You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Diabetes is a global epidemic. In 2015, the International Diabetes Federation estimated that 415 million people worldwide were living with diabetes; by 2040 that number is expected to grow to 600 million people.1 National Health and Nutrition Examination Survey data found that between 2011 and 2012 approximately 15% of the population in the United States had diabetes and 40% had prediabetes.2 As potentially half of the patients in a dental practice may have or be at risk of developing diabetes, oral healthcare professionals should understand and be able to communicate the relationship between this disease and oral health.
Understanding the Basics of Diabetes
Individuals with diabetes do not produce enough insulin to regulate their blood glucose levels. Diabetes is most often diagnosed when a patient's A1c, or 3-month blood glucose average, is 6.5% or higher; fasting blood glucose is above 126 mg/dL; or blood glucose is above 200 mg/dL after a 2-hour oral glucose tolerance test. Common symptoms of diabetes include polydipsia, polyuria, polyphagia, unintentional weight loss, fatigue, blurry vision, and difficulty in wound healing.3
The three main types of diabetes are type 1, type 2, and gestational diabetes. Type 1 diabetes is an autoimmune disease affecting approximately 5% to 10% of people with diabetes.3 Unable to produce insulin, these individuals must manage the disease with insulin injections. In addition to the required insulin, lifestyle changes are recommended to help these patients maintain overall health.
Approximately 90% to 95% of people with diabetes have the type 2 variation. Although they can produce insulin, their body does not use it efficiently, resulting in insulin resistance or insulin deficiency.3 Non-modifiable risk factors for type 2 diabetes include age 45 years or older, family history, prediabetes, history of gestational diabetes, and certain ethnicities (African American, Latino, Native American, Asian American, and Pacific Islander). Modifiable risk factors include inactivity, or BMI ≥ 25 (≥ 23 for Asian Americans), blood pressure ≥ 140/90, and dyslipidemia. For this type of diabetes, first-line treatment usually involves lifestyle changes, such as diet and exercise routine. Second-line treatment includes oral medications and insulin as the disease progresses or when blood sugar levels are very high.
Gestational diabetes affects approximately 10% of women who are pregnant.4 Usually diagnosed between the 24th and 28th week of pregnancy, this disease is a result of hormonal changes that increase blood sugar levels and the need for insulin, which the woman is not able to produce sufficiently. The safest, most efficient way to treat these patients is with insulin. Although blood glucose levels typically return to normal after the pregnancy ends, these women remain at a higher risk of developing type 2 diabetes in the future.
Patients with high blood sugar levels who have an increased risk of developing type 2 diabetes are classified as having prediabetes.5 Through lifestyle interventions, such as losing weight, eating healthier, and exercising more, type 2 diabetes may be prevented or delayed. The oral medication metformin may also be prescribed to help regulate blood sugar levels.
Relationship between Diabetes and Oral Health
After a diabetes diagnosis, managing the disease is crucial. Diabetes may result in numerous complications if not well managed: one explanation for this is chronic inflammation.
People with type 2 diabetes are 3 times more likely to develop periodontal disease, which is a chronic inflammatory process that can result in tooth loss, pain, and inflammation.6 The longer a person has diabetes, the higher the chance of developing periodontal disease. Metabolic control, such as higher A1c levels, is a factor in this oral disease.7 Other concurrent factors, such as plaque, poor oral hygiene, smoking, certain medications, and stress, also increase the risk.7
Diabetes may exacerbate oral health problems through a decrease in saliva production, resulting in dry mouth, which increases the risk of dental caries and may impact the types of food a patient consumes. Fluctuations in blood sugar levels can also hinder oral health. High blood sugar impairs wound healing and increases the chance of infections. When blood sugar is low, patients require something to increase their levels quickly—usually a simple carbohydrate such as juice, honey, glucose tablets, or regular soda, all of which can be harmful to teeth.8,9 In addition, to prevent low blood sugar, sometimes patients with diabetes need to eat often. The pH acidity in common interventions for low blood sugar are not conducive to healthy teeth: this increased exposure leads to erosion.
There is also evidence that people with periodontal disease are at a higher risk of developing diabetes. The more severe the periodontitis is, the higher the risk of diabetes and an elevated A1c.10 Periodontitis also increases the risk of developing other diabetes-related complications such as cardio-renal mortality, atherosclerotic plaques, and microalbuminuria.
Preventing complications such as periodontal disease can help patients with diabetes live healthier lives. In 2017, the American Diabetes Association recommended that after an initial diagnosis, patients visit a dentist for a comprehensive checkup to prevent oral complications before problems arise.11
The Nutrition Factor
A healthy diet is important for maintaining systemic health by preventing nutritional deficiencies. For example, if milk or calcium products are not consumed, teeth or bones may become damaged, which in turn affects metabolic diseases. If healthy fats are not consumed, heart and blood pressure may be affected. There is a broad multidisciplinary emphasis on nutrition because of the interrelationships of body systems.
A national study known as the Diabetes Prevention Program found that nutrition, weight loss of 5% to 10%, and exercise of 150 minutes per week can effectively lower the rate of diabetes and delay onset. The report concluded that lifestyle changes are more effective than the drug commonly used for prediabetes, metformin.13
Medical nutrition therapy provides nutritional diagnosis and counseling services for disease management through a registered dietitian or nutritional professional.13 For people with diabetes, medical nutrition therapy can lead to A1c reduction by 0.25% to 3% within 3 to 6 months.13 (Comparatively, a drug is considered effective if it reduces A1c by 0.5%.) Nutrition therapy can also work for other related health conditions, such as low-density lipoprotein, for which it can help lower levels up to 16%.
Although there is clear evidence that medical nutrition therapy can help in the management of some diseases, the benefit for oral health has not been established. Nutrition professionals do not often provide a formal diagnosis or nutrition therapy plan for patients regarding their oral health, limiting clinical evidence. However, even absent the specific clinical benefits of medical nutritional therapy on oral health, it is understood that diet factors, such as limiting sugar to < 10% of daily calories14,15 can promote oral health.
Several dietary factors are associated with oral disease and periodontal health (Table 1).12 For example, acidic foods can cause dental erosion, while fermentable carbohydrates that feed the microorganisms in the mouth cause dental caries.16 Firmer foods that do not adhere to teeth are better for dental health than food that is sticky. Eating foods or chewing gum to promote saliva stimulation can help improve oral health. Finally, food exposure time plays a part: frequency will increase exposure time.
In addition, the nutritional composition of food is important for oral health: many vitamins and minerals are essential12 (Table 2). Overall, these nutrients promote the restoration of bone structures and healthier cell formation.
Oral conditions can lead to poor nutrition, which in turn diminishes oral health. For example, tooth loss can be an indicator of general health, as it may limit the quality of food and the types of nutrients consumed. Oftentimes softer, easier-to-chew items (which may be higher in fat and sugar because of the nature of the food) are chosen instead. In addition, people with dry mouth, or candidiasis, may increase their intake of candies or high-carbohydrate beverages due to pain and discomfort.
Need for Collaboration, Raising Awareness at Dental Offices
The Academy of Nutrition and Dietetics recently released a position statement promoting the interrelationship between nutrition and oral health and a need for collaboration between the fields.12 The statement encouraged these professionals to educate their respective patients how each aspect impacts the other.
The Joslin-Sunstar Diabetes Education Initiative shares up-to-date scientific evidence regarding the bidirectional links between oral and systemic health, which professionals can share among themselves and with their patients. This initiative hopes to reach a wide range of healthcare professionals (including dentists, physicians, dental hygienists, nurses, dietitians, researchers, and pharmacists) through a 1-day program on the pathophysiology of oral disease and diabetes and how they are linked, as well as evidence for prevention. The program provides a platform for medical health and dental professionals to collaborate, and encourages them to refer patients to one another.
Collaboration between oral health and nutritional health professionals will be key in gathering clinical evidence of outcomes. One example of collaboration in action is updating guidelines to recommend diabetes screening at dental practices, and to refer patients with diabetes to dentists for comprehensive examination.17
The Healthy Plate Method is used to encourage a balanced diet. Among other recommendations, this system promotes the consumption of complex, controlled, and consistent carbohydrates, which can prevent fluctuations in blood sugar. Overall, this method helps in ensuring adequate micronutrients for systemic and oral health. In addition, balanced macronutrients help to prevent weight-related diseases, and the resulting oral impacts. Many of the represented foods are also anti-inflammatory. A discussion of the Healthy Plate Method can be incorporated into a dental practice, and patients encouraged to try this approach.
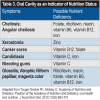
In addition to documenting oral conditions, dental health professionals should take note of nutrient deficiencies during checkups and make recommendations. Potential nutrient deficiencies can be identified by symptoms such as cheilosis in the lips; xerostomia, canker sores, and candidiasis in the mouth; bleeding in the gums; and glossitis, magenta color, and atrophic filiform papillae on the tongue (Table 3).12 Nutrition-related habits also impact oral health in other ways: For example, overweight patients may be consuming higher-calorie and carbohydrate foods, as well as eating more frequently, which exposes their teeth to food for longer periods. Other behaviors, such as reflux or bulimia, can cause enamel erosion.9 When patients show oral warning signs for a nutrition deficiency, they should be referred to a dietitian.
Dentists can implement other clinical and educational tools in their practice to help patients who may be at risk of developing diabetes. Knowledge and awareness is the first step. Although screenings should not be used to diagnosis diabetes, dentists can use these questionnaires to identify patients who are at a higher risk.
If possible, dental hygienists can do a simple blood glucose check and alert patients if their blood sugar level is above 200 mg/dL, as well as encouraging them to visit a physician or dietitian. If a glucose test can not be performed, the team should still educate their patients on the benefits of regular dental appointments and medical checkups.
In addition to educating patients, dentists can also collaborate by sharing the periodontal disease screening tool with medical doctors, so they may evaluate their patients who are at a higher risk of periodontal disease and refer them to a dentist. Medical doctors should also advise their patients about the relationship between oral and overall health, including the oral complications of diabetes.
Diabetes, oral health, and nutrition are interrelated, with inflammation being an important link. By encouraging interventions in these disciplines, oral healthcare professionals have the opportunity to allay diabetes and its complications, along with other related issues, in their patients. By maintaining oral health, patients can lower their risks for certain systemic diseases, and cultivate a healthier lifestyle.
References
1. International Diabetes Federation. IDF Diabetes Atlas, 7th edn. Brussels, Belgium: International Diabetes Federation, 2015.
2. Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988-2012. JAMA. 2015;314(10):1021-1029.
3. American Diabetes Association. 2. Classification and diagnosis of diabetes. Diabetes Care. 2017;40(Suppl 1)S11-S24.
4. DeSisto CL, Kim SY, Sharma AJ. Prevalence estimates of gestational diabetes mellitus in the United States, Pregnancy Risk Assessment Monitoring System (PRAMS), 2007-2010. Prev Chronic Dis. 2014;11:E104.
5.American Diabetes Association. Diagnosing Diabetes and Learning about Prediabetes. http://www.diabetes.org/diabetes-basics/diagnosis. Accessed November 2, 2017.
6. Chapple IL. Potential mechanisms underpinning the nutritional modulation of periodontal inflammation. J Am Dent Assoc. 2009;140(2):178-184 .
7. Ryan ME, Carnu O, Kamer A. The influence of diabetes on the periodontal tissues. J Am Dent Assoc. 2003;134(Spec No): 34S-40S.
8. Bowen WH, Lawrence RA. Comparison of the cariogenicity of cola, honey, cow milk, human milk, and sucrose. Pediatrics. 2005;116(4):921-926.
9. Saeed S, Al-Tinawi M. Evaluation of acidity and total sugar content of children's popular beverages and their effect on plaque pH. J Indian Soc Pedod Prev Dent. 2010;28(3):189-192.
10. Chapple IL, Genco R; working group 2 of the joint EFP/AAP workshop. Diabetes and periodontal diseases: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J Periodontal. 2013;84(4 Suppl):S106-S112.
11. American Dental Association. For the dental patient. Diabetes: tips for good oral health. J Am Dent Assoc. 2010;141(7):926.
12. American Diabetes Association. Standards of Medical Care in Diabetes—2009. Diabetes Care. 2009;32(Suppl 1):S13-S61.
13.Bantle JP, Wylie-Rosett J, Albright AL, et al. Nutrition recommendations and interventions for diabetes–2006: a position statement of the American Diabetes Association. Diabetes Care. 2006;29(9):2140-2157.
14. Moynihan P, Petersen PE. Diet, nutrition and the prevention of dental diseases. Public Health Nutr. 2004;7(1A):201-226.
15. Moynihan PJ. The role of diet and nutrition in the etiology and prevention of oral diseases. Bulletin of the World Health Organization. 2005;83(9):694-699.
16. Velan E, Nelson T. Evaluating caries risk. Dimensions of Dental Hygiene. 2014;12(2):53-59.
17. American Diabetes Association. Standards of Medical Care in Diabetes - 2017. Diabetes Care. 2017;40(suppl 1):S4-S5.