You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The ADAA has an obligation to disseminate knowledge in the field of dentistry. Sponsorship of a continuing education program by the ADAA does not necessarily imply endorsement of a particular philosophy, product, or technique.
Snoring and Obstructive Sleep Apnea
It is estimated that 24 percent of all adult women and 40 percent of all adult males snore (Table 1). Both men and women are likely to snore as they age. Alcohol, drugs, muscle relaxers and tobacco products contribute to snoring. Overweight individuals have more fatty tissue around their neck causing a closing off of the airway, and women who are pregnant have a tendency to snore more. It is estimated that over 2 percent of children under the age of 12 snore. It is important to remember, that while snoring is a symptom of sleep apnea, not all people who snore have obstructive sleep apnea. Many people do not realize they snore unless they are told by a partner. Even when told, since they do not awaken, they do not recognize it as a problem. Both parties can suffer from sleeplessness due to the loud snoring, causing stress and a strain in the relationship.
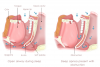
Obstructive sleep apnea, or OSA, is a sleep-related breathing disorder. It occurs when the tissues in the airway collapse, either partially or completely. These collapses can happen hundreds of times a night. The pause can last for as little as 10 to 30 seconds or be as long as a minute or perhaps even longer. When the collapse occurs, the brain causes the person to wake up and begin breathing, although the individual may not even be aware they have awoken. A person having 15 of these episodes per hour of sleep is considered to have mild or moderate sleep apnea.
If left untreated, the effects on a person's bed partner can be disastrous.
Stages of Sleep
There are two distinct sleep states; the first is called rapid eye movement, or REM. REM is the deep sleep the body requires to feel rejuvenated. It is typically entered about 90 minutes after initially falling asleep and can recur about five times in an eight-hour sleep cycle. Non-REM occurs in four separate stages, each describing a deeper state of restfulness. Snoring only occurs during non-REM sleep. When suffering from obstructive sleep apnea, the body is consistently being deprived of REM sleep. Symptoms of sleep deprivation may be evident even though the person believes he/she is sleeping soundly through the night. People with OSA report getting 8 to 10 hours of sleep a night only to catch themselves falling asleep at the wheel while driving to work the next morning.
Signs and Symptoms of Obstructive Sleep Apnea
• restless or fragmented sleep
• insomnia
• excessive daytime sleepiness
• loud snoring
• xerostomia (dryness of the mouth from breathing through it)
• trouble concentrating
• irritability
• memory loss
• depression
• morning headaches
• decreased sex drive
• inability to focus mentally on work or project
• family history
Children With Obstructive Sleep Apnea
Children with OSA have many of the same symptoms as adults: daytime sleepiness and an inability to concentrate, along with behavioral difficulties without any obvious cause, irritability, and bed wetting. It is believed that many children with OSA are misdiagnosed with either Attention Deficit Disorder (ADD) or Hyperactivity. Children also seem to not gain weight or grow at a normal rate due to lower levels of growth hormones. They also have trouble learning as they cannot concentrate on tasks such as school work.
A study published in March, 2017 in the Journal of Scientific Reports compared 16 children between 7 and 11 years of age who have moderate or severe obstructive sleep apnea to children the same age who slept normally, found significant reductions of gray matter—brain cells involved in movement, memory, emotions, speech, perception, decision making and self-control—in several regions of the brains of children with sleep apnea.
The finding points to a strong connection between this common sleep disturbance, which affects up to five percent of all children, and the loss of neurons or delayed neuronal growth in the developing brain. This extensive reduction of gray matter in children with a treatable disorder provides one more reason for parents of children with symptoms of sleep apnea to consider early detection and therapy.
Diagnosis
If symptoms suggest obstructive sleep apnea, further testing will need to be performed. A polysomnography is a “sleep study” that is done to evaluate the patient's sleep pattern by measuring the Apnea-Hypopnea Index using electrodes. This type of study requires an overnight stay in a sleep study facility. An Apnea-Hypopneas Index or AHI is the average number of partial and complete pauses in breathing that occurs per hour of sleep. A person with an AHI of more than 30 occurrences in a one-hour period is considered to have severe sleep apnea.
According to the American Academy of Dental Sleep Medicine, a physician is responsible for the diagnosis of sleep disorders and for recommending a treatment option. Dentists are not permitted to diagnose sleep apnea, but they can help screen patients for this serious condition. Because dentists see patients on a regular basis, they have the opportunity to engage in conversation about sleep apnea and advise at-risk patients to speak to their physician and visit a sleep center for further testing. Given that the number of practicing dentists is more than 180,000 in the United States, this increases access to patients and the opportunity to alert them about the serious risk of untreated OSA.
Recovery after Stroke or Heart Attack
If sleep apnea increases the risk of stroke, either directly or indirectly, untreated patients with comorbid OSA may have worse functional outcomes and higher mortality after acute stroke. Several observational studies suggest that OSA is a predictor of poor functional outcome after stroke, increasing the likelihood of dependency and post stroke mortality.
Treatment Options
Although the options vary greatly for the treatment of OSA, treatment must be tailored to the individual patient based on medical history, physical examination and the result of a sleep study program.
Treatment with CPAP has the unique potential to improve the recovery from stroke and to reduce the risk of recurrent stroke both indirectly through better control of multiple modifiable risk factors and directly through a variety of proposed mechanisms. It is an effective treatment for OSA, reducing OSA-associated hypertension, atrial fibrillation, cardiovascular morbidity and mortality, exclusive of stroke, and reducing daytime somnolence. CPAP provides a constant, positive pressure to the airway throughout the respiratory cycle, serving to splint open the upper airways to prevent narrowing or collapse. The impact of early treatment of OSA with CPAP on neurologic recovery after stroke is just beginning to be studied.
Summary
OSA is more common than most people realize. Because the biggest warning sign is snoring, most people pass it off as an annoyance; however, this disease is far more dangerous when left untreated. A person's health, work and everyday lifestyle can be greatly affected. It is important for any person to seek a medical evaluation if suffering from any of these symptoms. A sleep study is necessary to properly diagnose OSA; diagnosis and treatment can have a profound effect on children and adults. Treatment options vary from the simplest of lifestyle changes (Table 2) to oral appliances to surgery (Table 3). All options should be discussed with a physician to find the right choice of treatment.
Glossary
AADSM- American Academy of Dental Sleep Medicine; the only non-profit national professional society dedicated exclusively to the practice of dental sleep medicine
AASM- American Academy of Sleep Medicine; the only professional society dedicated exclusively to the medical subspecialty of sleep medicine
Apnea-Hypopnea Index/AHI- an index of sleep apnea severity that combines apneas and hypopneas; the apneas must last for at least 10 seconds and are associated with a decrease in blood oxygenation
continuous positive airflow pressure/CPAP- therapy utilizes a machine to help a person who has obstructive sleep apnea (OSA) breathe more easily during sleep
diabetes- metabolic disease in which the body's inability to produce any or enough insulin causes elevated levels of glucose in the blood
gastroesophageal reflux disease/GERD- condition in which the stomach contents (food or liquid) leak backwards from the stomach into the esophagus (the tube from the mouth to the stomach); this action can irritate the esophagus, causing heartburn and other symptoms
laser-assisted uvulopalatoplasty/LAUP- a surgical procedure performed with the aim of reducing or eliminating snoring
non-REM- a type of sleep that occurs in stages, each one getting deeper until the person reaches REM
obesity- the condition of being grossly overweight
obstructive sleep apnea/OSA- a type of sleep disorder characterized by pauses in breathing
polycystic ovary syndrome/PCOS- condition which can affect a woman's menstrual cycle, fertility, hormones and aspects of her appearance; it can also affect long-term health
polysomnography- a type of sleep study; a multi-parametric test used in the study of sleep and as a diagnostic tool in sleep medicine
rapid eye movement/REM- stage in the normal sleep cycle during which dreams occur and the body undergoes marked changes including rapid eye movement, loss of reflexes, and increased pulse rate and brain activity
snoring- breathing with a snorting or grunting sound while asleep
tracheostomy- an incision in the windpipe made to relieve an obstruction to breathing
uvulopalatopharyngoplasty/UPPP- surgical resection of unnecessary palatal and oropharyngeal tissue to open the airway; intended to cure extreme cases of snoring (with or without sleep apnea)
References
American Academy of Dental Sleep Medicine; www.aadsm.org. Accessed on October 8, 2014.
Aurora RN, Casey, KR, Kristo D, Auerbach S, Bista SR, Chowdhuri S, Practice parameters for the surgical modifications of the upper airway for obstructive sleep apnea in adults. Sleep, 2010 Oct; 33 (10) 1408-13.
Joshi, Arjun S. “Oral Appliances in Snoring and Obstructive Sleep Apnea” Medscape, www.emedicine.medscape.com, (2013) October 8, 2014.
Reports on Obstructive Sleep Apnea. University of Maryland Medical Center; http://umm.edu. Accessed on October 8, 2014.
Sleep Apnea Dentist; www.sleepapneadentist.com. Accessed on October 8, 2014.
Untreated sleep apnea in children; www.sciencedaily.com, a published study by the Journal of Scientific Reports, March, 2017
Neurology Clinical Practice; www.ncbi.nlm.nih.gov, Easy diagnosis and treatment of OSA after stroke. June, 2013
About the Author
Tija Hunter, CDA, EFDA, FADAA
Tija Hunter, CDA, EFDA, FADAA is a practicing dental assistant/office manager in O'Fallon, Missouri. She is the author of numerous dental articles and continuing education courses. She is a member of the American Dental Assistants Association and sits on the state board in Illinois. She also is a member of several councils of the ADAA. Tija is also the Director of the Dental Careers Institute with five locations throughout the United States.