You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Clinicians often ponder how to be conservative with endodontic therapy and concurrently treat a patient with a sick tooth in a predictable, time-efficient manner that will give the patient confidence that the root canal being recommended will be in function for many years to come. With all the endodontic systems dentists have to choose from, which system works best for the individual? This article will aid the decision-making process the clinician undertakes when choosing a particular endodontic therapy, protocol, and system for a practice.
Clinicians must do their best to make procedures successful. They must be confident that the system and technique being used are appropriate. After the work has been completed, they must be confident that the endodontic therapy was simple, safe, and sophisticated, without separated instruments.
The cases presented in this article will assist the clinician in understanding and appreciating the engineering efforts of companies such as Dentsply Sirona, Komet-USA, and Sonendo in the development of nickel-titanium (NiTi) rotary endodontic-file systems. The article will describe the steps for completing most endodontic therapies using three endodontic files for primary endodontic lesions with secondary periodontal effects. It also will describe restorative techniques using a prefabricated, tapered-root post made of glass fiber embedded in epoxy resin.
Considerations for the clinician in making the decision to use rotary instrumentation are resistance to file separation, maintaining as much dentin as possible within the glide path, and efficient cutting of the dentin. The technique involves fewer files within the procedure, less crown-down technique, and simplification of initial shaping. The entire process can be accomplished with fewer files to develop the ideal shaping of the canal.
Should the clinician use hand files or rotary files? To answer that question, the clinician should know the long-term goal of the endodontic therapy and estimate how stable the tooth will be in consideration of the long-term restoration.
The best endodontic therapy is often found when the coronal, middle, and apical regions of the canal are properly shaped. After the determination of working length, variably tapered shaping files .02, .04 and .06 can ensure this result is achieved. One must also consider not only ideal shaping but creating the appropriate apical stop to avoid overfilling. After the apical foramen is widened excessively, it is almost impossible to successfully seal the canal(s). The apical preparation that is most forgiving is the one that is tapered. This apical shaping objective not only is more predictable with variably tapered shaping files, it requires fewer instruments to achieve the result.1 The reason to create shape is to allow irrigants to reach all the apical and lateral extents of a root so the bacteria can be killed. Irrigants such as ethylene-diamine-tetra-acetic acid (EDTA) can remove the smear layer created during shaping; full-strength sodium hypochlorite (NaOCl) can be used for at least 30 minutes in necrotic pulp and 45 minutes for vital cases.2,3
The files used in the cases described below were designed with extremely sharp angles for cutting efficiency. The use of such files decreased the time the file would remain in the canal and effectively removed infected debris from the canal(s). Less time in the canal(s) resulted in less separation of instruments and a more productive and profitable appointment. The file system used was very flexible, allowing it to more easily adapt to the morphology of the canal, including molars with severely curved canals. The cases reviewed and evaluated in this article were all completed using rubber-dam isolation for optimum electronic apex location, debridement, irrigation, and final obturation.
Case One: Right Maxillary Canine (No. 6)
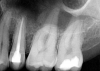
A patient presented with acute pain and facial swelling. Tooth No. 6 was positive to percussion, without sensitivity to air, sweets, or temperature stimulus. Treatment options were discussed with the patient. The decision was to complete endodontic therapy to eliminate the pain (Figure 1). Definitive long-term final-restoration treatment options were presented using a fiber post and core with full-coverage CAD/CAM crown.
Step 1. Access and Enlarge Coronal Portion of Canal
The canine was accessed from the lingual with a high-speed diamond #6 round bur, ensuring a straight-line visual access to the canal. The coronal portion of the canal was opened with an opener bur that eliminated the need for two burs.
Step 2. Prepare Glide Path
A smooth glide path was developed with a #15 K-file. Working length was verified with an apex locator to 29 mm.
Step 3. Use 025 File (.04 Taper)
The canal was shaped with a 025 rotary file (.04 taper) with a water-soluble gel to the 29-mm working length. The handpiece was set for 1.80-Ncm torque value and at 300 rpm. The author has found that when the rpm value is increased to expedite the negotiation of the canal, considerable amounts of time are spent trying to remove the separated file. The clinician should stay below the 350-rpm value and maintain 1.8-Ncm torque. This philosophy tends to improve the shaping of the canal(s) and the likelihood for successful therapy.
Step 4. Use 035 File for Final Preparation
The canal was prepared with an 035 (.04 taper) NiTi rotary file to the 29-mm working length with large amounts of water-soluble gel (Figure 2). The rotary files were supplied in lengths of 21 mm, 25 mm, and 31 mm. The system provided matching paper points and gutta-percha in all file sizes. Irrigation took place with NaOCl before the solution was allowed to remain in the canals for 30 minutes. After the irrigation, CO2 laser technology was used for 20 seconds to eliminate bacterial and viral contaminants. The laser evaporated any residual bacteria or viruses that remained after irrigation. The laser was an effective modality for root-canal sterilization.4
Case Two: Maxillary Left Second Bicuspid (No. 13)
The patient presented with temperature sensitivity and pain during mastication (Figure 3). Local anesthesia was delivered, and steps 1 through 4 were performed.
Step 1. Access and Enlarge Coronal Portion of Canal
A high-speed diamond #6 round bur was used for visual access, followed by the opener to enlarge the coronal portion of the bicuspid.
Step 2. Prepare Glide Path
A #15 file was used to establish a glide path. Verification of the working length of 20 mm was performed with an apex locator.
Step 3. Use 025 File (.04 Taper)
A 025 file (.04 taper) was used with a pecking motion and lubrication to the canal to the 20-mm working length.
Step 4. Use 035 File for Final Preparation
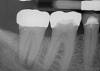
The 035 final file was used to the 20-mm working length with lubrication. The canal was irrigated with NaCl for 30 minutes, 035 dry points were used, and the root-canal sterilization was performed with the CO2 laser. Then the final fill was completed with the matching 035 gutta-percha and root-canal sealer (Figure 4).
Case Three: Left Maxillary First Molar (No. 14)
A patient had been seen for caries control and replacement of deteriorating amalgam restorations. Two weeks postoperatively, the patient was unable to tolerate hot or cold temperatures and was unable to chew any type of food (Figure 5). The patient accepted endodontic therapy, post and core, and full-crown coverage at a later date. The principles of the rotary-file system were used again.
Step 1. Access and Enlarge Coronal Portion of Canal
A radiograph, local anesthetic, and digital working-length measurement were completed. The access opening was performed, and then coronal enlargement of the canal took place. This process eliminated using burs #2 and #3.
Step 2. Prepare Glide Path
A#15 K-file was used to develop a smooth glide path. Working length was verified with an electronic apex locator to 21 mm for the mesiobuccal and distobuccal canals and 23 mm for the palatal canal.
Step 3. Use 025 File (.04 Taper)
The 025 (.04 taper) NiTi file was used with lubrication to the established and verified working lengths. While using the files, the clinician should remember to use a pecking motion. The clinician should resist the temptation to accelerate the rpm and torque value. The settings on the handpiece should remain at no greater than 350 rpm and 1.8 torque value. This will help prevent the likelihood of a file separation into the canal.
Step 4. Use 035 File for Final Preparation
Final file instrumentation of the 035 (.04 taper) was used with large amounts of a water-soluble gel to the established working lengths. NaCl irrigation was implemented and allowed to sit for 30 minutes in the canals, and then matching paper points were used to dry the canals. A CO2 laser was used to sterilize the canals. The final obturation was completed with the matching gutta-percha and root-canal sealer (Figure 6).
Treating and Restoring Primary Endodontic and Periodontal Lesions
Questions are raised frequently on presentation of affected pulpal tissue and the surrounding periodontium regarding diagnosis, prognosis, and treatment. Pulpal infection can drain through the periodontal ligament space and give an appearance of periodontal destruction, termed retrograde periodontitis.5 In comparison, both pulpal and periodontal infections can coexist in the same tooth-combined lesions, where the treatment depends on the degree of involvement of the affected tissues. Both endodontic and periodontal diseases are caused by a mixed anaerobic infection.6
Treatment of combined endodontic and periodontal lesions does not differ from the treatment of either an endodontic lesion or a periodontal lesion. The part of the lesion sustained by the root-canal infection can usually be expected to resolve after proper endodontic treatment. Timing of the completion of the root-canal therapy, medicaments used, and assessment of restorability are considerations for the long-term success and survival of the tooth.7 Figures 7, 8, and 9 represent the timing of completion and restorative decision-making to complete all therapies.
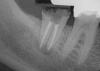
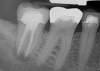
In Figure 7, the periapical radiograph identifies the presence of the combined endodontic-periodontal lesion developing due to a carious lesion beneath an existing vintage gold crown with ill-fitting margins. Intraoral examination revealed a fistula developing and moderate pain on percussion and mastication. After occlusal access and clear visualization of the canals, the canals were shaped using the rotary files, with precautions taken not to perforate or enlarge the apical foramen. Maintaining the endodontic therapy within the canals prevents the infection from being introduced into the surrounding periodontium. In this case, calcium hydroxide medicament was placed into the canals and evaluated 30 days postoperatively.8
The patient returned for final evaluation of the provisional calcium-hydroxide endodontic therapy and resolution of the infection (33 days postoperatively). Fistula was not present; the tooth was not sensitive to percussion or mastication. The gold crown was removed using a high-speed metal cutting bur, the remaining caries were excavated conservatively, and the endodontic therapy was completed. Placement of glass-fiber reinforced composite and composite core buildup took place. The natural tooth structure to receive the glass-fiber post and a long-term restoration was available (Figure 8). Within one appointment, the tooth was restored (Figure 9). The patient was instructed to return for clinical and radiographic evaluation after 6 to 12 months to determine progression of periodontal healing. At that time, if the healing were adequate and the tooth were stable, evaluation of the tooth would be considered every 3 to 4 years.7
Glass-Fiber Post Principles
After endodontic therapy, how the tooth is to be restored and what demands will be placed on the tooth must be considered. Often patients present with teeth that require endodontic therapy; however, the restorative load in the case of an abutment for a fixed partial denture or a supporting tooth for a removable prosthesis may exceed the tooth's ability to support such restorative options. Careful evaluation of remaining volume and surface area of dentin after excavation and endodontic therapy is critical.
Cast posts, stainless steel, titanium, and glass-fiber posts have been available for many decades. Fiber posts have been available since the 1990s for the restoration of endodontically treated teeth.9 They are available in several sizes, shapes, and compositions. Glass-fiber posts are similar in modulus of elasticity to natural dentin tooth structure.10
When forces are placed during mastication, deformation of the post is in the same proportion as the natural tooth. The opposite happens with metal posts. Metal posts are more rigid and create an increased stress on the root, causing a much higher number of root fractures that are catastrophic. Indications for using fiber-post placement are having more than 2 mm of coronal healthy dentin in height and thickness (measured from bony crest, mesiodistally, and buccolingually).9
Proper sizing of the fiber post and cementation considerations are as follows. Resin cements have improved mechanical properties to zinc phosphate and glass-ionomers. Resin cements that are dual-cure or self-cure are better options for cementation of endodontic posts.11 This article presented a self-cure resin-cement option. Approximately 4 minutes after glass-fiber post cementation, core buildup can be performed. The appropriate resin material for core buildup should be not only for the reconstruction, but also for consideration of the final long-term restoration. The purpose of the post is to retain the core, which in turn helps retain the crown.12 This suggests that a more flexible post will not by itself reduce the clinical root fractures and failures. Sound clinical decision-making is the key to reducing clinical failures.
Conclusion
Root canals are the everyday dentistry that many clinicians see routinely. About 80% of the root-canal therapies in a dental practice can be completed with two to three rotary files after access opening for straight-line visualization and coronal enlargement. Rotary-file endodontic systems and glass-fiber posts can save time for patients and are valuable for dental practices that offer endodontic therapy and restorative dentistry.
A manageable rotary-file sequence using two to three files reduces the time requirements for properly shaping canals conservatively; working lengths to the apical constriction without perforation or enlargement of the foramen (apical shaping length .05 mm to 1.0 mm short of the foramen) are the goal for increasing endodontic success rates. Because endodontic therapy is an internal technique, clinicians must be able to adequately remove soft tissues (necrotic or vital) and properly shape and seal the canals to arrest the advancement of disease. The ensuing challenge after endodontic completion is to appropriately choose the restorative post-and-core assembly and the final long-term restoration. The challenges that occur daily in practice can be met with new technologies and materials, thereby creating the move from long-term "survival" statistics to a platform in the realm of "success" statistics and long-term life of endodontically treated and restored teeth.
About the Author
Thomas M. Bilski, DDS
Private Practice
Independence, Ohio
References
1. Schilder H. Cleaning and shaping the root canal. Dent Clin North Am. 1974;18(2):269-296.
2. Ram Z. Effectiveness of root canal irrigation. Oral Surg Oral Med Oral Pathol. 1977;44(2):306-312.
3. Singh N, Chandra A, Tikku AP, Verma P. A comparative evaluation of different irrigation activation systems on smear layer removal from root canal: an in-vitro scanning electron microscope study. J Conserv Dent. 2014;17(2):159-163.
4. Asnaashari M, Safavi J. Disinfection of contaminated canals by different laser wavelengths, while performing root canal therapy. J Lasers Med Sci. 2013;4(1): 8-16.
5. Jansson L, Ehnevid H, Lindskog S, Blomlöf L. The influence of endodontic infection on progression of marginal bone loss in periodontitis. J Clin Periodontol. 1995;22(10):729-734.
6. Jansson L, Ehnevid H, Lindskog S, Blomlöf L. Relationship between periapical and periodontal status. A clinical retrospective study. J Clin Periodontol. 1993;20(2):117-123.
7. Abbott P. Endodontic management of combined endodontic-periodontal lesions. J N Z Soc Periodontol. 1998;83:15-28.
8. Abbott PV. Medicaments: aids to success in endodontics. Part 1. A review of the literature. Aust Dent J. 1990;35(5):438-448.
9. Ree M, Schwartz RS. The endo-restorative interface: current concepts. Dent Clin N Am. 2010;54(2):345-374.
10. Stewardson DA, Shortall AC, Marquis PM. The effect of the elastic modulus of endodontic posts on static load failure. Int Endod J. 2011;44(5):458-468.
11. Uzunoğlu E, Türker SA, Yilmaz JZ. Influence of cement type and thickness on polyfiber post adhesion. J Conserv Dent. 2014;17(3):255-260.
12. Schwartz RS, Robbins JW. Post placement and restoration of endodontically treated teeth: a literature review. J Endod. 2004;30(5):289-301.