You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Disclaimer: Participants must always be aware of the hazards of using limited knowledge in integrating new techniques or procedures into their practice. Only sound evidence-based dentistry should be used in patient therapy.
Conflict of Interest Disclosure Statement
Dr. Zablotsky is a senior consultant for the Nova Southeastern University Area Health Education Centers (AHEC) Program and lecturer at the NSU College of Dental Medicine. He is compensated by NSU through institutional funds.
Introduction
There is an acknowledgment amongst health care professionals that working with tobacco and nicotine using patients to quit their addiction is one of the most difficult tasks they are asked to perform. The obligation and duty of a healthcare provider is to prevent disease, thus we ideally should be speaking to parents and their children about the dangers of tobacco use as early as is feasible as most smokers begin using cigarettes between the ages of 10-13.1 In addition, "Secondhand smoke exposure causes disease and premature death in children who do not smoke. Children exposed to secondhand smoke are at an increased risk for sudden infant death syndrome (SIDS), acute respiratory infections, ear problems, and more severe asthma. Smoking by parents causes respiratory symptoms and slows lung growth in their children."2,3
Despite our issuing these warnings, we still have 36.5 million adult smokers (15.1%) in the United States and 8 billion smokers worldwide.4 It is clear that far too many people are suffering. In order to try to make any inroads in reversing this national tragedy, there are many areas that need to be addressed. How did we get here? What products are causing this problem? How do they compromise our health and welfare? What can we do as a profession, and individual, to undo the damage done and prevent future generations from suffering a similar fate?
History of Tobacco
Tobacco's genus, Nicotiana, named in honor of Jean Nicot, the French ambassador to Portugal, contains sixty-four species, two of which have been used by humans for various purposes, Nicotiana rustica, and Nicotiana tabacum. These species are native only to the Americas and were first seen by humans 18,000 years ago. It is estimated that tobacco plants were first cultivated sometime between 5000-3000 B.C in the Peruvian/Ecuadorean Andes and that its use spread throughout the America's and included Cuba as well. As time passed, humans found many uses for this plant. It was initially used by shamans in South America, in religious rites as well as a medicine. It served as a mild analgesic and antiseptic, a poultice applied to wounds and teeth, as eye drops, enemas and as a narcotic. Its smoke was blown on women to make them fertile, and on warriors to give them courage in battles. In 1565 (Seville, Spain) Nicolas Monardes wrote a treatise, "Joyful News of our New Found World" in which he claimed that tobacco could be used to treat toothaches, kidney stones, tape worms, and dandruff.5
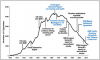
Fast forward to 1889, in the US, James "Buck" Duke formed the American Tobacco Company. Utilizing Virginia inventor James Bonsack's cigarette rolling machine, he made 200 cigarettes a minute. Within five years one billion cigarettes were produced.5 The sale of Duke's cigarettes exploded, leading the way to the production of 30 cigarettes a second and the sales of approximately six trillion cigarettes worldwide in 2014 (Figure 1).6 As this century progresses, we are seeing the tobacco industry expand their sale of cigarettes into Asia, the Middle East and Africa as the market in developed countries shrinks, and as a global health treaty (FCTC), has been introduced to reduce tobacco related diseases. Tobacco companies will continue to create new products which healthcare professionals will need to address as our patients use them.
Tobacco and Nicotine Products
Over the last century, up to the present, the tobacco industry has had a major impact on societal norms and health. They have convinced us that tobacco use would make us chic, calm our nerves, help us maintain a slender figure, be more attractive to the opposite sex, amongst many other things. After Surgeon General Luther Terry's report in 1964 stated unequivocally that "Cigarette smoking is a health hazard of sufficient importance in the US to warrant remedial action" and that it was the cause of lung cancer in men, and most likely women," the tobacco industry has tried to adapt to continue to market their products in various iterations. The purpose of this section is to review the myriad of tobacco products that are presently available to our patients and which continue to potentially compromise their oral and overall health (Table 1).
Cigarettes
The present day cigarette has come a long way from its first ancestor; the papelote, shredded tobacco wrapped in paper, which was smoked by the poor in Spain in the 1800s. The modern-day cigarette has a filter that is made from cellulose acetate fiber, paper or activated charcoal. Below the filter is the cigarette paper and tobacco filler. The paper contains many chemicals one of which is titanium oxide, which accelerates and maintains burning. The tobacco in the cigarette is - shredded tobacco, - "reconstituted tobacco" made from a pulp of mashed tobacco stems, and other parts of the leaf which might go to waste. This mix is then impregnated with nicotine and as much as 600 chemical additives.7 The final third is expanded to puff tobacco, which is tobacco impregnated with Freon and/or ammonia. The ammonia increases the smoker's ability to extract nicotine while smoking.7 Additionally, cigarette smoke has 7,000 chemicals with more than 70 of which can cause cancer.8 Despite the public's awareness of the dangers of smoking, it is estimated that 155,000 men and women in the US will die from lung cancer in 2017,8 90% of which will be caused by cigarette smoking.8 Smoking will also be the cause of one out of three of all cancer deaths, as it is known to cause cancer of the larynx, oral cavity, bladder, pancreas, cervix, kidney, stomach, blood, liver, colon, rectum and the esophagus.8
Thirty-two percent of all coronary heart disease deaths in the United States each year are attributable to smoking. Smoking also contributes to hypertension and stroke, with the risk of ischemic stroke nearly doubling.8v Smoking accounts for 11% of all stroke deaths8 and will also increase the number of Americans getting diabetes, hearing loss and vision problems, chronic coughing, emphysema and bronchitis.8 It will exacerbate asthma in adults and also impair their immune system.8
The bottom line is that cigarette smoking is responsible for more than 480,000 deaths per year in the United States, including more than 41,000 deaths resulting from secondhand smoke exposure.9
Cigars
Higher grade cigars are made of high quality tobacco which has been fermented and aged and used in the filler and wrapper. Low grade and machine made cigars are composed of chopped tobacco as the filler, and the wrapper of long leaves or a paper made from tobacco pulp. Some cigars do have flavorings added. All cigar smokers, whether they inhale or not, expose their lips, tongue and throat to smoke and its toxic and cancer-causing chemicals. While many believe that cigars are not harmful because cigar smoke is not inhaled, studies have shown that some cigar smokers do inhale, thereby absorbing smoke into their lungs and bloodstream and depositing smoke particles in their lungs as well as their stomachs and digestive tract."12-17 Although cigarette use has declined in the US, the use of cigars has increased dramatically since 1993.18 Each year, about 9,000 Americans die prematurely from regular cigar use.10-20
Bidis
Bidis (Figure 2) are small, thin hand-rolled cigarettes mostly made in India and Southeast Asia. They are composed of tobacco wrapped in a tendu or temburnia leaf. Many bidis are flavored. Bidi smoking increases the risk for oral cancer, lung cancer, stomach cancer, and esophageal cancer.21
Kreteks
Kreteks (Figure 3), or clove cigarettes, are imported from Indonesia and contain tobacco, cloves and other additives. Both of these products are not safe alternatives to cigarettes. Regular kretek smokers have 13 to 20 times the risk for abnormal lung function (e.g., airflow obstruction or reduced oxygen absorption) compared with nonsmokers.22
Hookahs and Pipes
The hookah pipe (Figure 4, also called water pipe, shisha, goza, amongst other names) was introduced in the 1500s in the Mideast. Tobacco is heated and the smoke carrying charcoal combustion particles passes through the tobacco to water, which bubbles into a vapor that users inhale.23 Unfortunately, the common perception is that the water in the hookah will filter out harmful chemicals. In reality, "the smoke that passes through the water does not eliminate the hazardous, addictive chemicals released from the tobacco (Figure 5). At least 82 toxicants and carcinogens have been identified in hookah smoke, including tobacco-specific nitrosamines (TSNAs), polycyclic aromatic hydrocarbons (PAHs), and heavy metals."24 During a one hour hookah session a person inhales as much smoke as 100 cigarettes. According to the 2015 Youth Tobacco Survey (YTS), 7.2% of high schoolers and 2.0% of middle schoolers, totaling over 1.2 million youth, have used hookah in the past months.24-26
Additionally, the 2012-2013 Adult Tobacco Survey (ATS) found that 18.2% of 18-24 year olds use hookah every day, some days or rarely; this age group has the highest use rate among all adults. Although other types of pipe smoking have decreased, pipe smoking is still associated with an increased mortality rate from the same diseases as smoking cigarettes.27
Electronic Nicotine Delivery Systems (ENDS)
E-cigarettes are battery powered nicotine delivery systems that produce heated aerosol as opposed to smoke. The first non-tobacco cigarette was credited to Herbert Gilbert in 1967, with the present day e-cigarette's credit going to Hon Lik, a Chinese pharmacist in 2004.
The intent of the e-cigarette is to create a safer and cleaner way to deliver nicotine and help cigarette smokers break their addiction to cigarettes. The liquid used in the e-cigarette is usually composed of propylene glycol and/or glycerin, nicotine ranging from 0-36 mg/ml and up to a possible 7,000 various flavorings and additives. There has been great debate as to the efficacy of these products as a tobacco cessation aid as well as its safety. In addition, there is also the fear that this product may entice young people to use it, and then go on to using more dangerous tobacco products, given the sky rocketing rise in the prevalence of its use in middle and high school students.29 With these concerns in mind, the US Food and Drug Administration (FDA) in 2016 passed new regulations to help protect the public in this regard. Further research will be needed to determine whether e-cigarettes will prove to be an effective smoking cessation aid, and whether it has any detrimental effects on overall health as well as that on the oral cavity (Figure 6).
IQOS (HEETS)30
IQOS was introduced by Philip Morris International in 2014 as an attempt to create a less harmful tobacco alternative to cigarettes. IQOS uses tobacco refills which heats instead of burns, to produce tobacco-flavored vapor. This product tries to recreate the experience of smoking just as the e-cigarette has attempted to do. It is stated that "Because the tobacco is heated and not burned, the level of harmful chemicals is significantly reduced compared to cigarette smoke"30 The FDA is presently evaluating this product.
Smokeless Tobacco
It is speculated the first use of tobacco by humans was by inhaling it in powdered form through the nose thousands of years ago. "Public health authorities including the Surgeon General and the National Cancer Institute have found that smokeless tobacco use is hazardous to one's health and can lead to nicotine addiction."28 Smokeless tobacco contains 3,000 chemicals and at least 28 carcinogens causing oral, pancreatic and esophageal cancer.28 The use of smokeless tobacco is also associated with other health problems including lesions in the mouth and tooth decay."31
Snuff
Snuff (Figure 7) is a finely ground, moist, fire-cured tobacco that is placed between the lower lip and the gums, or SNUS, the Swedish name for snuff which may have less nitrosamines and is similarly used. Nicotine is absorbed through the oral mucosa.
Chewing Tobacco
This product comes as a loose leaf, twist or plug. Chewing tobacco (Figure 8) is chewed or placed between the cheek and gum and left there for several hours. Nicotine is absorbed through the oral mucosa.
Compressed Tobacco
This form of smokeless tobacco is finely-processed tobacco that can be dissolved in the mouth. This product comes in the form of sticks, strips, orbs and lozenges (not the same as those used for quitting smoking), and as they linger in the mouth can create pathologies as well. Nicotine is absorbed through the oral mucosa.
Impact of Tobacco Use in the Oral Cavity
Impact on Oral Health
Tobacco use is associated with many oral pathologies including cleft lip and palate formation, dental caries, periodontal diseases, implant failure, nicotinic stomatitis, leukoplakia, and life threatening oral and oropharyngeal cancer.
Cleft Lips and Palates (Figure 9). Studies have shown that maternal smoking, be it passive or active during pregnancy, may be associated with an increased risk for cleft lips and palates in offspring.32,33
Dental Caries (Figure 10). There is a higher incidence of dental caries seen in those using tobacco products as there is an increased acidity seen in the oral cavity and a decreased buffering capacity of the saliva.8
Periodontal Disease (Figure 11). To quote the 2014 Surgeon General's report, "The evidence is sufficient to infer a causal relationship between smoking and periodontitis."2 This was highlighted by Tomar and Asma, when they showed that 52.8% (8.1 million people) of periodontitis in the US population was attributable to current and former smokers.31 In addition, it was also demonstrated that quitting smoking reduced the risk of periodontitis.8,34
Dental Implants (Figure 12). Given that the anchoring of a dental implant is achieved by osseointegration, and smoking is a risk factor for the destruction of soft and hard tissue that support the teeth, it is agreed that smoking increases the risk of implant failure.2,8,35-38
Leukoplakia. Leukoplakia (Figure 13) occurs six times more frequently in smokers than non-smokers. It also has been shown that over 40% of smokeless tobacco users exhibit a lesion where the tobacco is held. Given the unpredictability of benign leukoplakia changing to a malignancy, these lesions must be carefully assessed.2,8
Oral Cancer (Figure 14). The American Cancer Society estimates that 49,670 people will get oral and oropharyngeal cancer in 2017, with 9,700 dying from these cancers, which is most commonly squamous cell carcinoma. The risk of developing oral cancer is much greater in tobacco users than in non-users as approximately 75% of all people getting oral cancer use tobacco. The combination of tobacco and alcohol use increases the odds even further.2,8
Given the dire consequences of developing oral cancer, it is incumbent upon dental professionals to discuss tobacco's role in causing this disease and through tobacco cessation prevent oral cancer from occurring.
Nature of Addiction
Taber's medical dictionary defines addiction as, "An enslavement to some habit." As we will see in this section, addiction is a multifaceted process and is a disease that needs to be treated as such. There are basically two components to addiction. First there is a physical component, a substance creates a dependence by inducing a physiologic change in the body. Secondly, we see a psychological process at work as well, with certain compulsive behaviors involving actions that reinforce themselves.
Tobacco or nicotine addiction is a combination of a physical addiction and habitual behaviors. In addition, scientists have noted there is also a genetic component that may make certain people more vulnerable to addiction. Younger people need to be aware that based on their family history they may need to be even more cautious as to exposing themselves to nicotine containing products.39
Physical Addiction
Nicotine was first isolated in 1828 in Heidelberg, Germany. It is a clear liquid and poisonous alkaloid. It is found in tobacco, and to a much lesser concentration, in tomatoes, potatoes and eggplants. It binds to the alpha 4 beta 2 nicotinic receptor sites in the Ventral Tegmental Area of the brain and is believed to cause the release of dopamine at the Nucleus Accumbens region. Scientists state that nicotine is as addictive as heroin and cocaine, with inhaled cigarette smoke affecting the brain in five seconds. It takes approximately 5 cigarettes or 4-6 mg of nicotine to reach the threshold of addiction.40 Nicotine is far from a benign chemical as it increases clotting tendencies, causes bronchospasms, alters heart rates, increases blood pressure, causes coronary artery constriction, causes hyperinsulinemia, and insulin resistance amongst other things. In addition to all of this, it initiates feelings of pleasure, helps concentration, reduces anxiety, relieves pain, and curbs one's appetite, all contributing to why it is so difficult to give up using it.
Psychological Addiction
The psychological component of nicotine addiction can be viewed as a series of habits that are reinforced with rewards. As proposed by Charles Duhigg in his excellent book, "The Power of Habit," habits involve three processes, an environmental cue, a behavioral routine, and a reward. Some of the environmental cues in smoking and tobacco use may be a cup of coffee, an alcoholic drink, smoking with friends, playing a sport, driving in a car, or stressors created by work, family or other social situations.
The behavioral routine would be to light up a tobacco or nicotine containing product, and the reward would be a release of dopamine or endogenous opioids, creating the beneficial feelings stated above.
It is clear that in order to break a dependence on nicotine, a patient will need to have to address both their physical as well as psychological addictions.
Tobacco and Nicotine Cessation
Every year about 70% of smokers would like to quit their nicotine addiction, with 40% making an attempt to do so. Sadly, only about 7% succeed on their first attempt,40 but patients need to realize that it may take many attempts to finally be successful at quitting, even as many as 30,41 but they should continue to try. There are various ways that people try to quit. These include cold turkey, nicotine replacement therapies (NRT), Bupropion (Zyban), Varenicline (Chantix, Champix), and counseling (Figure 15).42,43
The fears of the user to quit include withdrawal symptoms, weight gain, the expense of NRT, and a fear of failure if they are unable to be successful in the attempt. Withdrawal symptoms include, dysphoria, anxiety, irritability, a decrease or increase in heart rate, insomnia, an increase in appetite, and a craving for more nicotine. Withdrawal symptoms can begin as soon as 4 hours after the last cigarette and peak at 3-5 days. Cravings usually last for 3-5 minutes. Most of these symptoms disappear in about 6 months, but as most tobacco users will tell you, they always fear relapsing back to their old habits.
Cessation Approaches
Research shows that people who use a combination of brief counseling, medication and follow-up advice are often successful in stopping. Various NRT's can be combined, and under certain circumstances used with other drugs.
Nicotine Replacement Therapies
Nicotine therapy is a gradual quit approach that uses patches as well as other products to deliver different dosages of nicotine over a given period of time. These products are sold over-the-counter, but patients should seek the guidance of a healthcare professional who is knowledgeable of these products and knows the patients' medical and mental health history to maximize their effectiveness.
Nicotine replacement therapies are represented by an array of products which each may prove to be effective based on the individual.41
Nicotine Patch (Figure 16). This product delivers a varying dosage transdermally (7mg, 14mg, 21mg), based on the extent of a patient's nicotine addiction. The patch can deliver nicotine for a 16 or 24 hour period, and is intended to wean the patient off of nicotine over an 8 or 10 week period.
Nicotine Gum and Lozenges (Figure 17). Nicotine gum and lozenges deliver nicotine more quickly to the brain than the patch, and allow the patient to have more control of their nicotine intake if they experience strong or frequent cravings. Ideally these products will be used for approximately 12 weeks. Nicotine gum and lozenges come in 2 and 4mg dosages.
Nicotine Inhalers. Nicotine inhalers deliver 4 mg of nicotine which is delivered from a porous plug containing 10mg of nicotine. Initial treatment usually can last from 6-12 weeks.
Pharmacological Agents
Bupropion HCL (Zyban). This drug was approved for medical use in 1989. It inhibits the neuronal uptake of norepinephrine and dopamine and is a nicotinic antagonist. It is used as an antidepressant and smoking cessation aid. In a 2013 Cochrane review of medications used for smoking cessation, Bupropion helped about 80% more people quit than placebo.42 This drug is contraindicated for epileptics/people with lower seizure thresholds or people taking MAO inhibitors. It should also be used cautiously in patients with liver damage, severe kidney disease or severe hypertension, and in pediatric patients, adolescents, and young adults due to potential suicide ideation.42 The most common side effects are headache and transient insomnia. A thorough review of this drug must be done before prescribing it by any healthcare provider.
Varenicline (Chantix, Champix). Varenicline (Figure 18) was developed by modifying the structure of cytosine and was approved for use in 2006. This drug is used to treat nicotine addiction. It is a nicotinic receptor site partial agonist and can reduce cravings and decrease the pleasurable effects of tobacco products. In a 2013 Cochrane review,42 Varenicline more than doubled the chances of quitting compared to placebo. It has not been tested for those under 18, or pregnant women, and is not recommended for this group. The most common side effect is nausea. Less common side effects include headache, difficulty sleeping and nightmares. A 2014 systematic review did not find any increased suicide risk.43 Multiple recent reviews also found no increase in overall or serious cardiovascular events.44 Again, a thorough review of this drug must be done before it is prescribed.
In Summary
"NRT and Bupropion helped about 80% more people to quit than placebo; this means that for every 10 people who quit with placebo about 18 could be expected to quit with NRT or with Bupropion. Varenicline more than doubled the chances of quitting compared with placebo, so that for every 10 who quit with placebo about 28 could be expected to quit with Varenicline.
Varenicline helped about 50% more people to quit than nicotine patch and ‘other' NRT (tablets, sprays, lozenges and inhalers), and about 70% more people than nicotine gum. So for every 10 people who quit with NRT patch or with ‘other' NRT, about 15 could be expected to quit with Varenicline, and for every 10 who quit with NRT gum about 17 could be expected to quit with Varenicline. Combining two type of NRT was as effective as using Varenicline, and helped more people to quit than single types of NRT. There was little to choose between different types of NRT, apart from ‘other NRT, which helped slightly more people than nicotine gum; for every 10 people who quit with NRT gum, about 12 could be expected to quit with ‘other' NRT.
NRT combined with Nortriptyline or with Bupropion was not more effective than NRT alone."43
The Role of the Dental Professional
At the outset, the dental team must systematically identify all tobacco using patients. (Ask), clarify what they use and how often, and then (Assess) the level of their addiction and readiness to quit. Over the years the Fagerström test works well in gauging this.
• Pre-contemplative stage: Not usually ready to quit for at least six months
• Contemplative stage: Usually ready to quit in 1 to six months
• Preparative stage: Ready to quit in less than one month.
The method one uses to discuss tobacco use with a patient can be modified based on their addiction level and stage of readiness (Figure 19 through Figure 22).
Motivational Interviewing (MI)
Motivational interviewing as a technique was developed in the early 1980s by Bill Miller and Steve Rollnick. It is "a person-centered, collaborative, and goal-oriented style of communication. It is designed to strengthen personal motivation for and commitment to a specific goal by eliciting and exploring the person's own reasons for change within an atmosphere of acceptance and compassion."48 This communicative style cannot only be used to help work with tobacco using patients to quit, but can also be incorporated in motivating patients to improve their overall oral health.
Initially, one asks for permission from the patient to discuss their tobacco addiction, and then reflectively listens to what the patient has to say, and then summarizes what has been said. Questions need to be open-ended, non-confrontational, and non-judgmental. Ultimately, the patient must feel that they are self-motivated and have been empowered to change.
Case Studies and Role Playing Scripts
Case 1: Susan (Pre-contemplative)
• 45-year-old female who presents as a new patient
• Smokes 2 packs of cigarettes a day
• Has smoked since age 12
• Has Type-2 Diabetes
• Takes Sitagliptin 100mg once a day
• No past quit attempts
• Husband smokes, parents and grandparents smoked
• Slightly overweight
• No interest in quitting smoking
• Advanced periodontal disease
Patient presents with maxillary and mandibular anterior teeth having been extracted and is wearing transitional removable appliances.
Decisions need to be made as to smoking cessation, periodontal treatment and tooth replacement. The photos and dental radiographs were taken prior to the referral (Figure 23 through Figure 25), and the periodontal charting done post-op (Figure 26).
Script for Dental Health Professional (DHP) and the Patient [Note if an MI technique was used it is described after in brackets]
DHP: Hi Susan.
Now that you have had your abscessed front teeth extracted, we need to discuss further how you will approach your periodontal treatment and more permanent tooth replacements, as well as your cigarette smoking. Do you mind if we talk about your smoking at this time? [Asking permission]
Patient: You know, my teeth did seem to be flaring out a bit over the years. In fact, it is funny, but my 9-year-old niece told me that my teeth looked weird. It made me look at my teeth more closely. That was what got me to the dentist. I really feel terrible about losing my front teeth.
DHP: I am sure this has been a very difficult thing for you to go through. [Empathic response]. It does appear your upper and lower front teeth were moving because of the bone loss due to your periodontal infection. Do you think that your smoking may have contributed to this? [Asking the patient to give voice to what might be the cause of the problem]
Patient: I don't know. I have been trying to floss and brush more. I guess my smoking may have helped cause this.
DHP: Is it okay if we talk about that for a few minutes? [Asking permission] What do you know about the relationship between smoking and oral health? [Use an open-ended question to have the patient give voice before giving her information or lecturing her]
Patient: Look, I know that smoking isn't good for my health, but I really like smoking. It makes me feel good. My whole family smokes, and my grandparents are in their 80's and they are fine. Anyway, everyone has to die from something.
DHP: What I hear you saying is that on the one hand, you really enjoy smoking, and on the other hand, you are aware it's causing all sorts of health problems. [Use a double-sided reflection to let the patient hear her ambivalence about quitting]
On the following scale (show the patient the readiness ruler) from 1 to 10, where 1 is not ready to quit smoking and 10 is definitely ready to quit, what number best reflects how ready you are right now to quit? [Use a Readiness Ruler to assess a patient's readiness to quit]
Patient: I don't know, probably a 2.
DHP: And where were you 6 months ago on that same scale?
Patient: Definitely a 1.
DHP: Okay, how did you go from a 1 to a 2?
Patient: Not sure, but my niece's comment made me feel awful.
DHP: What would it take to move from a 2 to a 3?
Patient: Well, I don't want to lose any more of my teeth.
DHP: I can understand if you are not entirely ready to quit smoking right now. [Sounding empathic] For most smokers it is not easy, especially if they have been smoking for many years. [Normalizing]
While it sounds this is not the right time for you to quit, [Reflection] what I'm wondering is if you would be willing to take some pamphlets on quitting smoking and referral resources, and we can talk about this more as you go through your oral hygiene instruction and initial cleanings. [Ask, Advise and Refer]
Patient: Sure. Thanks.
Case 2: Tom (Contemplative)
• 62-year-old male who has been a patient for past 20 years
• Smoked 1½ packs per day for past 40 years
• Diltiazem extended release capsule 540mg in the morning for high BP
• Chronic cough
• Advanced periodontal disease despite past periodontal surgery
Beginning to lose teeth, no maxillary or mandibular molars, premolar teeth failing.
Patient had quit smoking in the past but relapsed due to a difficult time in his family life and work.
Patient is ambivalent about quitting smoking at the present time but would consider the possibility in the next 6 months.
Script for Dental Health Professional (DHP) and the Patient [Note if an MI technique was used it is described after in brackets]
DHP: Hi Tom, how are you doing today? In looking at your new X-rays and periodontal charting, it seems that your premolar teeth are starting to fail (Figure 27 and Figure 28). We spoke on your last visit about your tobacco use; would you mind if we talked about your smoking again today? [Asking permission]
Patient:You know I realize that my periodontal disease is getting worse, and my cough is really bugging me. I know that my smoking is causing all kinds of problems, but despite all that, I don't know if I can deal with quitting right now. On the other hand, I really don't want to lose my teeth.
DHP: It sounds like part of you wants to quit but another part of you finds it very difficult. [Reflective listening] Many people report feeling like you do … they want to quit smoking for their health, but find it difficult. [Normalizing] Let me ask you, what are some of the good things for you about your smoking? [Decisional balancing]
Patient: I guess smoking makes me feel good, helps me deal with stress, and relaxes me. You know, I tried to stop 10 years ago, but after my divorce I went back right away to smoking.
DHP: I am sensing that there is a lot of pressure on you to change because of your health problems and knowing that your blood pressure medication can cause additional gum problems, but you are not sure you can do it because you have tried before. [Reflective listening]
Patient: Yes. It is difficult and I'm not sure I can do it. However, as far as my periodontal disease, what are my options?
DHP: Wearing partial dentures could be a possible way to replace your teeth but my sense is that you might not like having to take them in and out every day. Another alternative is to have implants, but the failure rate for people who smoke is much higher due to slower healing.
Patient: I know I need to stop. Can I set up an appointment to talk about the implants at my next 3-month recall?
DHP: Sure. Let me get some pamphlets that explain about how smoking can interfere with the success rates of the implants and we can discuss this at your next visit. Also, would you like some information about how to quit smoking and where you can go if you need additional help? [Ask, Advise, and Refer]
Patient: Yes, that sounds like a good plan and we can talk about it at my next visit.
DHP: That's great. I look forward to talking with you in 3-months, but if you change your mind and want to consider quitting sooner please call me.
Case 3: Claire (Oral Cancer Victim)
Patient began smoking in her early teenage years and continued to smoke at least a pack a day throughout her adult life as well as drink alcohol moderately. She continued to smoke despite watching her mother pass away from lung cancer, and being diagnosed herself in her 40s with breast cancer for which she had a mastectomy. No radiation or chemotherapy was needed at that time.
In her 60s, she noticed changes on the inside of her cheek and face and then presented with the following. The patient was referred to an oral surgeon to evaluate these lesions and was diagnosed with an advanced squamous cell carcinoma (Figure 29 through Figure 32).
She had surgeries to remove all of her maxillary teeth along with a portion of her face and palate, as well as place a graft to repair her face (Figure 33 and Figure 34). Ultimately, her only source of nutrition was through a feeding tube. She survived for two years after her diagnosis in significant pain.
Despite watching his sister suffer and being diagnosed himself with a blood dyscrasia and aneurysms, and the warning by his physicians that he must quit to survive, the patient's brother continues to smoke over one pack a day.
This case highlights the power of a nicotine addiction and how difficult it is to get patients to quit their tobacco use. It also reminds us why it is our duty to try.
Conclusion
When discussing quitting smoking or tobacco use, many patients will say that they have to die from something, so why bother to quit. Unfortunately, some of the repercussions for this addiction are miserable chronic diseases that do not end quickly or pleasantly. Clearly, there are many challenges for the dental professional in trying to get their patients to quit this addiction. It takes time, is frustrating, requires education and an organization of the office team, and is rarely reimbursable. Despite all of that, the satisfaction one gets in watching someone break this addiction, and how it positively impacts them, as well as their friends and relatives is quite fulfilling in itself. In order to be effective, a dental office must be knowledgeable about tobacco and nicotine addiction, have resources such as brochures in the office to read, as well the contact information for counselors, and quit lines that are available in the area.
References
1. Johnston LD, O'Malley PM, Bachman JG, et al. Monitoring the Future: National Survey Results on Drug Use, 1975-2012. Volume I, Secondary School Students. 2013 Jun. Accessed October 18, 2017.
2. U.S. Department of Health & Human Services. The Health Consequences of Smoking-50 Years of Progress: A Report of the Surgeon General. 2014. Accessed October 18, 2017.
3. U.S. Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta, GA. 2006.
4. CDC. Smoking & Tobacco Use. Current Cigarette Smoking Among Adults in the United States. 2016 Dec 1. Accessed October 18, 2017.
5. Gately I. Tobacco: a cultural history of how an exotic plant seduced a civilization. New York, NY. Grove Press. 2001.
6. U.S. Department of Health & Human Services. A Report of the Surgeon General. 1986. Accessed October 18, 2017.
7. U.S. Food and Drug Administration. How Cigarettes Are Made and How You Can Make a Plan to Quit. 2017 Apr 24. Accessed October 18, 2017.
8. U.S. Department of Health & Human Services. The Health Consequences of Smoking-50 Years of Progress: A Report of the Surgeon General. 2014. Accessed October 18, 2017.
9. CDC. Smoking & Tobacco Use. Tobacco-Related Mortality. 2016 Dec 1. Accessed October 18, 2017.
10. Wikipedia. Cigar. Accessed October 18, 2017.
11. NIH. National Cancer Institute. Smoking and Tobacco Control Monograph No. 9. Accessed October 18, 2017.
12. NIH. National Cancer Institute. Cigar Smoking and Cancer. 2010 Oct 27. Accessed October 18, 2017.
13. NIH. National Cancer Institute. Monograph 9: Cigars: Health Effects and Trends. 1998. Accessed October 18, 2017.
14. Campaign for Tobacco-Free Kids. The Rise of Cigars and Cigar-smoking Harms. Accessed October 18, 2017.
15. Rodriguez J, Jiang R, Johnson WC, et al. The association of pipe and cigar use with cotinine levels, lung function, and airflow obstruction: a cross-sectional study. Ann Intern Med. 2010 Feb 16;152(4):201-10. doi: 10.7326/0003-4819-152-4-201002160-00004.
16. McDonald LJ, Bhatia RS, Hollett PD. Deposition of cigar smoke particles in the lung: evaluation with ventilation scan using (99m)Tc-labeled sulfur colloid particles. J Nucl Med. 2002 Dec;43(12):1591-5.
17. Chang CM, Corey CG, Rostron BL, et al. Systematic review of cigar smoking and all cause and smoking related mortality. BMC Public Health. 2015 Apr 24;15:390. doi: 10.1186/s12889-015- 1617-5.
18. NIH. National Cancer Institute. Cigars: Health Effects and Trends. Monograph 9: Smoking and Tobacco Control. 1998. Accessed October 18, 2017.
19. Nonnemaker J, Rostron B, Hall P, et al. Mortality and Economic Costs From Regular Cigar Use in the United States, 2010. American Journal of Public Health. 2014;104(9):e86-e91. doi:10.2105/ AJPH.2014.301991.
20. NIH. National Cancer Institute. Cigars: Health Effects and Trends. Monograph 9: Smoking and Tobacco Control. 1998. Accessed October 18, 2017.
21. CDC. Smoking & Tobacco Use. Bidis and Kreteks. 2016 Dec 1. Accessed October 18, 2017.
22. Mangunnegoro H, Sutoyo DK. Environmental and occupational lung diseases in Indonesia. Respirology. 1996 Jun;1(2):85-93.
23. Campaign for Tobacco-Free Kids. Hookah is not Harmless. Accessed October 18, 2017.
24. U.S. Department of Health & Human Services. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General, 2012. Accessed October 18, 2017.
25. Shihadeh A. Investigation of mainstream smoke aerosol of the argileh water pipe. Food Chem Toxicol. 2003 Jan;41(1):143-52.
26. Cobb C, Ward KD, Maziak W, et al. Waterpipe tobacco smoking: an emerging health crisis in the United States. Am J Health Behav. 2010 May-Jun;34(3):275-85.
27. Henley SJ, Thun MJ, Chao A, et al. Association between exclusive pipe smoking and mortality from cancer and other diseases. J Natl Cancer Inst. 2004 Jun 2;96(11):853-61.
28. Hartmann-Boyce J, McRobbie H, Bullen C, et al. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. 2016 Sep 14;9:CD010216. [Epub ahead of print]. doi: 10.1002/14651858.CD010216.pub3.
29. CDC. E-cigarette use triples among middle and high school students in just one year. 2015 Apr 16. Accessed October 18, 2017.
30. Science and Innovation. Heated Tobacco Products. Heating tobacco to release flavors and nicotine without combustion. Accessed October 18, 2017.
31. Greer RO Jr, Poulson TC. Oral tissue alterations associated with the use of smokeless tobacco by teen-agers. Part I. Clinical findings. Oral Surg Oral Med Oral Pathol. 1983 Sep;56(3):275-84.
32. Li Z, Liu J, Ye R, et al. Maternal passive smoking and risk of cleft lip with or without cleft palate. Epidemiology. 2010 Mar;21(2):240-2. doi: 10.1097/EDE.0b013e3181c9f941.
33. Xuan Z, Zhongpeng Y, Yanjun G, et al. Maternal active smoking and risk of oral clefts: a meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016 Dec;122(6):680-690. doi: 10.1016/j. oooo.2016.08.007. Epub 2016 Aug 18.
34. Tomar SL, Asma S. Smoking-attributable periodontitis in the United States: findings from NHANES III. National Health and Nutrition Examination Survey. J Periodontol. 2000 May;71(5):743-51.
35. Warnakulasuriya S, Dietrich T, Bornstein MM, et al. Oral health risks of tobacco use and effects of cessation. Int Dent J. 2010 Feb;60(1):7-30.
36. Strietzel FP, Reichart PA, Kale A, et al. Smoking interferes with the prognosis of dental implant treatment: a systematic review and meta-analysis. J Clin Periodontol. 2007 Jun;34(6):523-44. doi: 10.1111/j.1600-051X.2007.01083.x.
37. Hinode D, Tanabe S, Yokoyama M, et al. Influence of smoking on osseointegrated implant failure: a meta-analysis. Clin Oral Implants Res. 2006 Aug;17(4):473-8. doi: 10.1111/j.1600- 0501.2005.01244.x.
38. Baig MR, Rajan M. Effects of smoking on the outcome of implant treatment: a literature review. Indian J Dent Res. 2007 Oct-Dec;18(4):190-5.
39. Prokhorov AV, Pallonen UE, Fava JL, et al. Measuring nicotine dependence among high-risk adolescent smokers. Addictive Behaviors. 1996;21(1):117-27. doi: 10.1016/0306-4603(96)00048- 2. Accessed October 18, 2017.
40. Benowitz NL, Henningfield JE. Establishing a nicotine threshold for addiction. The implications for tobacco regulation. N Engl J Med. 1994 Jul 14;331(2):123-5. doi: 10.1056/ NEJM199407143310212.
41. Chaiton M, Diemert L, Cohen JE, et al. Estimating the number of quit attempts it takes to quit smoking successfully in a longitudinal cohort of smokers. BMJ Open. 2016;6(6):e011045. doi:10.1136/bmjopen-2016-011045.
42. Hughes JR. New treatments for smoking cessation. CA Cancer J Clin. 2000 May-Jun;50(3):143-51; quiz 152-5.
43. Cahill K, Stevens S, Perera R, et al. Pharmacological interventions for smoking cessation: an overview and network meta-analysis. Cochrane Database Syst Rev. 2013 May 31;(5):CD009329. doi: 10.1002/14651858.CD009329.pub2.
44. Hughes JR. New treatments for smoking cessation. CA Cancer J Clin. 2000 May-Jun;50(3):143-51; quiz 152-5.
45. Fiore MC. US public health service clinical practice guideline: treating tobacco use and dependence. Respir Care. 2000 Oct;45(10):1200-62.
46. Prochaska JJ, Hilton JF. Risk of cardiovascular serious adverse events associated with varenicline use for tobacco cessation: systematic review and meta-analysis. BMJ. 2012 May 4;344:e2856. doi: 10.1136/bmj.e2856.
47. Heatherton TF, Kozlowski LT, Frecker RC, et al. The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991 Sep;86(9):1119-27.
48. Severson HH, Hatsukami D. Smokeless tobacco cessation. Prim Care. 1999 Sep;26(3):529-51.
49. Sobell L, Sobell M. AHEC Tobacco Cessation Clinician Resource. Nova Southeastern University School of Dental Medicine.
50. Ruiz JJ. Promoting Tobacco Cessation Using Motivational Interviewing Strategies.
About the Author
Nevin Zablotsky, DMD
Dr. Zablotsky received his dental and postgraduate degree in periodontology from the Tufts School of Dental Medicine. He has lectured throughout the US and internationally on tobacco related issues and has lectured, and continues to lecture for the American Dental Association. He recently authored a chapter on tobacco and oral health, and tobacco cessation in the periodontal textbook, "Non-Surgical Control of Periodontal Diseases." He received the Vermont Advocate of the Year award from the American Cancer Society and the lifetime achievement award for the Vermont Special Olympics, and was the past president of the Vermont Periodontal Society.
Email: nev1248@aol.com