You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Improving the population's oral health and eliminating oral health disparities is an important public health and health system priority.1,2 Fifteen years after the Surgeon General's report,2 oral health disparities persist in the United States (US). Poor oral health may lead to life-long problems; for instance, dental diseases are a leading cause of student absenteeism and predict poorer performance on standardized assessments.3,4 Adults with poor oral health are less likely to be employed than those with good oral health5 and are more likely to develop serious health conditions and chronic diseases.6-8
Almost all dental diseases are preventable. Dental disease prevention and management is critical in improving oral health and reducing oral healthcare delivery costs in the US.9 Preventive clinical interventions are effective (e.g., the topical application of fluoride varnish and dental sealants); however, discrepancies in access to these interventions limit their diffusion and perpetuate oral health disparities.
Numerous factors affect patients' access to care; however, access depends on oral healthcare professionals' service delivery.2 Dental hygienists are responsible for dental disease prevention, oral health promotion, and periodontal disease management. This workforce may effectively improve access to services that reduce oral health disparities (e.g., preventive dental procedures).10,11 In a study examining low-income children in a school setting, the number of dental hygienist encounters was inversely correlated with number of children with dental decay and urgent dental needs.10 Regarding mid-level dental practitioner models, a health care professional with prophylaxis training (e.g., a dental hygienist) may provide most dental care services offered in community-based settings.11 These findings collectively suggest that dental hygienists may improve access to oral healthcare services; however, it is important to note that previous findings reflect examination of individual workforce models within particular communities and states. They may not be generalizable due to variations in organizational, local, or state workforce policies.
Dental hygiene education is nationally standardized; however, at the state level, professional licensing boards' statutes and regulations govern professional practice.12 State policies dictate dental hygienists' permitted clinical tasks, professional supervision requirements, professional governance, and Medicaid reimbursement terms.13 These policies are documented in the Dental Hygiene Professional Practice Index (DHPPI), originally developed in 2001 by the Health Resources and Services Administration (HRSA) and updated in 2014. In the DHPPI, states are assigned numeric values and categorized based on the level of professional independence afforded to the dental hygiene workforce.13 Professional practice environments vary between states. For example, in states supporting professional independence, dental hygienists may serve as independent oral healthcare access points, whereas in states restricting such independence, dental hygienists may only practice at existing points of care, generally under a licensed dentist's supervision. Claims that such practice restrictions protect public safety are poorly supported.14 Additionally, state support for professional independence predicts dental care access.15,16 Moreover, variations in state regulation of the dental hygiene workforce affect the capacity of the dental safety net, which supports the oral healthcare needs of underserved individuals.
State regulation of the dental hygiene workforce is associated with oral health service availability within the dental safety net17; this association has been supported regarding Federally Qualified Health Centers (FQHCs; a critical component of the dental safety net).18,19 Federal funding agreements require all FQHCs to ensure that community members have access to “preventive dental services”20; however, the state-level professional practice environments for dental hygienists continue to apply to FQHCs. Thus, federal and state policies intersect at FQHCs, thereby permitting examination of state workforce policies' impact on oral healthcare availability and access. Restriction of professional independence appears to predict reduced delivery of dental services.17 Empirically supporting this relationship's existence may lead to improved dental care availability in underserved communities; however, demonstrating access requires the examination of service use, rather than resource availability.21 The purpose of this study was to examine whether state policies regulating the dental hygiene workforce affected FQHC patients' actual access to dental care in order to inform policies aimed towards improving the population's oral health.
Methods
This study used an adaptation of Aday and Andersen's Framework for the Study of Access to Medical Care to study state workforce policies' effect on oral healthcare access.17 In this framework, FQHCs represent an allocative health policy that aims to affect the volume and distribution of oral health services in underserved communities; however, it should be noted that FQHCs must deliver care that is within the context of their particular state. Therefore, the authors theorized that state workforce policies are likely to influence FQHCs' ability to provide dental services and thereby affect care access.
This study examined longitudinal data on 958 FQHC grantees located in the 50 states and the District of Columbia that received community health center funding from the U.S. Health Center Program from 2004 to 2012. It is important to note that one grantee may operate in multiple locations within their service area. Federal funding agreements require FQHC grantees to report administrative and patient utilization data to the Uniform Data System (UDS) on an annual basis. UDS data for this study were obtained through a Freedom of Information Act (FOIA) request.
Outcome Measure
Dental care access among FQHC patients was the outcome of interest; this was defined as the proportion of unique FQHC patients that had a dental examination at the FQHC grantee within a reporting year. Dental examinations are generally required before initiation of dental treatment in traditional dental settings. Therefore, the dental examination was considered a reasonable proxy measure for access to oral health care at FQHCs. FQHC grantees report the total number of unique patients as well as the number of unique patients by procedure, using Current Dental Terminology (CDT) codes. The following CDT codes are defined as dental examinations in the UDS: D0120, D0140, D0145, D0150, D0160, D0170, and D0180.22 FQHC patients are reported as having had a dental examination if they had a visit associated with any of the aforementioned CDT codes during a reporting year. The proportion of FQHC patients accessing dental care was calculated by dividing the total number of unique FQHC patients reported as having a dental examination by the total number of unique patients at the FQHC within a reporting year.
Primary Independent Measure
The primary independent variable was the Dental Hygiene Professional Practice Index (DHPPI); this constituted a baseline measure of state policy environments. The DHPPI was analyzed as a five level categorical variable (5 = most supportive policy environment, 1 = most restrictive).
The following limitations were addressed in the DHPPI before using it in the analysis. First, many states changed their relevant dental hygiene policies from 2001 to 2012; this was likely to affect state-level professional practice and oral healthcare access. To account for any effects of such changes, all relevant policy changes that occurred between 2002 and 2011 were identified and a subsequent binary, state-level variable was generated and included in the analysis. Additional information regarding the identification of these changes and coding of this variable may be found in the technical appendix. Second, the DHPPI quantifies professional practice environments for dental hygienists based on state policies; this may not accurately represent dental hygienists' practice. Therefore, the DHPPI data was considered to represent state-policy context, rather than dental hygienists' practice. A more detailed description of the DHPPI is provided in Appendix A.
Covariates
Covariates were FQHC grantee level administrative and aggregate patient characteristics drawn from the UDS for each year included in the study; specifically, the number of clinical sites operated by a given FQHC, the geographic location primarily served by the FQHC, and the proportions of patients who are uninsured, Medicaid recipients, percent in poverty, or members of racial and ethnic minority groups. A variable (time) representing FQHCs' duration of receiving funding was also generated to control for funding duration's effect on care access in the multivariable models: A value of 1 was assigned to each FQHC in the first year it received funding; this value increased by 1 for each subsequent year the FQHC continued to receive funding. A complete list of study variables with associated definitions and values can be found in Appendix B, Table VI.
Analysis
Continuous variables are described using means and standard deviations (SDs) and categorical variables are described using frequencies and percentages. Longitudinal profiles of dental care access in FQHCs were modeled using linear mixed-effects models. Random intercepts were adopted at both the state and FQHC levels to account for within-state and within-FQHC correlations. Univariate regressions were conducted to evaluate unadjusted associations between the outcome and predictors. A backward model selection was subsequently adopted to identify the best multivariate model for evaluating the adjusted associations. Two-sided p-values <0.05 were considered statistically significant. All statistical analysis was performed using SAS© version 9.3 (SAS Institute, Cary, NC, USA).
Results
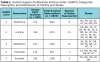
Table I presents the number of unique FQHC grantees, the number of FQHC observations (total number of FQHC grantees observations across all years), and states by DHPPI category. A total of 6,830 observations were collected dating from 2004 to 2012. The “limiting” DHPPI category (i.e., the second-most restrictive policy environment) contained the largest number of FQHCs grantees, observations, and states.
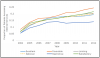
Table II presents statistics describing FQHC grantees' characteristics and the univariate regression analyses' results, as well as the proportion of patients accessing dental care by DHPPI category and where appropriate. In general, a greater proportion of FQHC patients accessed dental care in states with more supportive policy environments. States categorized as “favorable” and “restrictive” contained the largest and smallest proportion of patients accessing dental care, respectively (18% and 12%); this finding was consistent for all years. Approximately 6% fewer (-0.056, 0.046) patients access dental care at FQHC grantees located in the most restrictive states as compared to those located in states categorized as excellent (used as reference in descriptive analyses). Dental care access among FQHC patients increased consistently across all DHPPI categories over the study period; consistently, the highest and lowest proportions of FQHC patients accessing dental services were in favorable and restrictive states, respectively (Figure 1). The gap in proportions between favorable and restrictive states increased over the study period. In 2012, 24.3% and 13.9% of patients in favorable and restrictive states were accessing dental care, respectively. Nationally, 19.9% of FQHC patients accessed dental care at FQHCs in 2012.
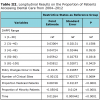
In the longitudinal regression analysis, after adjusting for numerous factors, 6% more patients accessed dental services at FQHCs in favorable or “excellent” states than in restrictive states (“excellent” refers to the most supportive policy environment) (Table III). The proportion of Medicaid patients (0.09, P<0.0001) and minority patients (-0.5, P<0.0001) predicted the proportion of patients accessing dental services within FQHCs. The proportion of patients accessing dental services increased significantly or each additional year of funding (0.01, P<0.001).
Discussion
The results of this study suggest that state regulation of the dental hygiene workforce is likely associated with access to dental care among patients of FQHCs. Further, findings suggest that dental hygienists likely facilitate access to dental services at FQHCs; demonstrated in the finding that fewer patients accessed dental care at FQHCs located in restrictive states.
The results do not indicate whether state policies (as quantified by the DHPPI) independently affect oral healthcare service access or if another underlying factor is correlated with DHPPI and affects care access. Nonetheless, the present results support previous research indicating state regulation's effect on dental care access in the general population15,16 and among underserved individuals.17 The present results suggest that state policies affect underserved individuals' access to dental care and oral healthcare services' availability in FQHCs.
The study examined the proportion of FQHC patients accessing dental care in 2012 in order to contextualize the present findings. In 2012, approximately 2.1 million people visited FQHCs located in restrictive states; 286,769 of these subsequently received dental care (13.9%). In contrast, in the same year, approximately 2.7 million people visited FQHCs located in favorable states, 663,614 of whom subsequently received dental care (24.3%; a difference of 376,845 people). In 2012, approximately 18.3 nationwide, whereas 3.7 million accessed dental care at FQHCs (approximately 20%); the remaining 14.7 million people may lack access to recommended preventive dental care.23
FQHC patients in restrictive states may access dental services outside of their local FQHC; however, this is unlikely to be true of all patients. FQHCs are located in urban and rural communities designated as “medically underserved areas” by the federal government24; these communities are characterized by recognized and significant shortages in healthcare resources. Individuals in these communities face significant barriers to dental care access (e.g., transportation issues, inability to take time off work, dental care costs).18, 25-27
State policies appear associated with underserved individuals' access to dental care. The present findings do not indicate if this relationship is causal; however, restrictive state policies may limit dental healthcare professionals' ability to provide dental care. For example, FQHCs located in Mississippi (a restrictive state) cannot provide or bill for preventive dental services delivered by a dental hygienist unless the hygienist is directly supervised by a licensed dentist. In contrast, FQHCs in Maine (a favorable state) may do so without dental oversight. In Colorado (an excellent state), FQHCs may bill for dental services provided by dental hygienists, allowing FQHCs to employ dental hygienists in their primary care clinics and thereby provide preventive dental care and education. This allows patients to access several types of preventive care in one visit and increases patients' access to care. Conversely, in Kentucky (a restrictive state), FQHCs cannot employ dental hygienists or bill for dental services without concurrently employing a supervising dentist.28 FQHCs in Kentucky that do not employ dental professionals may refer patients requiring dental services to affiliated dental practices rather than directly providing such services; however, a study conducted at one FQHC found that relatively few referrals led to dental visits and many patients did not receive dental care.28 Future research should further examine state policies' effect on delivery of dental services at FQHCs and subsequent access to dental care.
Limitations
This study has the following limitations. As mentioned above, some key data could not be obtained and some assumptions were not robustly supported (e.g., that the DHPPI accurately represents state-level professional practice environments for dental hygienists). Additionally, data were not available regarding some potentially confounding state- and FQHC-level factors (e.g., Medicaid policies, patient encounter rates). The authors managed this limitation by adjusting for random effects at the state and FQHC levels; however, future research should test the present findings using additional FQHC-level data from the U.S. Health Center Program in order to more validly assess state policy's effect on FQHCs.
Furthermore, FQHC grantee-level information was subject to a number of limitations. The authors could not obtain data indicating the number of healthcare professionals (including dental professionals) practicing in each FQHC using a FOIA request because it is considered proprietary information. Therefore, the analysis could not adjust for variations in dental workforce capacity at the FQHC level. In order to account for, to some extent, dental workforce capacity within a state, state level dentist per capita data were included in exploratory analyses and considered during preliminary model construction. Dentist per capita was ultimately excluded in the final statistical models, as it was not statistically significant or correlated with study outcomes. Appendix B lists all independent variables and covariates included in the final statistical models for this study.
New and innovative workforce models that delivery oral health care in non-traditional settings (i.e. school-based, nursing communities, etc.) are emerging across the country and may contribute to improved access to preventive oral health care. These non-traditional models may or may not operate in similar fashion to more traditional oral health care delivery models. For example, patients receiving school-based oral health care may or may not have a dental examination prior to receiving preventive services such as fluoride varnish or prophylaxis. However, in more traditional settings (i.e. FQCHs or dental offices) dental examinations are typically administered prior to receipt of additional preventive or restorative services. Recognizing these differences, it is important that these findings be considered and interpreted within the context of the research objectives, which as to determine how state scope of practice policies affect FQHC patients' access to oral health care services as measured by dental examinations. Future studies that both qualitatively and quantitatively evaluate how state scope of practice regulations affect non-traditional models of oral health care delivery as well as various types of preventive oral health services would fill an important gap that currently exists in this area of research.
Policy implications
The present findings make a valuable contribution to public health research and constitute an initial examination of state workforce policies' relationship with underserved individuals' access to oral healthcare services. Accordingly, these findings have the following implications. Regarding FQHCs, the findings indicate the necessity of improving FQHC productivity, which is critical to increasing dental safety-net capacity.29,31 Simultaneously, preventing and managing dental disease may most effectively reduce oral health disparity.9 Better alignment between FQHCs' dental service requirements and dental hygienists' professional focus will allow dental hygienists at FQHCs to better increase access to dental services. Numerous FQHCs are pursuing such alignment by embedding dental hygienists in their primary care clinics in order to expand preventive services for patients29 or by employing dental hygienists in school-based dental programs to expand the reach of particular preventive services (e.g., dental sealant application).32 Of course, FQHCs may only employ such models if state policies permit dental hygienists to function in these capacities.
Regarding state policy, the present findings may promote discussion between lawmakers and oral healthcare providers regarding optimization of state workforce policies to ensure public safety without impeding underserved populations' oral healthcare access. The study found that 20% of FQHC patients nationwide receive dental care from FQHCs, which indicates the importance of such discussions and may suggest that the use of dental hygienists to address this ongoing public health issue may be promising.
Finally, regarding federal policy, the HRSA might consider collaborating with key researchers to better understand each state policy's effect on underserved patients' access to oral healthcare and advocate for better access to the FQHC data necessary to further examining this relationship. Federal officials should consider the potential funding issues stemming from the intersection of state workforce policies and federal public health programs. Specifically, the federal government mandates that a health center's funding application shall not be granted unless it shows that “the required primary health services of the center will be available and accessible in the catchment area of the center promptly …” (emphasis added).20 Therefore, FQHCs in a restrictive policy environment that cannot promptly provide “preventive dental services” (which comprise one of the required primary health services)20 to patients in their catchment area via referrals are not productively using their allocated federal funds to deliver dental services to underserved community members. Failure to provide care to underserved individuals increases the cost of emergency and restorative dental procedures to those individuals. In summary, the present results suggest that restrictive state policies impede the implementation of federal health system priorities such as decreasing the cost and increasing the quality and availability of care.33
Conclusion
Improving underserved communities' access to oral healthcare services is a public health priority. Most dental diseases are preventable; however, disparities in access to oral healthcare make it difficult for underserved individuals to benefit from receipt of dental services. Therefore, states should consider supporting the dental hygiene workforce's ability to improve FQHC patients' access to dental examinations, which generally precede additional dental services. Currently, state workforce policies often limit dental hygienists' ability to efficiently deliver oral health services to the largest possible number of people. Federal and state officials and healthcare professionals should optimize these policies in order to maximize public safety and ensure that the healthcare workforce can provide important dental services such as dental examinations within FQHCs.
Acknowledgements
The authors acknowledge the Health Resources Services Administration of the Department of Health and Human Services for assistance in obtaining the data examined in this study. In addition, they acknowledge the Center for Health Workforce Studies at the State University of New York in Albany and the American Dental Hygienists' Association for the technical assistance provided in reference to examining state policy environments.
About the Authors
Hannah L. Maxey, RDH, MPH, PhD is the director, health workforce studies and assistant professor of family medicine; Connor W. Norwood, MHA, PhD is a research associate and assistant director of health workforce research and policy; Johannah B. O'Connell, JD is a former research associate; all at the Bowen Center for Health Workforce Research and Policy, Indiana University School of Medicine, Indianapolis, IN.
Ziyue Liu, PhD is an assistant professor, Department of Biostatistics, Indiana University Richard M. Fairbanks School of Public Health, Indianapolis, IN.
References
1. Institute of Medicine. Advancing Oral Health in America. Washington, DC: National Academies Press; 2011: 1-4.
2. U.S. Department of Health and Human Services. Oral health in America: a report of the surgeon general. Rockville, MD: U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000: 1-322.
3. Guarnizo-Herreño CC, Wehby GL. Children's dental health, school performance, and psychosocial well-being. J Pediatr. 2012 Oct;161(6):1153-1159. e1152.
4. Seirawan H, Faust S, Mulligan R. The Impact of oral health on the academic performance of
disadvantaged children. Am J Pub Health. 2012 Sep;102(9):1729-1734.
5. Gift HC, Reisine ST, Larach DC. The social impact of dental problems and visits. Am J Pub Health. 1992 Dec;82(12):1663-68.
6. Pace CC, McCullough GH. The association between oral microorganisms and aspiration pneumonia in the institutionalized elderly: review and recommendations. Dysphagia. 2010 Sep;25(4):307-322.
7. Sfyroeras GS, Roussas N, Saleptsis VG, et al. Association between periodontal disease and stroke. J Vasc Surg. 2012 Apr;55(4):1178-84.
8. Lamster IB, Lalla E, Borgnakke WS, et al. The relationship between oral health and diabetes mellitus. J Am Dent Assoc. 2008 Oct;Suppl 139:19S-24S.
9. Edelstein B. The dental safety net, its workforce, and policy recommendations for its enhancement. J Public Health Dent. 2010 Jun;70 Suppl 1:S32-39.
10. Simmer-Beck M, Walker M, Gadbury-Amyot C, et al. Effectiveness of an alternative dental workforce model on the oral health of low-income children in a school-based setting. Am J Pub Health. 2015 Sep;105(9):1763-69.
11. Phillips E, Gwozdek AE, Shaefer HL. Safety net care and midlevel dental practitioners: a case study of the portion of care that might be performed under various setting and scope-of-practice assumptions. Am J Pub Health. 2015 Sep;105(9):1770-76.
12. McKinnon M, Luke G, Bresch J, et al. Emerging allied dental workforce models: considerations for academic dental institutions. J Dent Educ. 2007 Nov;71(11):1476-91.
13. National Center for Health Workforce Analysis. The professional practice environment of dental hygienists in the fifty states and the District of Columbia, 2001. Washington, D.C.: Health Resources and Services Administration; 2004:1-202.
14. North Carolina State Board of Dental Examiners v. Federal Trade Commission, 135 US 1101, 1109 (2015).
15. Wanchek T. Dental hygiene regulation and access to oral healthcare: assessing the variation across the US states. Br J Ind Relat. 2010 Dec;48(4):706-25.
16. Wing P, Langelier MH, Continelli TA, et al. A dental hygiene professional practice index (DHPPI) and access to oral health status and service use in the united states. J Dent Hyg. 2005 Spring;79(2):1-10.
17. Maxey HL, Norwood CW, Liu Z. State policy environment and the dental safety-net: a case study of professional practice environments' effect on dental service availability in Federally Qualified Health Centers. J Pub Health Dent. 2015 April;76(4):295-302.
18. Jones E, Shi L, Hayashi AS, et al. Access to oral health care: the role of federally qualified health centers in addressing disparities and expanding access. Am J Public Health. 2013 Mar;103(3):488-493.
19. Donabedian A. Aspects of medical care administration: specifying requirements for health care. Cambridge, MA: Harvard University Press; 1973: 1-800.
20. Public Health Services Act (PHS) 42 U.S.C.Sect. 330 (1944).
21. Donabedian A. Models for organizing the delivery of personal health services and criteria for evaluating them. Milbank Q. 1972 Oct;50(4):103-154.
22. American Dental Association. CDT 2011-2012: current dental terminology: the ADA practical guide to dental procedure codes. 1 ed. Chicago, IL; American Dental Association: 2012: 1-297.
23. Health Resources and Services Administration: Oral Health [Internet]. Rockville (MD): Department of Health and Human Services; [modified 2017 May; reviewed 2018 Feb 16]. Available from: http://www.hrsa.gov/publichealth/clinical/oralhealth/
24. Health Resources and Services Administration. Medically Underserved Areas/Populations. Guidelines for MUA and MUP Designation [Internet]. Rockville (MD): Department of Health and Human Services; [modified 2017 May; reviewed 2018 Feb 16]. Available from: http://www.hrsa.gov/shortage/mua/
25. Mofidi M, Rozier RG, King RS. Problems with access to dental care for Medicaid-insured children: what caregivers think. Am J Pub Health. 2002 Jan;92(1):53-58.
26. Pourat N, Martinez A, Crall J. Better together: co-location of dental and primary care provides opportunities to improve oral health. Los Angeles, CA: UCLA Center for Health Policy Research; 2015: 1-8.
27. Pourat N, Finocchio L. Racial and ethnic disparities in dental care for publicly insured children. Health Aff (Milwood). 2010 Jul;29(7):1356-63.
28. Maxey HL. Integration of oral health with primary care in health centers: profiles of five innovative models. Bethesda, MD: National Association of Community Health Centers; 2015: 1-27.
29. Bailit H, D'Adamo J. State case studies: improving access to dental care for the underserved. J Public Health Dent. 2012 Summer;72(3):221-34.
30. Bureau of Primary Health Care. Program Requirements [Internet]. Rockville (MD): Health Resources and Services Administration; [modified 2015 May; reviewed 2015 Aug 15]. Available from: https://bphc.hrsa.gov/programrequirements/policies/index.html
31. Bailit H, Beazoglou T, Demby N, et al. Dental safety net: current capacity and potential for expansion. J Am Dent Assoc. 2006 Jun;137(6):807-15.
32. Bailit H, Beazoglou T, Drozdowski M. Financial feasibility of a model school-based dental program in different states. Public Health Rep. 2008 Nov-Dec;123(6):761-67.
33. Public Health Services Act (PHS) 42 U.S.C. Sect. 330 (1944).
34. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008 May-Jun;27(3):759-69.
APPENDIX A: Dental Hygiene Professional Practice Index (DHPPI)
The Dental Hygiene Professional Practice Index (DHPPI) contains values representing the professional practice of dental hygienists in the 50 states and the District of Columbia as of 2001. It was developed by the Center for Health Workforce Studies at the State of New York at Albany (SUNY) for Health Resources Services Administration (HRSA).1
DHPPI summarizes and quantifies the four aspects of legal practice environment of dental hygienists: legal and regulatory environment; supervision in various practice settings; tasks permitted under various levels of supervision; and, reimbursement environment. Legal requirements (as of December 31, 2001) for the provision of dental hygiene services across the states are sought to generate values for each of the four aspects. The total index value reflects the sum of values for the four aspects. The influence of each aspect is not distributed equally, as maximum values are assigned for each aspect based on predefined level of importance. Higher values in a category are associated with more supportive environment. The breakdown of these values is as follows: 10 points for legal and regulatory environment; 47 points for supervision; 28 points for tasks permitted; and, 15 points for reimbursement environment. DHPPI values are also grouped into 5 policy categories: restrictive, 0-29; limiting, 30-39; satisfactory 40-49; favorable, 50-79; and, excellent, 80-100. Complete methodology for the DHPPI was published in the final report, The Professional Practice Environment of Dental Hygienists in the Fifty States and the District of Columbia, 2001, in April of 2004 and is available to the public through HRSA at: http://bhpr.hrsa.gov/healthworkforce1/reports/dentalhygiene50statesdc.pdf.
Key Legislative Changes Following DHPPI Development
The DHPPI was developed based on legislative data collected in 2001. Thus, the DHPPI reflects a cross-section of the professional practice environment of dental hygienists at the state level. A number of states experienced changes in legislation for dental hygiene supervision, reimbursement, and scope of clinical practice following the development of the DHPPI (Table IV). These changes are likely to alter the DHPPI; however, it is unlikely legislative changes have an immediate impact on oral health service delivery within a HC grantee due to the nature of the legislative processes in most states.
The American Dental Hygienists Association (ADHA) has collected information annually on state level legislative changes since 2002, specifically the data track bills that have been signed into law by state Governors. This includes information on reimbursement policies, supervision requirements, and scope of clinical practice. This information was obtained from ADHA's legislative liaison, Daniel Zurawski, on September 16, 2013 for the purpose of this study.
Changes in the legislative environment of a state following the development of the DHPPI may affect the delivery of oral health care services in HC grantees over the study period. In order to control for changes, ADHA legislative data are used to generate legislative change variable. Changes are identified by year for each state. A total of nine legislative change variables are created: 8 variables representing state-level changes for each year of the study and 1 variable representing any legislative changes within a state during the 8-year period. States with legislative changes are coded as 1 and states without change are coded as zero.
Ideally, the DHPPI or another indicator of the political practice environment should be updated on an annual basis. Unfortunately, the DHPPI index has not been routinely updated as it requires a significant amount of resources (time and manpower) which have not been readily available. This study examines DHPPI values as a baseline measurement of state policy environment, controlling for key changes in the policy environment. Updating the DHPPI is outside of the scope of this study; however, the development of an index which could be updated annually may be warranted, if the legislative change variables included in this study as covariates have a significant impact.
The following summarize states with key policy (statute or regulatory) changes following the development of the Dental Hygiene Professional Practice Index (DHPPI). This index was developed based on the state level policy environment in 2001. Domains of interest in this study include supervision requirement, scope of clinical practice, and Medicaid reimbursement. These were selected because they (1) are included in the DHPPI (Wing et al., 2005) and (2) have been identified to have direct influence on the dental hygiene labor market and access to oral health care within a state (Wanchek, 2010; Wing et al., 2005).
Supervision requirements are defined as the level of professional oversight required for the clinical practice of dental hygiene. Generally, oversight by a licensed dentist is the most common supervision requirement. There is a large range in the level oversight required. For example, in Colorado there are currently no supervision requirements for delivery of basic dental hygiene procedures (with the exception of the administration of local anesthesia). Whereas in Mississippi, direct oversight by a licensed dentist is required for all clinical dental hygiene services. The DHPPI measured level of supervision within a state using discrete values. Changes in the level of supervision are important; however, this study seeks to identify change in supervision requirement as a two level variable (yes/no). All legislative changes reviewed for this study included provisions that increased professional autonomy for dental hygienists within a state. Thus, policy changes would be associated with an increase in the value of the respective aspects (supervision, tasks, etc.) addressed and the total DHPPI value. This two level variable will be used as a covariate in statistical analyses to control for policy changes in cross-sectional and longitudinal analyses.
The DHPPI includes professional regulation as a fourth domain. The structure of professional governance, state board, is the primary measure for regulation within a state. This is included in the DHPPI as an important measure of the level of professional autonomy within a state; however, it is unlikely changes in the regulatory structure within a state translate directly to changes in delivery of care by dental hygienists. Rather, these changes are likely to be precursory to changes in the other measures (supervision, scope of clinical practice, and Medicaid reimbursement). As changes to governance structures are not considered to have a direct effect on the clinical practice of dental hygiene, they are not included among those changes that are controlled in analyses of this study.
Table V lists the states in which policy changes occur by aspect (supervision, clinical tasks, reimbursements, any). A total of 36 states had policy changes between 2002 and 2011. The majority, 27 states, had changes to supervision requirements, and 17 states had changes to clinical tasks. Only three states had changes to reimbursement policy. Nine states had changes in more than one of the policy aspects during this time period. Changes included in this study are summarized by year.
2003: November 2002 - July 2003
Among the states with key policy changes in supervision requirements during this time period are Illinois, Kansas, Maryland, Minnesota, Oklahoma, South Carolina, and Virginia. Illinois, Kansas and Minnesota introduced policy specific to public health settings, such as federally qualified health centers. North Dakota and West Virginia had changes in scope of practice policy. New Mexico had changes to reimbursement policy which enabled direct reimbursement to dental hygienists for unsupervised dental hygiene care.
2004: August 2003 – September 2004
Arizona, Idaho, Illinois, and the District of Columbia had changes in supervision requirements during this period. Of these, Arizona's policies were specifically aimed at reducing barriers to dental hygiene practice in public health settings, such as federally qualified health centers. In addition, Michigan and Tennessee had changes within scope of clinical practice policy.
2005: January –November 2005
Michigan was the only state to have changes to supervision requirements during this period. These changes were directly focused on reducing supervision requirements in public health settings, such as federally qualified health centers. Connecticut, Massachusetts, Maine, and Minnesota had changes in scope of practice during this period.
2006: January – June 2006
Arizona, Florida, and Rhode Island had changes to supervision requirements during this time period. Policy changes in Arizona and Florida were specifically focused on public health settings. In Rhode Island, policy changes were directed toward care for the elderly through reducing supervision requirements in nursing homes. New Hampshire, Ohio and Virginia had changes in scope of clinical practice. Wisconsin policy changes enabled direct reimbursement to dental hygienists for specified services only.
2007: July 2006 – June 2007
A number of states had key policy changes during this period. California, Indiana, Kansas, Louisiana, Maryland, Nebraska, North Carolina, North Dakota, Rhode Island, and Washington all had changes to supervision requirements. Among these, Kansas, Louisiana, Nebraska, and North Carolina policy changes specified decreased levels of supervision within public health setting, which included federally qualified health centers. A number of the supervision changes also permitted lower levels of supervision for the provision of care to the elderly in nursing homes and senior centers. In addition, a number of states had policy changes which expanded scope of clinical practice, including Minnesota, Louisiana, Maryland, Oregon, and Virginia. Most notable among these are Oregon and Minnesota which incorporated dental hygiene diagnosis or examination into the scope of clinical practice. Wisconsin had changes in reimbursement policy which enabled direct reimbursement to dental hygienists for the delivery of any dental hygiene service.
2008: September 2007 - July 2008
Arkansas, Indiana, Maine, Maryland, Pennsylvania, Vermont had changes to supervision requirement policies. All of these changes included reducing the level of supervision required within public health settings. Although variability in these changes were large; for example, Indiana required examination by a dentist within 45 days of dental hygiene care, while Vermont and Arkansas supervision only required patient chart review or collaborative agreement with a dentist and not a physical oversight examination. In addition, Arkansas and Tennessee had changes to scope of clinical practice.
2009: July 2008 - June 2009
During this time period Arkansas, Massachusetts, Texas, Virginia, Washington, and West Virginia had changes to supervision requirements. Massachusetts, Texas and West Virginia specified policy changes reducing the amount of supervision required in federally qualified health centers. Colorado, Kentucky, and Maryland had changes to scope of clinical practice during this period. Of note, Massachusetts policy changes also enabled Medicaid reimbursement direct to dental hygienists practicing in underserved areas.
2010: July 2009 - June 2010
Kentucky, Maryland, and Ohio had changes to supervision regulation during this period. Maryland policy changes were focused on long-term care facilities. Louisiana and Missouri had policy changes involving scope of practice.
2011: July 2010 – June 2011
Arkansas, Florida, and South Dakota had supervision requirement changes during this time period. Of note, Florida statute included physicians as providing professional oversight for dental hygienists. New Hampshire, Oregon, Indiana, and Ohio had changes to scope of practice statute or rules during this period. Maine had changes to Medicaid reimbursement (MaineCare) enabling direct reimbursement for dental hygiene services.
This study examines DHPPI values as a base-line measurement of state policy environment, controlling for key changes in the policy over the study period. The binary variable for policy change will be used as a covariate in statistical analyses to control for policy changes in cross-sectional and longitudinal analyses.