected this axis-receptor- x-ray triangle, the bisector, DB, would form the common side of two equal triangles as defined by Cyzynski's theorem.
Since the sides formed by the tooth's long axis and the receptor are equal, the image cast onto the receptor would be the same length as the tooth or teeth casting that image. This linear equality is the basis for diagnostic quality bisecting angle radiographic images.
Anatomical Considerations
The bisecting angle technique is of value when the paralleling technique cannot be utilized. This may include patients with small mouths and those with low palatal vaults. Because of the increased exposure to radiation in this technique, it should only be employed when necessary.
Beam Angulation
The bisecting technique calls for varying beam angulations, depending on the region to be examined.
Horizontal angulation: The horizontal angulation of the tube head should be adjusted for each projection to position the central ray through the contacts in the region to be examined. This angulation will usually be at right angles to the buccal surfaces of the teeth to be radiographed.
Vertical angulation: In practice, the operator should position the central ray of the x-ray beam so that it is perpendicular to the imaginary line bisecting the angle formed between the tooth long axis and the receptor. This principle works well with flat, two dimensional structures, but teeth that have depth or are multirooted will produce distorted images. If the vertical angulation is excessive the image will appear foreshortened. Insufficient vertical angulation produces an elongated image.
The optimum angle will vary from patient to patient, but Table 1 serves as a general guideline for beam angulation.
Stabilizing the Receptor
Supporting the receptor with the patient's forefinger is not recommended. This method has several drawbacks. In addition to exposing the patient's digit to additional radiation, the patient may exert excessive force, thus bending the receptor and distorting the radiographic image. The receptor may slip without the operator's knowledge and produce a radiographic image outside the proper image field. Therefore, intraoral support is best accomplished using receptor holding devices that restrain the receptor and help align the beam properly.
Quiz
- On what principle is the bisecting angle technique based?
- How did this principle originate?
Answers
- The bisecting angle technique is based on the principle of aiming the central ray of the x-ray beam at right angles to an imaginary plane bisecting the angle formed by the longitudinal axis of the tooth and the plane of the receptor.
- The principle originated from Cyzynski's Rule of Isometry (Cyzynski's Theorem) which states that two triangles are equal when they share one complete side and have two equal angles.
Bisecting Angle Methodology
Patient Positioning
Maxillary region: For bisecting angle radiographic images of the maxilla, the patient should be positioned so that the maxillary occlusal plane is parallel to the floor and the sagittal plane of the patient's head is perpendicular to the floor.
Mandibular region: For bisecting angle radiographic images of the mandible, the patient should be positioned so that the mandibular occlusal plane is parallel to the floor and the sagittal plane of the patient's head is perpendicular to the floor.
Before any radiographic images are exposed, the patient must be draped with a protective apron and thyroid collar. The apron must be properly placed to avoid interference with the radiographic exposure.
Full Mouth Exposure
Procedure for the Maxillary Central/Lateral Incisors
- Assemble the anterior receptor holding device and insert the receptor vertically on the biteblock. Use a type 1 receptor.
- Center the receptor on the central/lateral incisors as close as possible to the lingual surfaces of the teeth with approximately a one-eighth inch border of the receptor extending below the incisal edge of the teeth (Figure 40). Position the biteblock on the incisal edges of the teeth to be radiographed (Figure 41).
- A cotton roll may be inserted between the mandibular teeth and the biteblock for patient comfort. Ask the patient to slowly, but firmly bite onto the block to maintain the correct position.
- Align the central ray perpendicular to the bisector vertically and at the desired interproximal contact to be viewed. Horizontally, the central ray should bisect the central/lateral (Figure 42). For maxillary exposures the tube head will be pointed down for positive (+) angulation.
- Follow the receptor and equipment manufacturer's recommendation concerning exposure factors. Make the exposure.
- This procedure should be followed for the opposite side maxillary central/lateral incisors if needed.
Procedure for the Maxillary Canines
- Assemble the anterior receptor holding device and insert the receptor vertically on the biteblock. Use a type 1 receptor.
- Center the receptor on the canine as close as possible to the lingual surfaces of the teeth with approximately a one-eighth inch border of the receptor extending below the incisal edge of the teeth (Figure 43). Position the biteblock on the incisal edges of the teeth to be radiographed. (Figure 44).
- A cotton roll may be inserted between the mandibular teeth and the biteblock for patient comfort. Ask the patient to slowly, but firmly bite onto the block to maintain the correct position.
- Align the central ray perpendicular to the bisector vertically and at the desired interproximal contact to be viewed. Horizontally, the central ray should bisect the canine (Figure 45). For maxillary exposures the tube head will be pointed down for positive (+) angulation.
- Follow the receptor and equipment manufacturer's recommendation concerning exposure factors. Make the exposure.
- This procedure should be followed for the opposite side maxillary canine.
Procedure for the Maxillary Premolars
- Assemble the posterior receptor holding device and insert the receptor horizontally on the biteblock. Use a type 2 receptor.
- Center the receptor on the premolars as close as possible to the lingual surfaces of the teeth (Figure 46). Position the receptor in the palate so that the entire tooth length will appear on the radiographic image with approximately a one-eighth inch border below the cuspal ridge. Align the anterior border of the receptor with the canine so that the image captured on the anterior edge of the receptor will be the distal third of the canine. Position the biteblock on the occlusal surface of the teeth being radiographed (Figure 47).
- A cotton roll may be inserted between the mandibular teeth and the biteblock for patient comfort. Ask the patient to slowly, but firmly bite onto the block to maintain the correct position. (Watch the occlusal border of the receptor; it tends to slip down anteriorly.)
- Align the central ray perpendicular to the bisector vertically and at the desired interproximal contact to be viewed. Horizontally, the central ray should pass between the contact of the first and second premolar (Figure 48). For maxillary exposures the tube head will be pointed down for positive (+) angulation.
- Follow the receptor and equipment manufacturer's recommendation concerning exposure factors. Make the exposure.
- This procedure should be followed for the opposite side maxillary premolars.
Procedure for the Maxillary Molars
- Assemble the posterior receptor holding device and insert the receptor horizontally on the biteblock. Use a type 2 receptor.
- Center the receptor on the molars as close as possible to the lingual surfaces of the teeth (Figure 49). Position the receptor in the palate so that the entire tooth length will appear on the radiographic image with approximately a one-eighth inch border below the cuspal ridge. Align the anterior border of the receptor with the second premolar so that the image captured on the anterior edge of the radiographic image is the distal third of the second premolar. Position the biteblock on the occlusal surface of the teeth being radiographed (Figure 50).
- A cotton roll may be inserted between the mandibular teeth and the biteblock for patient comfort. Ask the patient to slowly, but firmly bite onto the block to maintain the correct position.
- Align the central ray perpendicular to the bisector vertically and at the desired interproximal contact to be viewed. Horizontally, the central ray should pass between the contact of the first and second molar (Figure 51). For maxillary exposures the tube head will be pointed down for positive (+) angulation.
- Follow the receptor and equipment manufacturer's recommendation concerning exposure factors. Make the exposure.
- This procedure should be followed for the opposite side maxillary molars.
Procedure for the Mandibular Central/Lateral Incisors
- Assemble the anterior receptor holding device and insert the receptor vertically on the biteblock. Use a type 1 receptor.
- Center the receptor on the central/lateral incisors as close as possible to the lingual surfaces of the teeth with approximately a one-eighth inch border of the receptor extending above the incisal edge of the teeth. Position the biteblock on the incisal edges of the teeth to be radiographed (Figure 52).
- A cotton roll may be inserted between the maxillary incisors and the biteblock for patient comfort. Ask the patient to slowly, but firmly bite onto the block to maintain the correct position. The receptor should be straightened as the patient closes and the floor of the mouth relaxes.
- Align the central ray perpendicular to the bisector vertically and at the desired interproximal contact to be viewed. Horizontally, the central ray should pass between the central/lateral incisors (Figure 53). For mandibular exposures the tube head will be pointed up for negative (-) angulation.
- Follow the receptor and equipment manufacturer's recommendation concerning exposure factors. Make the exposure.
Procedure for the Mandibular Canines
- Assemble the anterior receptor holding device and insert the receptor vertically on the biteblock. Use a type 1 receptor.
- Center the receptor on the canine as close as possible to the lingual surfaces of the teeth with approximately a one-eighth inch border of the receptor extending above the incisal edge of the canine. Position the biteblock on the incisal edges of the teeth to be radiographed (Figure 54).
- A cotton roll may be inserted between the maxillary teeth and the biteblock for patient comfort. Ask the patient to slowly, but firmly bite onto the block to maintain the correct position. The receptor should be straightened as the patient closes and the floor of the mouth relaxes.
- Align the central ray perpendicular to the bisector vertically and at the desired interproximal contact to be viewed. Horizontally, the central ray should bisect the canine (Figure 55). For mandibular exposures the tube head will be pointed up for negative (-) angulation.
- Follow the receptor and equipment manufacturer's recommendation concerning exposure factors. Make the exposure.
- This procedure should be followed for the opposite side mandibular canine.
Procedure for the Mandibular Premolars
- Assemble the posterior receptor holding device and insert the receptor horizontally on the biteblock. Use a type 2 receptor.
- Center the receptor on the premolars as close as possible to the lingual surfaces of the teeth. Align the anterior border of the receptor with the canine so that the image captured on the anterior edge of the receptor will be the distal third of the canine. Position the biteblock on the occlusal surface of the teeth to be radiographed (Figure 56).
- A cotton roll may be inserted between the maxillary premolars and the biteblock for patient comfort. Ask the patient to slowly, but firmly bite onto the block to maintain the correct position. The receptor should be straightened as the patient closes and the floor of the mouth relaxes.
- Align the central ray perpendicular to the bisector vertically and at the desired interproximal contact to be viewed. Horizontally, the central ray should pass between the first and second premolars (Figure 57). For mandibular exposures the tube head will be pointed up for negative (-) angulation.
- Follow the receptor and equipment manufacturer's recommendation concerning exposure factors. Make the exposure.
- This procedure should be followed for the opposite side mandibular premolars.
Procedure for the Mandibular Molars
- Assemble the posterior receptor holding device and insert the receptor horizontally on the biteblock. Use a type 2 receptor.
- Center the receptor on the molars as close as possible to the lingual surfaces of the teeth. Align the anterior border of the receptor with the second premolar so that the image captured on the anterior edge of the receptor will be the distal third of the second premolar. Position the biteblock on the occlusal surface of the teeth to be radiographed (Figure 58).
- A cotton roll may be inserted between the maxillary molars and the biteblock for patient comfort. Ask the patient to slowly, but firmly bite onto the block to maintain the correct position. The receptor should be straightened as the patient closes and the floor of the mouth relaxes.
- Align the central ray perpendicular to the bisector vertically and at the desired interproximal contact to be viewed. Horizontally, the central ray should pass between the contact of the first and second molar (Figure 59). For mandibular exposures the tube head will be pointed up for negative (-) angulation.
- Follow the receptor and equipment manufacturer's recommendation concerning exposure factors. Make the exposure.
- This procedure should be followed for the opposite side mandibular molars.
Bitewing Radiography
Bitewing radiographic images are of particular value in detecting interproximal caries in the early stages of development, before it is clinically visible. For this reason, it is critical that horizontal angulation be accurately projected following the direction of the interproximal contacts and no overlapping contacts are present on the radiographic image. Bitewing radiographic images are also useful in evaluation of the alveolar crests for detection of early periodontal disease.
Basic Principles
Bitewing images are parallel images because the receptor is positioned parallel to the long axis of the teeth and the beam is perpendicular to the receptor as in Figure 60. A bitewing tab is utilized to stabilize the receptor as the patient bites together.
Beam Angulation and Receptor Holding Devices
Bitewing radiographic images are usually exposed with an indicated vertical angulation of +10 degrees (tube head points down for positive (+) angulation). This angulation provides an acceptable compromise for the differences between the long axis inclinations of the maxillary and mandibular teeth. Horizontal angulation is aligned with the direction of the contact, and the central ray is directed between the contacts of the teeth to be radiographed. Horizontal angulation is achieved when the central ray of the x-ray beam is directed specifically between the contacts of the teeth to be radiographed.
The interproximal examination may be done using a special type 3 bitewing receptor but is preferably achieved by using four type 2 receptors fitted with a tab. There are also receptor holding devices available that support the receptor as well as provide an external reference for positioning the tube head. The patient stabilizes the receptor by gently biting together on the manufactured tab or on the holding device.
Tube head position is illustrated in Figure 62, and a sample set of bitewing radiographic images is illustrated in Figure 63.
Before any radiographic images are exposed, the patient must be draped with a protective apron and thyroid collar. The apron must be properly placed to avoid interference with the radiographic exposure.
Quiz
- What is the main purpose for taking bitewing radiographic images?
- Why are bitewings exposed with a vertical angulation of +10 degrees?
Answers
- The main purpose for taking bitewing radiographic images is to detect interproximal caries.
- Bitewings are exposed with a +10 angulation to compromise for the differences in the long axis angulations of the maxillary and mandibular teeth.
Intraoral Occlusal Radiography
Maxillary Topographical Occlusal
Figure 64 shows the palate (roof of the mouth), zygomatic process of the maxilla (a projection from the maxilla), antero-inferior aspects of each antrum (in this case, the maxillary sinuses), nasolacrimal canals (tear ducts), teeth from the left second molars to the central incisors, and the nasal septum (cartilage dividing the nose).
Uses: To view the maxilla for anterior alveolar fractures, cysts, supernumerary teeth and impacted canines, and to view pathology at the apices of the incisors. It is not used to diagnose periodontal conditions.
Patient positioning: The patient is seated with the sagittal plane perpendicular to the floor and the occlusal plane parallel to the floor. Before any radiographic images are exposed, the patient must be draped with a protective apron and thyroid collar. The apron must be properly placed to avoid interference with the radiographic exposure.
Receptor placement: Use a type 4 receptor. With the tube side of the receptor toward the maxilla, the receptor is placed crosswise in the mouth, like a cracker. It is gently pushed backwards until it contacts the anterior border of the mandibular ramus. The patient bites down gently to maintain position.
Exposure factors: Follow the recommendations of the receptor and equipment manufacturer.
Direction of the central ray: The central ray is directed at the center of the receptor with a vertical angulation of +65 degrees and a horizontal angulation of 0 degrees. In this case, the central ray will pass through the bridge of the nose, as in Figure 65.
Mandibular Topographical Occlusal
Uses: To view the anterior portion of the mandible for fractures, cysts, root tips, and periapical pathology. It provides a very good view of the symphysis region of the mandible as seen in Figure 66.
Patient positioning: The patient is seated with the head tilting slightly backward, so that the occlusal plane (ala-tragus line) is 45 degrees above the horizontal plane. Before any radiographs are exposed, the patient must be draped with a protective apron and thyroid collar. The apron must be properly placed to avoid interference with the radiographic exposure.
Receptor placement: Use a type 4 receptor. With the tube side of the receptor toward the mandible, the receptor is placed crosswise in the mouth, like a cracker. It is gently pushed backwards until it contacts the anterior border of the mandibular ramus. The patient bites down gently to maintain position.
Exposure factors: Follow the recommendations of the receptor and equipment manufacturer.
Direction of the central ray: The central ray is directed between the apices of the mandibular central incisors and the tube is angled at -55 degrees relative to the receptor plane, as in Figure 67.
Maxillary Vertex Occlusal
Uses: To view the buccopalatal relationships of unerupted teeth in the dental arch (Figure 68).
Patient positioning: The patient is seated with the sagittal plane perpendicular to the floor and the occlusal plane parallel to the floor. Before any images are exposed, the patient must be draped with a protective apron and thyroid collar. The apron must be properly placed to avoid interference with the radiographic exposure.
Receptor placement: Use a type 4 receptor. The receptor is placed in the same manner as the Maxillary Topographical Occlusal.
Exposure factors: Follow the recommendations of the receptor and equipment manufacturer.
Direction of the central ray: The central ray is directed through the top of the skull (hence the name vertex occlusal). Since the beam must penetrate a considerable amount of bone and soft tissue, the exposure time must be increased. The central ray is perpendicular to the receptor plane and is directed to the center of the receptor as in Figure 69.
Mandibular Cross-Sectional Occlusal
Uses: To view the entire mandible for fractures, foreign bodies, root tips, salivary calculi, tori, etc. (Figure 70).
Patient positioning: The patient's head may be in any comfortable position that allows the central ray to be directed perpendicular to the plane of the receptor. Before any radiographic images are exposed, the patient must be draped with a protective apron and thyroid collar. The apron must be properly placed to avoid interference with the radiographic exposure.
Receptor placement: Use a type 4 receptor. The receptor is placed in the same manner as the Mandibular Topographical Occlusal.
Exposure factors: Follow the recommendations of the receptor and equipment manufacturer.
Direction of the central ray: The central ray is perpendicular to the receptor plane and is directed to the center of the receptor as in Figure 71.
Posterior Oblique Maxillary Occlusal
Uses: To view the maxillary posterior region and provide a topographical view of the maxillary sinus. The projection may be used in place of periapical images in patients who have a tendency to gag and for examining periapical pathology and root tips (Figure 72).
Patient positioning: The patient is seated with the occlusal plane parallel to the floor and the sagittal plane perpendicular to the floor. Before any radiographic images are exposed, the patient must be draped with a protective apron and thyroid collar. The apron must be properly placed to avoid interference with the radiographic exposure.
Receptor placement: Use a type 4 receptor. The receptor plane should be parallel to the floor, and the receptor should be pushed posteriorly as far as possible. The lateral border of the receptor should be positioned parallel to the buccal surfaces of the posterior teeth and extend laterally approximately one-half inch past the buccal cusps on the side of interest. The patient should bite down gently to maintain the correct position.
Exposure factors: Follow the recommendations of the receptor and equipment manufacturer.
Direction of the central ray: The tube is directed at an angle of +60 degrees. Horizontal angulation should be such that the central ray is approximately at right angles to the curve of the arch and strikes the center of the receptor as in Figure 73.
Posterior Oblique Mandibular Occlusal
Uses: The projection is used to view the posterior teeth of the mandible to locate cysts, fractures, supernumerary teeth, and periapical pathology. It can be used in place of posterior periapical radiographic images (Figure 74).
Patient positioning: The patient is seated with the occlusal plane parallel to the floor and the sagittal plane perpendicular to the floor. Before any radiographic images are exposed, the patient must be draped with a protective apron and thyroid collar. The apron must be properly placed to avoid interference with the radiographic exposure.
Receptor placement: Use a type 4 receptor. The receptor plane should be parallel to the floor, and the receptor should be pushed posteriorly as far as possible. The lateral border of the receptor should be positioned parallel to the buccal surfaces of the posterior teeth and extend laterally approximately one-half inch past the buccal cusps on the side of interest. The patient should bite down gently to maintain the correct position.
Exposure factors: Follow the recommendations of the receptor and equipment manufacturer.
Direction of the central ray: The tube is directed at the apex of the mandibular second premolar, and the central ray should strike the center of the receptor. The vertical angulation is -50 degrees as in Figure 75.
Modified Oblique Posterior Mandibular Occlusal
Uses: This projection is especially useful to detect calculi in the submandibular gland. Calculi are often difficult to detect on conventional radiographic images due to superimposition of the mandibular bone (Figure 76).
Patient positioning and receptor placement: Use a type 4 receptor. With the tube side of the receptor toward the mandible, the receptor is placed in the patient's mouth crosswise like a cracker. The receptor plane should be parallel to the floor, and the receptor should be pushed posteriorly as far as possible. The lateral border of the receptor should be positioned parallel to the buccal surfaces of the posterior teeth and extend laterally approximately one-half inch past the buccal cusps on the side of interest. The patient's head is then rotated to the side and lifted up. Before any radiographic images are exposed, the patient must be draped with a protective apron and thyroid collar. The apron must be properly placed to avoid interference with the radiographic exposure.
Exposure factors: Follow the recommendations of the receptor and equipment manufacturer.
Direction of the central ray: The tube is positioned under and behind the mandible and the central ray is directed onto the center of the receptor so that it passes inside the ascending ramus so that the submandibular gland will be between the tube and the receptor as in Figure 77.
Digital Radiology
Digital imaging was introduced into dentistry in 1987. Digital sensors are used instead of film receptors. Sensors can be wired or wireless depending on the system used (Figure 78). Sensors and tube head placement are the same for digital imaging as film and tube head placement is for traditional radiology. Most standard radiographic machines can be converted to acquire digital images. Digital imaging still uses ionizing radiation, and until recently it was believed that before any digital radiographic images are exposed, the patient must be draped with a protective apron and thyroid collar. The National Council on Radiation Protection & Measurement (NCRP) published new guidelines for the use of protective aprons and digital imaging. The new guidelines state that if an office only uses digital solid-state image receptors, protective aprons are only required when the patient is pregnant or could be pregnant. Protective thyroid collars are mandatory on pediatric patients. These protective devices should be placed on the patient in a way that will not interfere with the image.
The sensors are slightly thicker than a regular receptor. Modified receptor holding devices must be utilized in the placement of the sensors. These modified holders can be purchased from any major dental supply company. The sensors can be reused many times. Proper use of intraoral barrier and OSHA infection control techniques must be observed.
The advantages of digital radiology are decreased exposure time to the patient, elimination of darkroom processing time and exposure to processing chemicals. Digital imaging has environmental advantages with reduced waste production and also paper and receptor film consumption. Immediate viewing and ability to easily and cost effectively transmit directly to third party facilities or affiliating dental offices are added advantages.
Additional computerized advantages include the ability to enhance the image for viewing. Once an image is in the computer, brightness, contrast, and image reversal can be enhanced for optimal viewing of tissue and bone levels. The radiographic image can be rotated, enlarged, and magnified to enhance details for diagnosis and patient education. An additional feature shows embossed images creating a stacked effect of the oral tissues.
When an integrated system incorporates digital images with patient record management, efficiency and access is increased. Files and radiographic images are stored within the computer system and retrieved easily.
The main disadvantages are substantial start-up costs including machinery, operatory computer technology, and RAM capacity. Considerations must also be noted that although your office may utilize digital radiography, other facilities may not and the transfer of images between them could be more difficult.
The digital sensors are considered a disadvantage by some operators as they are thicker than traditional receptors/films and more difficult to orient in the oral cavity. When a patient cannot bite correctly on the receptor holders, the operator may have to use the bisecting technique. Using the paralleling technique with sensors may enable the operator to capture the apices of a tooth. The bisecting technique will help orient the receptors correctly, therefore allowing the operator to capture all of the images needed. Each patient will be different and the operator should pay close attention to the size of the patient’s mouth in order to correctly capture all of the images digitally. Using digital receptors may take the operator some time to adjust to the new techniques, however using both the Paralleling and Bisecting techniques the operator will provide the office with the images needed for proper diagnosis of the oral cavity. Remember, sensors cannot be sterilized and must be protected by a barrier before handling and placement. The operator should check with the manufacturer on how to properly place the barrier for maximum usage and patient comfort.
Summary
As technology advances in dental radiology, operators must maintain current knowledge and adapt their skills for the best treatment of the patient. Periapical, bitewing, and occlusal surveys are critical components of diagnosis and treatment of dental patients. Because of the exposure to ionizing radiation, proper techniques must be employed to reduce radiation exposure to the patient through the use of protective aprons, digital radiology, high speed films, and proper technique; thus, decreasing radiographic retakes and additional exposure. Dental radiographers must be familiar with different receptor holding devices that can be utilized for patient comfort. Digital imaging remains similar in technique, but some adaptations are required for optimum sensor placement. Proper infection control protocol, receptor, and tube head placement are all critical components of the total radiographic procedure.
Glossary
alveolar crest - highest part of the alveolar bone
alveolar ridge - part of the bone that contains the tooth sockets
anterior - in front
apices - plural for apex or tip of root
bisector - a straight line that bisects an angle
buccal - towards the cheek
calculi - plural of calculus; a hard, rough deposit on the tooth surface
digit - finger or toe
distal - tooth surface away from the midline
edentulous - without teeth
foramina - plural for foramen; an opening
horizontal - line extending from side to side
impacted - trapped below the surface as in an impacted third molar
incisal edge - biting surface of front teeth
interproximal - between the teeth
intraoral - inside the oral cavity
lingually - towards the tongue
long axis - imaginary plane that vertically divides the tooth into two equal halves
mandible - lower jaw
mandibular ramus - portion of the mandible that extends back and up
maxilla - upper jaw
mesial - tooth surface towards the midline
occlusal - biting surface of back teeth
palatal - pertaining to the roof of the mouth
parallel - extending in the same direction and same distance apart; never intersecting
periapical - surrounding the apex or tip of the tooth
periodontal - surrounding the tooth
periodontal disease - disease of the gums and supporting areas of the teeth
perpendicular - intersecting at a right angle
PID - position indicating device
posteriorly - behind
receptor/image receptor - the device used to capture the information
sagittal plane - vertical plane dividing the body
supernumerary teeth - extra teeth
tori - hard bony projections
vertical - line extending from top to bottom (up and down)
XCP - extended cone paralleling; type of radiographic image holder
ABOUT THE AUTHORS
Radiology Series editor:
ALLAN G. FARMAN, BDS, EDS, MBA, PHD
Dr. Farman is an oral and maxillofacial radiologist and is a professor of radiology and imaging science, Department of Surgical and Hospital Dentistry, at the University of Louisville. He serves as the ADA representative to the DICOM Standards Committee and 2009-2010 President of the American Academy of Oral and Maxillofacial Radiology (AAOMR).
ADAA COUNCIL ON EDUCATION
Members of the ADAA Council on Education reviewed this course. Their recommendations were researched, and updates were made accordingly. All members of the Council on Education are ADAA Active or Life Members with an interest in dental assisting education. Each one volunteers their time to the life-long learning of dental assistants.
References
Bird, CDA, RDH, MA, D.L., & Robinson, CDA, MS, D.S. (2014). Modern dental assisting. (11th ed.). St. Louis, MO: Mosby Elsevier.
Centers for Disease Control and Prevention, (2003). Guidelines for infection control in dental health-care settings (MMWR 52(RR17)). Retrieved from U.S. Government Printing Office website: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5217a1.htm
Iannucci, DDS, MA, J.M., & Howerton, L.J. (2012). Dental radiography: Principles and techniques. (4th ed.). St. Louis, MO: Mosby Elsevier.
Miles, BA, DDS, MS, FRCD(C), Dip. ABOMR, Dip. ABOM, D.A., Govoni, CDA, RDA, RDH, MBA, M., Metivier, BS, A.P., & Phinney, CDA, M.Ed., FADAA, D.J. (2013). An introduction to basic concepts in dental radiography. American Dental Assistants Association, Retrieved from www.dentalassistant.org