You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
In a recent survey1 of general dentists who were asked to treatment plan a restorative crown material for a mandibular first molar, more than 60% chose an all-ceramic material (including 30% zirconia and 20% lithium disilicate). In the anterior, almost all dentists chose an all-ceramic material. Ceramic materials have gained clinical preference, in part, because of their esthetic properties and reduced laboratory costs. However, perhaps the greatest clinical benefit of ceramic materials is that they are conducive to practicing more conservative dentistry. High-strength ceramics such as zirconia enable clinicians to prepare less tooth reduction because less space is needed for monolithic ceramic restorations than bi-layered metal-based restorations.
Conservation of tooth structure may be further achieved if the clinician chooses to bond the ceramic restoration. Bonded ceramic onlays preserve tooth structure because they do not require removal of tooth structure to obtain retention. Bonded ceramic crowns can be placed on cleansable supragingival margins, as the adhesive bonding achieved by the cement can compensate for a reduced preparation height.
So that the dentist can realize these clinical benefits of ceramic restorations, a sound clinical protocol for bonding should be developed. This article will review the decision-making process of when to bond, steps for bonding zirconia and glass-based crowns, techniques for cleaning ceramics prior to bonding, and the rationale for choosing different resin cements.
When to Bond
Prior to discussing the steps required for bonding, the first consideration should be whether or not bonding is necessary and whether the crown can be cemented with a glass-ionomer or resin-modified glass-ionomer (RMGI) cement. Cementing with RMGI-based cements has several advantages. RMGI cements have good moisture tolerance and should be used in cases where ideal isolation cannot be achieved.2 They are easy to clean up as they are less likely to bond to surrounding tooth structure, and they are less technique-sensitive because they do not require the use of ceramic or tooth primers. RMGI cement can be cleaned with water or phosphoric acid prior to try-in because no chemical bond is formed between the crown and the cement. A restoration planned for replacement that has been cemented with RMGI cement may be easier to cut off, because its bond is less tenacious and the cement is typically very white opaque and easy to visualize.
Various clinical situations dictate that a restoration be bonded. Restorations that have limited or no retention form will require bonding. Examples include, inlays, onlays, veneers, Maryland bridges, short crown preparations, and over-tapered crown preparations. Restorations should also be bonded if it is necessary to gain additional strength for the restoration. High-strength ceramics only require bonding if the restoration is thin; thresholds for the author are approximately 1.5 mm for lithium disilicate, 1 mm for translucent zirconia (also called “anterior” or “cubic” zirconia), and 0.8 mm for traditional zirconia. Ceramics with lower inherent strength should always be bonded, including feldspathic porcelain and resin composite crowns. The use of resin cements may also be preferred for esthetic restorations because they often are less opaque than RMGI cements.
Preparing a Ceramic Restoration for Bonding
For all types of ceramic materials, two steps are needed to prepare the intaglio surface for bonding. First, the surface is roughened to create micromechanical retention. Then, a chemical coupling agent is applied to form a chemical bond between the ceramic material and the resin cement.
Preparation of the intaglio surface of a crown prior to bonding will vary depending on whether or not it is a glass-based ceramic. Glass-based ceramics include porcelain, lithium disilicate, and leucite-reinforced cermaic. Zirconia does not contain glass and, therefore, is treated completely differently than other dental ceramics.
Glass-based Ceramic Restorations
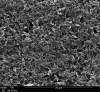
For glass-based restorations, surface roughening is created by etching the ceramic with hydrofluoric acid (Figure 1). Hydrofluoric acid selectively dissolves glass and leaves behind a fine texture of crystals that will interlock with the resin cement (Figure 2). Hydrofluoric acid is a stronger acid than the phosphoric acid used to etch tooth structure and should be kept off of skin or gingival tissue. It can be supplied in 5% or 9.5% concentrations. Etching time will be dependent on the type of ceramic material—lithium disilicate requires 20 seconds of etching with 5% hydrofluoric acid, whereas porcelain requires 1 to 2 minutes of etching with 5% hydrofluoric acid. Most dental laboratories will etch lithium-disilicate and porcelain restorations prior to mailing them back to the dentist. It is important to communicate with the laboratory to ensure that the crowns are being etched.
Following etching, glass-based crowns should then be coated with a primer containing silane. Silane is a molecule that has two functional ends. One end contains a silanol that can bond with hydroxide functional groups found in glass; the other end is a methacrylate that is capable of bonding to methacrylates in resin cements. Only a single coat of silane is needed. The restoration should then be thoroughly dried, because water is a by-product of the reaction between the silane and glass, and its evaporation will drive the reaction.
A clinical suggestion is to apply silane before trying in the crown, as this will protect the crown from contamination prior to delivery. Silane will make the intaglio surface of the crown hydrophobic and, therefore, prevent water-based contaminants in saliva from adhering to the surface.3 In fact, silane is the active ingredient in products that are applied to windshield glass to make it hydrophobic and repel rain water.
Silane can be supplied in several different kinds of products. Pure silane is available in single-bottle or two-bottle adhesive systems. One-bottle systems simplify the armamentarium, however, they have a shorter shelf-life than two-bottle systems. The shelf-life of silane is limited because individual silane molecules can react with each other and make the solution inactive. Expired silane will appear cloudy from the precipitates of reacted silane molecules and should not be used. Silane is also contained in many universal ceramic primers. These primers often contain silane as well as phosphate molecules used to bond to zirconia. This type of primer has been shown to be effective and is a good option for clinicians bonding both glass-based and zirconia restorations.4
Additionally, silane has been added to so-called universal adhesives, which are used as primers for both tooth structure and ceramic. In this case, the monomers present in the adhesive interfere with the activity of the silane. Laboratory studies have shown that universal adhesives are poor primers for glass-based restorations, particularly lithium disilicate.4
Zirconia Restorations
Zirconia does not contain glass, so the bonding procedure is much different. For one thing, there is no need to apply hydrofluoric acid to zirconia because it will not affect its surface, and application of silane will be useless because there is no potential for chemical bonding. The steps for bonding to zirconia include surface roughening with sandblasting (airborne particle abrasion) and application of a primer containing 10-methacryloyloxydecyl dihydrogen phosphate (MDP).
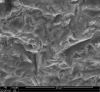
Sandblasting zirconia restorations should be accomplished with 50-µm alumina for 10 seconds at a distance of 10 mm at somewhere between 30 psi to 60 psi of pressure (Figure 3). This procedure will produce surface texture for bonding (Figure 4). Most sandblasting units contain either alumina particles, glass beads, or separate containers for both. Glass beads are less dense than alumina and are much less abrasive. When preparing traditional zirconia, it is necessary to sandblast with alumina particles because glass beads do not create surface texture for bonding. Due to the high strength and toughness of zirconia, sandblasting with alumina does not reduce its strength.5 Newer “translucent” or “cubic” zirconia lacks the transfomation-toughening properties of traditional zirconia and should only be sandblasted with alumina if the crowns will be bonded with a resin cement, not if they are cemented with a RMGI cement. Glass-based ceramics, however, should never be sandblasted with alumina because it will significantly weaken them.6 If the clinician desires to clean glass-based ceramics by sandblasting, glass beads should be used.
A chemical bond may be formed between resin cement and zirconia through the functional monomer MDP. In other words, MDP may be thought of as the “silane for zirconia.” MDP can be obtained in several different products, including pure MDP primers, universal ceramic primers, and universal adhesives. All of these formulations seem to be effective.7
An alternative strategy for bonding to zirconia is through tribochemical abrasion. In this process, zirconia is sandblasted with alumina particles that are covered in silica (glass). The silica coating is deposited onto the surface of the sandblasted zirconia. Once the zirconia has a silica coating on it, it may chemically bond with silane. This technique has been shown to produce effective bonding to zirconia.8
Cleaning the Restoration
Bonding a ceramic crown relies on achieving a chemical bond between the crown and the primer/cement. Contamination from various sources can occur prior to applying the primer or cement. These sources of contamination include stone from the die, oil from fingers, residue from try-in pastes, proteins in blood, and phospholipids in saliva. For glass-based restorations such as feldspathic porcelain or lithium disilicate, the restoration can be cleaned by using phosphoric acid or re-etching with hydrofluoric acid.9 Cleaning zirconia restorations, however, presents a chemical challenge. Phospholipids from saliva can bind to the bonding sites needed for MDP. If the crown is then cleaned with phosphoric acid, the phosphate-based remnants from the phosphoric acid will block the binding sites for MDP.
There are two solutions to this dilemma. The first is to use a cleaning solution (eg, Ivoclean, Ivoclar Vivadent, www.ivoclarvivadent.com) that contains a supersaturated concentration of zirconia particles. When the product is applied to contaminated zirconia, a chemical gradient drives the contaminants from the restoration into the cleaning solution. Another option is to re-sandblast the zirconia crown immediately prior to try-in. This technique has also been proven to be effective in cleaning zirconia.10
Choosing a Cement
The retention of a ceramic crown is dependent on the bond between the crown and the cement, as well as the tooth and the cement. If debonding of ceramic crowns is occurring frequently in a clinical practice, examination of the prepared tooth and the debonded crown may offer clues as to the bonding surface that needs attention. If remnant cement is seen on the tooth, then strategies should be implemented to change the methods of preparing the intaglio surface of the crown. If remnant cement is found on the crown, then cement selection and isolation protocols should be addressed.
Bonding a ceramic crown implies that a resin cement will be used instead of a glass-ionomer or RMGI cement. Resin cements may be classified as self-adhesive, self-etch, or total-etch cements. Self-adhesive cements are those that do not require any type of tooth primer prior to application of the cement. Self-etch cements use a self-etching primer or self-etch adhesive on the tooth prior to cement application. Total-etch cements utilize phosphoric acid on the tooth, followed by a primer/adhesive, and then the cement. Self-adhesive cements are easier to use; however, they do not provide the same level of retention as cements that are applied with the use of a tooth primer.11
Resin cements may also be classified as dual-cure or light-cure only. The advantage of a dual-cure cement is obvious; the cement will chemically cure even if adequate light polymerization is not achieved. This type of cement is particularly advantageous for zirconia crowns because they are too opaque to allow much light to pass through the crown. The advantages of light-cure cements are that they allow the clinician longer working time and they have historically been more color stable than dual-cure cements. The issue with color stability of dual-cure cements is related to an amine-based chemistry, which allows the cement to chemically cure. Recently, amine-free dual-cure cements have been developed to avoid the possibility of color change of the cement.12 Another issue related to dual-cure materials is that the use of an acidic self-etch adhesive on the tooth prior to application of an amine-containing dual-cure cement or build-up material may interfere with the setting reaction of the cement. To avoid this problem, a dual-cure activator can be mixed with the self-etch adhesive, or an amine-free cement can be used. Figure 5 shows a build-up that debonded while taking a final impression. The amine-containing build-up material was placed over an acidic self-etch adhesive.
Summary
Proper selection and application of dental materials can enable the clinician to practice conservative adhesive dentistry. However, new materials cannot substitute for sound clinical technique. Retentive preparation design, proper isolation, and adequate time/light for cement polymerization all affect the clinical success of adhesive bonding.
ABOUT THE AUTHOR
Nathaniel C. Lawson, DMD, PhD
Assistant Professor, Department of Clinical and Community Sciences, Division of Biomaterials, University of Alabama at Birmingham School of Dentistry, Birmingham, Alabama
REFERENCES
1. Makhija SK, Lawson NC, Gilbert GH, et al; National Dental PBRN Collaborative Group. Dentist material selection for single-unit crowns: Findings from the National Dental Practice-Based Research Network. J Dent. 2016;55:40-47.
2. Shimazu K, Karibe H, Ogata K. Effect of artificial saliva contamination on adhesion of dental restorative materials. Dent Mater J. 2014;33(4):545-550.
3. Kalavacharla VK, Kwon S, Godbole SA, et al. Shear bond strength to lithium disilicate with various surface treatments [abstract]. J Dent Res. 2013;92(spec iss B). Abstract 1656.
4. Passia N, Lehmann F, Freitag-Wolf S, Kern M. Tensile bond strength of different universal adhesive systems to lithium disilicate ceramic. J Am Dent Assoc. 2015;146(10):729-734.
5. Michida SM, Kimpara ET, dos Santos C, et al. Effect of air-abrasion regimens and fine diamond bur grinding on flexural strength, Weibull modulus and phase transformation of zirconium dioxide. J Appl Biomater Funct Mater. 2015;13(3):e266-e273.
6. Menees TS, Lawson NC, Beck PR, Burgess JO. Influence of particle abrasion or hydrofluoric acid etching on lithium disilicate flexural strength. J Prosthet Dent. 2014;112(5):1164-1170.
7. Zhao L, Jian YT, Wang XD, Zhao K. Bond strength of primer/cement systems to zirconia subjected to artificial aging. J Prosthet Dent. 2016;116(5):790-796.
8. Tzanakakis EG, Tzoutzas IG, Koidis PT. Is there a potential for durable adhesion to zirconia restorations? A systematic review. J Prosthet Dent. 2016;115(1):9-19.
9. Klosa K, Wolfart S, Lehmann F, et al. The effect of storage conditions, contamination modes and cleaning procedures on the resin bond strength to lithium disilicate ceramic. J Adhes Dent. 2009;11(2):127-135.
10. Angkasith P, Burgess JO, Bottino MC, Lawson NC. Cleaning methods for zirconia following salivary contamination. J Prosthodont. 2016;25(5):375-379.
11. Barcellos DC, Batista GR, Silva MA, et al. Evaluation of bond strength of self-adhesive cements to dentin with or without application of adhesive systems. J Adhes Dent. 2011;13(3):261-265.
12. Ural Ç, Duran İ, Tatar N, et al. The effect of amine-free initiator system and the polymerization type on color stability of resin cements. J Oral Sci. 2016;58(2):157-161.