You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
GLOSSARY
Adjuvant – a drug or agent added to another drug or agent to enhance its medical effectiveness
Aerosol transmissible diseases (ATD) – diseases transmitted by airborne infectious particles smaller than droplets that may remain suspended for periods of time – even days
Antigenic – capable of causing the production of an antibody
Antigenic drift – occurring in both influenza A and B, this involves an accumulation of variations, allowing the virus to mutate making it easier for them to spread throughout a partially immune population
Antigenic shift – a sudden change resulting from the recombination of two virus strains; associated with pandemics due to lack of immunity
Asymptomatic – condition without symptoms
ATD screening – identification of potential ATD cases through readily observable signs and the self-report of patients to determine the appropriateness of treating the patient at that time; screening should be performed prior to treatment
Avian flu – a subtype of influenza type A that was identified in 2003 and continues to infect birds; this subtype has the potential to cause a human pandemic if it mutates to a form that can be transmitted easily between humans
CDC – Centers for Disease Control www.cdc.gov.
Cilia – a microscopic hairlike process extending from a cell
Droplets – respiratory and oral particles larger than 5 microns in diameter generated by coughing, sneezing, talking or by splatter-producing procedures, such as dentistry
Febrile – pertaining to a fever; symptoms of a fever
Flu – commonly used term for influenza
HPAI – highly pathogenic avian influenza
Influenza – acute respiratory viral illness characterized by fever, headache, myalgia (muscle aches), exhaustion, sore throat and cough; some patients suffer nausea, vomiting and diarrhea; symptoms usually last about 7 days, but may last much longer, and may be confused with other illnesses; complications include acute viral pneumonia, secondary bacterial pneumonia and sometimes death
Influenza epidemic – widespread, rapid transmission of influenza infection throughout a population
Influenza pandemic – worldwide spread of a new (novel) subtype or one that has not circulated among humans for a long time; may cause severe infection, illness and death because of its virulence and because people have little or no immunity to the pathogen
NIH – National Institutes of Health
Novel influenza – “new” influenza virus to which people have little or no natural immunity
Pathogen – agent that causes disease
Respiratory Hygiene/Cough Etiquette in Health Care Settings – CDC, November 4, 2004, hereby incorporated by reference for the sole purpose of establishing requirements for source control procedures
RNA – ribonucleic acid
Standard precautions – term used in infection control to identify a standard of care in which all blood or any other body fluid, excretion, or secretion (except sweat), non-intact skin or mucous membranes, regardless of whether they contain blood, are treated as infectious
WHO – World Health Organization
BACKGROUND
Influenza, more commonly called “the flu,” spreads rapidly through populations each year during colder months bringing seasonal flu. Flu season usually begins in the fall and peaks in the months of January and February. However, there have been times with the flu has started as early as October and ended as late as May. Approximately 5% to 20 % of the US population contracts the flu each year. If a virus is similar to previous strains, people may be partially immune and the severity of seasonal flu symptoms may be reduced. When a “novel” virus appears (one that is new, and to which people have little or no natural immunity), it spreads quickly. 2009 H1N1 was a novel virus and spread rapidly throughout the world, which caused the 2009 flu pandemic and made control of respiratory illness a top priority.
When the general public refers to the “the flu,” they are often under the impression that this is just one type of virus. However, several flu strains are usually active during a season. For instance, the CDC has antigenically characterized 83 influenza viruses, including 62 2009 influenza A (H1N1) viruses, 20 influenza A (H3N2) viruses, and one influenza B virus, collected since October 1, 2013.
How Influenza Replicates: RNA Genetic Mutation
Influenza RNA contains eight segments that change by genetic mutation or reassortment during viral replication. Antigenic drift refers to small point mutations that occur with successive replication, resulting in viral subtypes with some new characteristics. Slight mutations result in strains that people have partial immunity to through previous exposure or vaccinations. If the mutations give rise to viral subtypes that are not similar to previous strains, the virus is likely to spread rapidly. Antigenic shift is a major and abrupt genetic reassortment resulting in new (novel) variants, or subtypes. These new variants are potentially very dangerous because they are often completely unrecognized by host immune systems. For this reason they are able to infect large numbers of animals and/or humans and spread rapidly, leading to epidemics or pandemics.
Types of Influenza
Viral subtypes are identified and named by their surface antigens hemagglutinin (H) and neuraminidase (N). There are three types of influenza. Type A is the most diverse and infects humans and many animals, including ducks, chickens, pigs, whales, horses and seals. While certain subtypes are found in specific animal hosts, birds are hosts to all subtypes of influenza A and are a repeated source of new flu pathogens. Type A is likely to undergo an antigenic shift if two or more subtypes infect a single host; an occurrence that has caused both epidemics and pandemics. Type B influenza infects only humans, primarily children, and generally causes milder symptoms than type A. Type B is known to cause seasonal outbreaks and epidemics, but not pandemics. Type C influenza is common in swine, but rarely seen in humans.
INFLUENZA EPIDEMICS AND PANDEMICS
It is important to know the difference between an influenza epidemic and pandemic. An epidemic is caused when an infectious disease or condition affects many people at the same time within a geographic area. A pandemic is when an infectious disease or condition is affecting people at the same time in many different parts of the world.
Novel Viruses
When Influenza types A and/or B circulate annually, they may cause epidemics. Every 10 to 40 years, however, new or “novel” viruses emerge and circle the globe causing a pandemic. All known influenza pandemics have resulted from influenza A variants undergoing antigenic shift, creating a new virus that spread between humans.
The earliest recognized pandemic of avian flu occurred in 1580 and there have been 31 since then. In 1918-1919, the Spanish influenza A (H1N1) pandemic started in Kansas and spread worldwide through United States military troops and steamship travel. In less than 5 months, 21 million people died. The pandemic claimed 500,000 US lives and killed 50 million worldwide (Two percent of those infected died). In 1957-1958, the Asian Flu A (H2N2) caused 70,000 American deaths, and the 1968-69 Hong Kong Flu A (H3N2) caused 34,000 American deaths. Typically, an avian flu virus first infects pigs then humans. The Hong Kong strain may have jumped directly from birds to humans. In 2001, influenza A (H1N2) emerged and spread globally. It most likely resulted from genetic reassortment of A (H1N1) and A (H3N2) when both viruses were present in one host.
In 2004 a deadly avian flu (Highly Pathogenic Avian Influenza A - H5N2) spread globally in birds and was detected in a flock of Texas chickens. According to the Centers for Disease Control (CDC), this was the first outbreak of HPAI (H5N2) in twenty years. No transmission to humans was reported.
Recent Flu Pandemics
The well-known 1918 “Spanish Flu” pandemic was caused by an H1N1 virus: the ancestor of all later human-adapted seasonal and pandemic species. During the 1918 pandemic, that flu strain was transmitted to pigs and it has been evolving in swine since then. The 2009 H1N1 strain (first called “swine flu”) was created when two common Swine Influenza Type A H1N1 viruses (that infect pigs and sometimes humans who are in contact with pigs) mixed with human flu and bird flu. The pigs were exposed to all four Type A (two swine, one human and one bird) viruses causing a dramatically different new strain of influenza with the ability to spread between humans. Many people had little or no immunity to 2009 H1N1 accounting for high rates of transmission.
As of January 2010, the World Health Organization (WHO) regions reported that more than 209 countries had confirmed cases of 2009 H1N1 influenza virus, including at least 14,142 deaths. This total was believed to be an underestimation of total cases in the world since many countries only use specific tests to confirm diagnosis on many persons with severe illness and/or high risk conditions, and many cases are not reported if the patient does not seek medical care. As of June, 2012, the mortality rate estimated between 151,700 and 575,400 people. A large number of these deaths occurred in Southeast Asia and Africa where access to treatment was limited.
Concern about the high transmissibility of the flu combined with high susceptibility of the world population has resulted in heightened global efforts to inform and vaccinate the public. It is important to remember, however, that flu viruses may mutate and become more virulent, and that every year in late fall and winter, 5% to 20% of the US population is infected with a flu virus. Approximately 226,000 of those infected are hospitalized, and about 36,000 infections result in death. Regardless of the type of virus, influenza is a serious matter.
Pandemic Phases
The WHO identifies six phases of pandemic alert to help health officials plan and activate resources (Table 1). In Phase 1, no viruses circulating in animals are found to cause human infections. In Phase 2, a virus circulating among domesticated or wild animals is known to have caused infection in humans (considered a potential pandemic threat). In Phase 3, an animal or human-animal virus causes sporadic cases or small clusters of disease in people, but not enough to result in community-level outbreaks. In Phase 4, there is verified human-to-human transmission of a virus resulting in community-level outbreaks. This indicates a significant risk of a pandemic threat. In Phase 5, human-to-human spread of a virus into at least two countries, within one WHO region, signals a strong likelihood of an imminent pandemic. In Phase 6, a virus is spreading in at least one country in additional to those in one WHO region meaning a pandemic is underway.
The 2009 H1N1 was a Phase 6 pandemic but the severity of the pandemic was moderate as of September, 2009. This means that most people recovered from the infection without the need for hospitalization or medical care. However, the WHO was concerned about current patterns of serious cases and deaths that were occurring primarily among young persons, including the previously healthy and those with pre-existing medical conditions or pregnancy. Public health leaders recommended a conservative approach to preventative precautions, implementing respiratory precautions in addition to droplet precautions for known or suspected ATD cases.
TRANSMISSION
Influenza is transmitted primarily through one of three ways:
• airborne large-particle respiratory droplets (5 microns or larger) from sneezing or coughing in close proximity (6 feet or closer) to another person,
• smaller aerosols traveling greater distances, or
• contact with respiratory-droplet contaminated surfaces. Inhalation, direct personal contact and touching eyes, nose or mouth with contaminated objects or hands are the most likely routes of flu transmission.
Like other respiratory viruses, influenza viruses attach to ciliated epithelial cells lining the respiratory tract where they penetrate and replicate. Common cold viruses (such as rhinovirus) are heat sensitive and only infect the upper respiratory tract. However, in addition to upper respiratory tissues influenza can also penetrate tissue in warmer, deeper areas such as the trachea, bronchi and lungs leading to more severe symptoms.
The incubation period for influenza is estimated at 1 to 4 days. An infected person can transmit the virus 1 day before symptoms develop, and at least 7 days after onset. Children may be infectious earlier before symptoms start, and remain contagious for longer after onset. Both symptomatic and asymptomatic people spread the infection, so high-risk susceptible people should consider avoiding crowded areas and close contact during times and in locations of influenza occurrence.
About half of the country may be at higher risk of serious illness from novel viruses. The following people have the highest risk of becoming severely ill or dying from both seasonal and novel flu viruses:
• children less than 5 years old
• pregnant women
• children and adolescents aged 6 months to 18 years, who are receiving long-term aspirin therapy and who might be at risk for experiencing Reye syndrome after influenza virus infection
• adults and children who have chronic pulmonary, cardiovascular, hepatic, hematological, neurologic, neuromuscular or metabolic disorders
• adults and children who have immunosuppression
• persons aged 50 years or older
• residents of nursing homes and other chronic-care facilities
CLINICAL SIGNS AND SYMPTOMS OF INFLUENZA AND SEVERE INFLUENZA-RELATED COMPLICATIONS
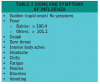
Influenza viral infections can cause a wide range of symptoms, including fever, cough, sore throat, body aches, headache, chills and fatigue (Table 2). Symptoms typically have a sudden onset and patients feel markedly worse than those with the common cold. Some people have reported diarrhea and vomiting associated with influenza. Seasonal flu viruses can vary in severity from mild to severe with the possibilities of pneumonia, respiratory failure and death. Sometimes bacterial infections may occur at the same time as or after infection with influenza viruses and lead to pneumonias, ear infections or sinus infections.
Severe influenza-related complications requiring emergency treatment are listed in Table 3.
PRECAUTIONS AGAINST INFLUENZA
Basic precautions recommended by the CDC for all people include:
• Covering the nose and mouth with a tissue when coughing or sneezing.
• Washing hands often with soap and water. If soap and water are not available, use an alcohol-based hand rub.
• Avoid touching the eyes, nose or mouth. Germs spread this way.
• Try to avoid close contact with sick people. If sick with flu-like illness, CDC recommends staying home for at least 24 hours after your fever is gone except to get medical care or for other necessities. (The fever should be gone without the use of a fever-reducing medicine.) Keep away from others as much as possible to keep from making others sick. This includes hospitals and healthcare facilities treating patients with influenza. Many hospitals have restricted visitation to flu patients and have created rules limiting any minors under the age of 18 from any hospital visitation.
Other important actions that can be taken:
• Follow public health advice regarding school closures, avoiding crowds and other social distancing measures.
• Be prepared in case of illness which may include the need to stay home for approximately 1 week; have a supply of over-the-counter medicines, alcohol-based hand rubs (for when soap and water are not available), tissues and other related items which will eliminate the need to make trips out in public while sick and contagious.
For dental healthcare workers, standard precautions reduce the risk of exposure to most contact and respiratory pathogens that are likely to be encountered. However, additional precautions are recommended for controlling highly contagious diseases, especially those that may become airborne. Prior to the 2009 H1N1 pandemic, healthcare personnel were instructed to observe Droplet Precautions (ie, wearing a surgical or procedure mask with eye protection for close contact), in addition to Standard Precautions, when examining a patient with symptoms of a respiratory infection, particularly if fever is present.
Studies on influenza transmission show that airborne (inhalation) transmission is one of the potential routes of transmission. CDC recommends a more conservative approach in dealing with ATD’s during a pandemic. All healthcare personnel should wear a fit-tested disposable N95 respirator surgical mask or better when they enter the rooms of patients in isolation with confirmed, suspected, or probable ATD such as influenza. Personal protective equipment (PPE) including specialized respiratory protection (fit-tested disposable N95 NIOSH respirators or better), gloves, gowns, and eye protection and other strategies such as innovative triage processes, hand-washing, disinfection, vaccination, antiviral drug use, written program, training, and special building construction and operation to contain and control room air flow. Unless dental facilities are specially equipped to comply with these safety requirements, they should avoid treating patients with ATD symptoms. Healthcare personnel who develop a febrile respiratory illness should be excluded from work for 7 days or until symptoms have resolved, whichever is longer.
SCREENING PATIENTS FOR FLU AND OTHER TRANSMISSIBLE RESPIRATORY INFECTIONS
Infection control starts before the patient arrives at the front office. When a patient is called for appointment confirmation they should be screened for febrile respiratory illness to prevent transmission of an aerosolized transmissible disease.
When the patient arrives, and while protecting their privacy rights, they should be screened again. Vital signs to assess temperature, respirations, and blood pressure can be documented with every visit as part of the patient seating and examination process. Provisions should be made to allow for prompt isolation and assessment of symptomatic patients. [Note: Always protect patient privacy during screening. Written screening forms may be most appropriate.].
A sample script for screening patients is presented in Table 4.
VACCINATIONS
Vaccinations are the highest priority for prevention of illness and should be administered if available and not contraindicated. The severity of seasonal flu epidemics depends on the symptoms, transmissibility of the viruses and susceptibility of the population. Scientists attempt to predict how influenza genes will mutate and/or re-combine as they replicate. Each year vaccines are produced to fight the expected epidemics. Sometimes the vaccines are very effective and other times the viruses mutate and spread differently than scientists predicted, rendering the vaccines less effective. Because flu viruses are usually similar to previous strains, many people have at least partial immunity due to either previous illnesses or vaccines. Due to the increased awareness of the flu and possible pandemics, more healthcare workers (HCW) are receiving flu vaccinations. In the 2007-2008 flu season, vaccinations of HCW reached 47.6%. In the 2011-2012 season, it jumped significantly to reach 62.4% overall in HCW.
Most people are advised to get vaccinated against seasonal influenza, but physicians exclude those people who are allergic to eggs, children under six months old and others who may have complications from the vaccine. Vaccines are available in injection form and a nasal spray. The flu shots contain inactivated fragments of killed influenza and will not cause the flu to manifest. The nasal spray (live attenuated influenza vaccine, or LAIV) is made using a weakened live flu virus. Pregnant women, young children and people with compromised immune systems cannot receive the nasal spray and should receive the injection.
The CDC prioritizes who should be vaccinated if vaccines are available in extremely limited quantities: pregnant women, people who live with or care for children younger than 6 months of age, healthcare and emergency medical services personnel, persons between the ages of 6 months through 24 years and people ages 25 through 64 years who are at higher risk for flu viruses because of chronic health disorders or compromised immune systems. Once demand for vaccinations for the prioritized groups has been met at the local level, programs and providers begin vaccinating everyone from the ages of 25 through 64 years. Current studies indicate that the risk for infection among persons age 65 or older is less than the risk for younger age groups. However, once vaccine demand among younger age groups is met programs and providers will offer vaccination to people 65 or older (see http://www.flu.gov/prevention-vaccination/vaccination/#)
ANTIVIRAL MEDICATIONS
There are prescribed medications from a healthcare provider that can be used to treat influenza. This medicine comes in the form of pills, liquid, or inhaled powder. Those who are very ill with the flu, or those who have a greater chance of additional, serious complications are candidates for this medicine. Most otherwise-healthy people with the flu do not need to be treated with antiviral medication.
Two antiviral medications: oseltamivir (Tamiflu®), and zanamivir (Relenza®) are available for those suffering from the flu. Tamiflu is available in pill or liquid and Relenza is a powder that is inhaled. Because it must be inhaled, Relenza is not recommended for people with breathing problems like asthma or chronic obstructive pulmonary disease (COPD).
When taken properly, these medicines can shorten and lessen the symptom time by 1 to 2 days and can also aid in the prevention of additional complications like pneumonia. For some higher risk patients, the medication can mean the difference between having milder symptoms to a hospital stay. Children and pregnant women can receive these antiviral medicines. Unfortunately, there are a few flu strains that have developed a resistance to oseltamivir.
Physicians should be consulted if the flu is suspected. It is important to distinguish a flu infection from a common cold, because antiviral medication taken within the first 2 days of sickness is recommended. The dosage is usually prescribed for 5 days and must be taken as directed. Some side effects have been noted, which are much like having the flu itself; nausea, vomiting, dizziness, runny nose, etc.
Antiviral medications are a second line of defense as a treatment. Even with the availability of these medications, the best defense is to receive the influenza vaccination.
SUMMARY
Influenza is an acute respiratory illness that returns every year in a new form. The 2009-2010 flu season brought a new threat to the world because 2009 H1N1 was a novel virus, to which virtually everyone was susceptible. The 1918 “Spanish Flu” H1N1 virus caused a devastating pandemic when no antiviral medications and no vaccinations were available. The 2009 H1N1 was derived from the 1918 virus and is highly transmissible with a severity similar to seasonal flu. Clinical signs and symptoms of influenza are fever, headache, muscle aches, exhaustion, cough, respiratory symptoms and possibly vomiting and/or diarrhea.
The most important strategy to prevent illness is vaccination. World health organizations urge everyone who is eligible to receive a vaccination. Dental offices should employ Respiratory Hygiene/Cough Etiquette and screen patients for respiratory symptoms and aerosol transmissible diseases. Symptomatic patients should not be treated, and dental healthcare workers with symptoms should not report to work. People in high risk categories may experience severe cases of influenza and should be vaccinated early, protected from exposure and seek immediate medical attention if they become ill. Informed, trained and motivated dental healthcare workers are an important part of the healthcare community’s effort to overcome any type of seasonal influenza.
The following link offers short Public Service Announcements (PSAs) from the CDC that could be played for your patients. http://www.cdc.gov/flu/freeresources/media-psa.htm
ABOUT THE AUTHOR
Wilhemina Leeuw, MS, CDA
Wilhemina Leeuw, MS, CDA is a Clinical Assistant Professor of Dental Education at Indiana University Purdue University, Fort Wayne. A DANB Certified Dental Assistant since 1985, she worked in private practice over twelve years before beginning her teaching career in the Dental Assisting Program at IPFW. She is very active in her local and Indiana state dental assisting organizations. Prof. Leeuw’s educational background includes dental assisting - both clinical and office management, and she received her Master’s degree in Organizational Leadership and Supervision. She is also the Continuing Education Coordinator for the American Dental Assistants Association.
SUGGESTED SITES FOR OFFICE REFERENCE MATERIALS
Centers for Disease Control – Seasonal Flu, http://www.cdc.gov/flu/references.htm
Respiratory Hygiene/Cough Etiquette in Healthcare Settings https://www.cdc.gov/flu/professionals/infectioncontrol/resphygiene.htm
World Health Organization – How to HandWash, http://www.who.int/gpsc/5may/How_To_HandWash_Poster.pdf
REFERENCES
(CDC 9/9/09) October 2006 “Interim Guidance on Planning for the Use of Surgical Masks and Respirators in Healthcare Settings during an Influenza Pandemic.” http://www.cdc.gov/flu/professionals/infectioncontrol/resphygiene.htm
California OSHA, Title 8, Chapter 4, Section 5199 Excerpts
Can’t Stop Coughing? 8 Causes of Chronic Cough. http://www.health.com/health/condition-article/print/0,,20267700,00.html (Accessed 7/7/09)
CDC H1N1 Interim Guidance for Infection Control for Care of Patients with Confirmed or Suspected Novel Influenza A (H1N1) Virus Infection in a Healthcare Setting. http://www.cdec.gov/h1n1flu/guidelines_infection_control.htm
CDC Interim Guidance for the Use of Masks to Control Influenza Transmission. http://www.cdc.gov/flu/professionals/infectioncontrol/maskguidance.htm
CDC Novel H1N1 Vaccination Planning Q & A, August 10, 2009 http://www.cdc.gov/flu
Control of Communicable Diseases Manual. D Heymann, Editor, Eighteenth Ed. 2004. Influenza, Pg 281 - 287
Cottone’s Practical Infection Control in Dentistry, Third Edition, Edited by John A. Molinari, PhD and Jennifer A. Harte, DDS, Chapter 4: Upper Respiratory Tract Infections, pg 45-62
Draft Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee (HICPAC), CDC. http://www.cdc.gov/ncidod/dhqp/ppe.html.
Droplet Precautions, Guideline for Isolation Precautions in Hospitals, Department of Health and Human Services, Centers for Disease Control and Prevention, http://www.cdc.gov/ncidod/dhqp/gl_isolation_droplet.html
Dynasty: Influenza Virus in 1918 and Today, June 29, 2009 News Release. NIH News. U.S. Dept of Health and Human Services. http://www.nih.gov/news/health/jun2009/niaid-29.htm
Early Identification and Deferral of Patients with Flu-Like Symptoms – Suggested Script for Front Office Staff. http://www.osap.org/flu
Early Results: In Children, 2009 H1N1 Influenza Vaccine Works Like Seasonal Flu Vaccine. http://www.nih.gov/news/health/sep2009/niaid-21.htm
Guidelines for Infection Control in Dental Health Care Settings--2003, Centers for Disease Control MMWR Dec. 19, 2003 / 52(RR17); 1-61
http://www.cdc.gov/flu/antivirals/whatyoushould.htm (Accessed 11/5/13)
http://www.cdc.gov/flu/weekly/summary.htm (Accessed 11/5/13)
http://www.cdc.gov/flu/spotlights/pandemic-global-estimates.htm (Accessed 4/17/13)
http://www.cdc.gov/h1n1flu/guidelines_infection_control.htm
http://www.cdc.gov/h1n1flu/updates/international/, (Accessed 8/17/09)
http://www.monofacto.com/facts/dictionary?PCR+test (Accessed 10/12/09)
http://www.who.int/csr/don/2010_01_22/en/ (Accessed 4/17/13)
Infection Control and Management of Hazardous Materials for the Dental Team, Third Ed. Miller, Palenik. Chapter 9, Immunization, Influenza, Pg 151- 153
Influenza Vaccine Information for Health Care Personnel. Department of Health and Human Services, Centers for Disease Control and Prevention. http://www.cdc.gov/ncicoc/hip/flu_vac.htm
Interim Guidance on Antiviral Recommendations for Patients with Novel Influenza A (H1N1) Virus Infection and Their Close Contacts. http://www.cdc.gov/h1n1flu/recommendations.htm (Accessed 5/6/09)
Novel Influenza A (H1N1) Virus, Resources for Dental Professionals (5.12.09), http://www.osap.org/displaycommon.cfm?an=1&subarticleenbr=1216
Protocol for Managing Dental Patients with Confirmed or Suspected Respiratory Infection. http://www.osap.org/associations/4930/files/Officeprotocol.osap.pdf
Respiratory Protection for Healthcare Workers in the Workplace Against Novel H1N1 Influenza A: A Letter Report. Report Brief, September, 2009. Institute of Medicine of the National Academies
Seasonal Flu. http://www.flu.gov/about_the_flu/seasonal/# (Accessed 4/22/13)
Study: Face masks seem to protect against flu. CNNhealth.com http://www.cnn.com/2009/HEALTH/08/03/face.mask.flu/index.html
Swine Flu. For Concerned Parents and Caregivers. http://www.cdec.gov/swineflu/parents.htm (Accessed 4/29/09)
The Flu…And You: A Novel Challenge with 2009 H1N1 Influenza A. Andrews, N., American Dental Assistants Association, 2009.
Transmission of Influenza A Viruses Between Animals and People. Department of Health and Human Services, Centers for Disease Control and Prevention. http://www.cdc.gov/flu/avian/gen-info/transmission.htm
U.S. Department of Health and Human Services, NIH News, Monday, September 21, 2009
What You Should Know About Flu Antiviral Drugs. CDC. http://www.cdc.gov/flu/antivirals/whatyoushould.htm (Accessed 4/22/13)
WHO Guidelines for Pharmacological Management of Pandemic (H1N1) 2009 Influenza and other Influenza Viruses, Executive Summary. 20 August 2009. World Health Organization
World Health Organization, Current WHO phase of pandemic alert. Current phase of alert in the WHO global influenza preparedness plan.
www.PandemicFlu.gov, (Accessed 9/9/09)