You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The high rate of infant mortality in the United States is a public health crisis.1 Infant mortality, defined as the number of infant deaths before age 1 per 1,000 live births, is an indicator of national health due to its association with maternal health, quality and access to medical care, socioeconomic status, and public health practices.1,2 The United States ranks 26th in infant mortality among other developed countries.1,2 The chief causes of infant mortality in this country are low birth weight (weight below 2,500 g or 5 lbs. 8 oz.) and pre-term births (birth before 37 weeks gestational age), which account for over 39% of infant mortality.1,2 In recent years, research placed emphasis on the link between poor oral health of pregnant women and premature or low birth-weight babies.3-5 Studies concerning adverse pregnancy outcomes associated with periodontal disease found that dental treatment during pregnancy is safe.4,6-11
There have been many efforts during the past decade to move pregnant patients and healthcare providers toward a better understanding of the importance and safety of oral healthcare prior to, during, and after pregnancy.12-15 Dental hygienists are well-positioned to provide oral care and offer pregnancy oral health information, as well as facilitate referrals to other healthcare providers. Many states, including Michigan, are currently developing perinatal oral healthcare guidelines with specific goals in mind. Goals include reducing the infant mortality rate, ensuring a healthy start for babies at the outset of their life, and providing access to care, through improving the oral health of the mother.13,15 In addition, a panel of multidisciplinary experts with the New York State Department of Health developed the 2006 Oral Health Care During Pregnancy and Early Childhood: Evidence-Based Guidelines for Health Professionals to improve oral healthcare during pregnancy.12 The oral health guidelines were intended to educate healthcare providers and patients on the effectiveness and safety of dental care during pregnancy. The guidelines suggest dental examinations and periodontal care are encouraged at any time during pregnancy.12
Background
In 2009, Cruz et al reported periodontal disease was recognized as the second most prevalent oral disease worldwide.8 A significant association found in the study linked maternal periodontal disease and low birth-weight babies.8 In 2008, a meta-analysis was published on the topic of maternal periodontal disease, poor pregnancy, and neonatal outcomes. This report reviewed several clinical trials and compared birth outcomes of pregnant women who received periodontal disease treatment during pregnancy with a control group of pregnant women whose periodontal disease was treated post-partum. The report concluded treating periodontitis with standard therapies (scaling and root planing) during pregnancy was safe.9 Even though dental care during pregnancy has been shown to be safe and can prevent long-term health problems for both mother and child, an overwhelming number of women do not seek dental care during pregnancy.9,16,17 Several studies have demonstrated a need for pregnant women to receive preventive dental care and oral health education during pregnancy to enhance early health of their child.4,7,9,18 In addition, studies have demonstrated a major hurdle for pregnant patients to receive oral care lies in the healthcare provider’s basic understanding of how essential oral health contributes to the overall health of the mother and the developing fetus.7,9
During pregnancy, healthcare providers of various disciplines work concurrently to support the healthcare needs and well-being of the woman and her developing fetus. Among those healthcare providers are: general medical doctors/physicians, obstetricians, midwives, advanced practical nurses, nurse practitioners, dentists, and dental hygienists. Over the last decade many healthcare professionals shared their knowledge and attitudes regarding the importance of oral health during pregnancy. A 2012 study explored the current knowledge, attitudes, and behaviors of dental and prenatal care practitioners about oral healthcare during pregnancy.19 Noteworthy, only 50% of general practitioners (medical doctors and physicians) advised their pregnant patients to seek a periodontal checkup as part of their prenatal care, even though 81% were aware of the increased risk associated with gingival inflammation during pregnancy.19 Fifty-four percent of the general practitioners indicated they were aware that poor oral health could affect pregnancy outcomes.19 Many (68%) believed that dental procedures such as scaling and root planing were unsafe treatments during pregnancy and advised patients to delay dental treatment until after the birth.19,20 Bell found healthcare providers received little oral health education and therefore reported low confidence levels in knowledge of oral health during pregnancy.6 These attitudes, knowledge, and practices are in contrast to current recommendations and highlight a lack of awareness on this topic.12,14
Obstetricians’ knowledge of oral health and birth outcomes were reported in a random sample survey of US obstetricians. Sixty-four percent reported the need for dental care during pregnancy, yet 49% included an oral health evaluation in their plan of care.11 The majority of the obstetricians surveyed agreed that it was safe for pregnant patients to complete preventive care treatments such as prophylaxis, restorative treatments for active carious lesions, and treatment for abscess drainage. Conversely, obstetricians debated the safety regarding radiographs, periodontal surgery, amalgam placement, and narcotic use.11
Occasionally, pregnant women received care though an office midwife or nurse practitioner versus the physician. Both professions are positioned to educate women on the need for oral care during pregnancy. A 2012 report stated midwives had limited knowledge of oral healthcare during pregnancy, were not informed of the impact of poor oral health on birth outcomes, and only discussed oral health when initiated by the pregnant patient.19 Similarly, advanced practical nurses and nurse practitioners responded with little knowledge of oral health effects on pregnancy and birth outcomes when surveyed.17 Research indicated that the traditional education of advanced practical nurses and nurse practitioners did not include providing an oral health examination during routine visits, and they needed more information about periodontal disease and its impact on adverse pregnancy outcomes.17 Twenty percent of the surveyed nurse practitioners indicated that oral examinations are the responsibility of the dental professional.17
In 2009, a study reported most dentists have favorable attitudes toward pregnancy-specific counseling and agreed preventive dental treatment should be a part of prenatal care.3,11 Of those surveyed, 91% agreed dental treatment was an important aspect of prenatal care. However, the study also reported dentists were still reluctant or uncomfortable treating pregnant patients even though it has been shown safe. Several studies have reported that dentists are uncertain about the safety of dental procedures and stress their hesitancy to treat women during pregnancy.3,11,19 Dentists and dental hygienists were asked the same questions regarding knowledge, attitudes, and practice of oral health and birth outcomes in a 2012 study. Misinformation was found among dental personnel regarding the safety and efficacy of dental care during pregnancy.21
George et al reported dentists have a high level of knowledge regarding adverse effects of poor oral health on pregnancy; however, many reported treatment practices taught in dental school included delay of treatment until after delivery.19,22 Several studies reported lack of time for proper counseling, legal risks associated with negative birth outcomes, and limited knowledge of dentists about the safety of procedures as reasons for lack of dental treatment by dental professionals during pregnancy.3,11,19,22
The dental hygienist is an oral healthcare professional well versed in preventive measures and who advocates for healthy lifestyles in addition to providing safe and effective dental hygiene services. A research study completed in 2012 surveyed dental hygienists’ knowledge and attitudes regarding oral-systemic connections; less than half of the dental hygienists’ surveyed reported having a strong opinion regarding evidence that links periodontal disease to pregnancy outcomes.6
The dental hygienist is in a prime position to educate and advocate; therefore, it is important to investigate the knowledge of dental hygienists when treating pregnant women. The purpose of this research was to survey dental hygienists’ knowledge, attitude, and practice behaviors providing oral healthcare to pregnant women.
Methods and Materials
A convenient sample of Michigan dental hygienists was surveyed to explore their knowledge, attitudes, and practice behaviors while providing care for pregnant patients. Data were collected through electronic surveys to answer the following questions:
1. What is the knowledge level reported by dental hygienists who provided care to pregnant patients?
2. What are the attitudes of dental hygienists who provided care for pregnant patients?
3. What are the practice behaviors of dental hygienists who provided care to pregnant patients?
The study utilized an anonymous electronic survey administered via SurveyMonkey® to all Michigan Dental Hygiene Association (MDHA) members (n = 1,047). The MDHA email list provided electronic addresses to disseminate the invitation, survey, and informed consent. This study received approval from the Institutional Review Board of the University of Texas Health Science Center San Antonio. Survey participants were given 2 weeks to complete the survey, with two follow-up emails to encourage participation.
Original survey questions were distributed to Michigan dentists for a study to evaluate dentists’ knowledge of oral healthcare during pregnancy; the results were analyzed by the Michigan Department of Community Health. Subsequently, questions were modified for dental hygienists to gather similar data regarding knowledge, attitudes, and practice behaviors when providing oral care to pregnant patients. The survey included participant demographics and Likert-scale questions, which captured the dental hygienists’ knowledge, attitudes, and practice behaviors. Likert rating scales were anchored as follows: 1 = strongly disagree, 2 = disagree, 3 = agree, 4 = strongly agree. Generally, items were worded such that higher ratings reflected more positive evaluations and lower ratings reflected more negative evaluations of instructional qualities and outcomes.
Data were collected online via SurveyMonkey and imported into SAS® 9.4 for Windows. Statistical analysis included: descriptive statistics, Spearman’s Rho correlations, analysis of variance, and chi square contingency tables. When Spearman correlations were given, the ordered survey responses were coded numerically and the numbers were correlated. For some tables, “strongly agree” and “agree” were collapsed to “agree,” and “strongly disagree” and “disagree” were condensed to “disagree.” Significance was taken at P < .05 for all analyses.
Results
Demographics
A 14.4% response rate (n = 150) was attained. The majority of the respondents were white (98.7%) and female (98.0%). The most frequent age group was 55 to 64 (31%). Education levels reported were: entry-level associate degree (41.6%), baccalaureate degree (39.6%), and graduate level degree (18.8%). The number of years practicing ranged from 0 to 48 and averaged 21.0 years.
Knowledge
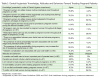
Knowledge regarding oral care during pregnancy is represented in Table 1. Respondents’ knowledge indicated that the following treatments could be provided throughout pregnancy: prophylaxis (95.8%), emergency care (92.7%), periodontal treatment (76.3%), and restorative care (61.5%). One question, “dental hygiene services should only be provided during the second trimester,” was written in the negative; a disagree rate of 85.6% indicated a high level of knowledge about this topic. Respondents agreed there was an association between poor dental care and adverse pregnancy outcomes ( 95.9%) and obstetric complications associated with poor oral health ( 91.6%).
Higher Degree
Knowledge about providing dental hygiene services outside of the second trimester was positively associated with dental hygienists who had a higher degree completed (r = 0.25, P = .0354), as was the knowledge about restorative care being provided throughout pregnancy (r = 0.27, P = .0117). Also associated with higher degree completed was the knowledge that periodontal treatment (scaling and root planing) could be safely provided throughout pregnancy (r = 0.22, P = .0371).
Years Since Degree
There was a statistical difference between knowledge dental hygienists demonstrated regarding restorative care being provided during pregnancy related to years since degree completion. In the group of respondents who were less than 5 years post degree completion, 18% believed that restorative care could be completed throughout pregnancy. Similarly, 48% of respondents in the group who were more than 21 years since their degree completion believed the same (P = .0480). Those who knew restorative dental care could be provided throughout pregnancy averaged 24.4 years in practice while others averaged 18.9 years (P = .0175). Respondents were evenly split on whether pregnant women could safely receive dental radiographs, although the knowledge about the safety of dental radiographs was also positively associated with years since degree (r = 0.26, P = .0215).
Attitudes
New education and inter-professional collaboration regarding oral health and pregnancy was favored by 64% and 74% of respondents, respectively (Table 2). Regardless of years in practice (P = .7124), level of degree (P = .6365), or years since degree (P = .6933), the majority of respondents (64%) desired more education about caring for a pregnant patient. Table 2 displays attitudes toward obtaining and receiving the most current education. Delivery responses varied from continuing education to 1-day workshops.
Table 1 displays dental hygienists’ attitudes and practice behaviors about treating pregnant patients. All respondents agreed oral healthcare was an important part of prenatal care, and prenatal care should include a dental screening. The majority of respondents were trained, comfortable, and had no aversion to treating pregnant women. Most items in Table 1 show significant (P < .01) evidence that the respondents’ responses were consistent with the 2006 New York State Perinatal Guidelines and the 2012 Oral Health Care National Consensus Statement.12,14
However, respondents differed from the above guidelines, regarding the safety of radiographs— only 50.5% of the respondents agreed radiographs throughout pregnancy were safe.
Behaviors
Ninety percent of respondents reported willingness to provide care for pregnant women, and 85% indicated they or their employers agreed to accept referrals to treat pregnant women. Table 3 shows the differences between the percentages of respondents providing care and accepting referrals for pregnant women. Although dental hygienists and employers were willing to treat pregnant patients (90.4%), those who accepted Medicaid patients were much lower (30%). When asked about established referral arrangements with prenatal care providers, the majority of dental hygienists (69.7%) reported no arrangement was in place, 11.4% responded yes, and 18.4% were unaware of an arrangement.
Respondents who had more years in practice reported having established referral arrangements for pregnant patients between prenatal care providers and oral care providers (P = .0027). There was a significant difference (P = .0027) in years of practice between respondents reporting established referral arrangements (28.2 years), those reporting no arrangements (21.9 years), and those unsure (13.3 years). It was also reported that as a dental hygienist’s degree level increases, so does the referral acceptance rate (P = .0111).
Discussion
Michigan dental hygienists demonstrated positive knowledge, attitudes, and behaviors regarding oral care provided throughout pregnancy. All respondents regarded oral healthcare an important part of prenatal care and believed oral examinations should be included with prenatal preventive care. In general, higher degree level and greater years of experience resulted in higher agreement with guidelines developed in the 2006 New York Perinatal Oral Care Guidelines and the 2012 Oral Health Care National Consensus Statement.12,14
The majority of respondents agreed upon the association between poor oral healthcare and adverse pregnancy outcomes. They were also knowledgeable about the links between active periodontitis, low birth weight, and premature birth. These findings, although more positive than previous studies, are consistent with the earlier reports found in the literature.11 When compared to low birth weight and premature birth, the current study revealed some skepticism regarding the correlation of the presence of active periodontitis during pregnancy and its association for an increased risk of developing preeclampsia. Again, the findings of the current study are more positive than earlier reports yet consistent with trends found in the literature.11 Respondents were less knowledgeable about obstetric complications and the association to poor oral health, which is consistent with the literature.11 An unexpected finding revealed that a small percentage of respondents reported feeling uncomfortable and/or preferred not to treat pregnant women. Some felt as though they were not trained to treat women during pregnancy, while others had liability concerns. Although these findings were unexpected to come from the respondent group, dentists surveyed in an earlier study declared having the same fears as the respondents from this survey.11
Inconsistencies existed within the profession regarding when and what procedures can be safely performed during pregnancy. The majority of the respondents identified emergency care and prophylaxis could be safely provided throughout pregnancy. By contrast, some were less knowledgeable about when and if periodontal therapy (scaling and root planing), restorative care, and radiographs could be completed. Knowledge regarding what procedures could be safely provided throughout pregnancy, such as restorative care and periodontal therapy, was positively associated with a more advanced degree. Similarly, knowledge about administering radiographs throughout pregnancy was positively associated with the number of years since degree.
The results concluded continuing education regarding oral healthcare and pregnancy was preferred. These results were consistent with findings throughout the literature that dental hygienists required continuing education to increase their knowledge about new oral-systemic connections.6,23 Implementing additional peri and prenatal education could be accomplished through continuing education courses and inter-professional collaboration. Comprehensive care for pregnant patients can improve when dental hygienists participate in inter-professional collaboration. Dental hygienists indicated an interest in participating in professional collaboration activities, however they lacked time and knowledge to develop professional referral relationships with prenatal care providers.
This study adds to the body of literature regarding dental hygienists’ knowledge, attitudes, and behaviors about oral health and pregnancy; however, limitations were noted. Limitations included a 14.4% response rate, no item identified if dental hygienists were actively practicing, and respondents were allowed to skip items. This lack of full participation with each question could have resulted in fewer answers about key knowledge, attitudes, and practice behaviors. The survey questions for this study were modified from a research study that evaluated dentists’ knowledge of oral healthcare during pregnancy and were not tested for validity, which could be a limitation.
Future research goals should focus on how dental hygienists can increase their knowledge about perinatal oral care through continuing education and inter-professional collaboration. Research should place emphasis on developing a universal standard of care surrounding perinatal oral health guidelines for all healthcare providers. Michigan can benefit from these survey results as it forges a strategic plan to develop and implement Michigan-specific guidelines. As guidelines are implemented and assessed, pregnant patients will be provided the opportunity to seek counsel, diagnosis, and treatment of oral health problems, creating an overall higher standard of care.15
Conclusion
Surveyed Michigan dental hygienists demonstrated positive knowledge, attitudes, and behaviors about providing oral healthcare during pregnancy. Additionally, results indicated regardless of years of experience or level of degree, most desired more education about caring for pregnant patients. Dental hygienists are in a position to use current findings, protocols, and practice guidelines to provide preventive oral care and advocate for pregnant patients. Improving oral health practices and preventive behaviors of pregnant women through education and referrals could reduce the risk of premature births and low birth-weight babies. It is imperative that prenatal healthcare providers collaborate with oral healthcare providers to help improve the chances for a full-term infant.
About the Authors
Stacey A. Schramm, RDH, BS, MSDH, is a Professor of Dental Hygiene at Kellogg Community College. Mary E Jacks, RDH, MS, is an Educational Specialist in the Virtual & Innovative Teaching and Learning Center at the University of Texas Health Science Center at San Antonio. Thomas J. Prihoda, PhD, is a Professor/Research at the Department of Pathology at The University of Texas Health Science Center at San Antonio. Martha J. McComas, RDH, MS, is a Clinical Assistant Professor at the Dental Hygiene Program, Department of Periodontics and Oral Medicine, University of Michigan School of Dentistry. Emelda E. Hernandez, RDH, MS, is an Assistant Professor/Clinical Dental Hygiene Division, Department of Periodontics at The University of Texas Health Science Center at San Antonio.
References
1. MacDorman MF, Mathews TJ, Mohangoo AD, Zeitlin J. International comparisons of infant mortality and related factors: United States and Europe, 2010. Natl Vital Stat Rep. 2014;63(5):1-6.
2. Martin JA, Hamilton BE, Ventura SJ, et al. Births: final data for 2010. Natl Vital Stat Rep. 2012;61(1):1-72.
3. Huebner CE, Milgrom P, Conrad D, Lee RS. Providing dental care to pregnant patients: a survey of Oregon general dentists. J Am Dent Assoc. 2009;140(2):211-222.
4. Kumar J, Samuelson R. Oral health care during pregnancy recommendations for oral health professionals. N Y State Dental J. 2009;75(6):29-33.
5. Wilder R, Robinson C, Jared HL, et al. Obstetricians’ knowledge and practice behaviors concerning periodontal health and preterm delivery and low birth weight. J Dent Hyg. 2007;81(4):81.
6. Bell KP, Phillips C, Paquette DW, et al. Dental hygienists’ knowledge and opinions of oral-systemic connections: implications for education. J Dent Educ. 2012;76(6):682-694.
7. Cibulka NJ, Forney S, Goodwin K, et al. Improving oral health in low-income pregnant women with a nurse practitioner-directed oral care program. J Am Acad Nurse Pract. 2011;23(5):249-257.
8. Cruz SS, Costa Mda C, Gomes-Filho IS, et al. Contribution of periodontal disease in pregnant women as a risk factor for low birth weight. Community Dent Oral Epidemiol. 2009;37(6):527-533.
9. Dasanayake AP, Gennaro S, Hendricks-Munoz KD, Chhun N. Maternal periodontal disease, pregnancy, and neonatal outcomes. Am J Matern Child Nurs. 2008;33(1):45-49.
10. Michalowicz BS, Hodges JS, DiAngelis AJ, et al. Treatment of periodontal disease and the risk of preterm birth. N Engl J Med. 2006;355(18):1885-1894.
11. Strafford KE, Shellhaas C, Hade EM. Provider and patient perceptions about dental care during pregnancy. J Matern Fetal Neonatal Med. 2008;21(1):63-71.
12. Oral health care during pregnancy and early childhood: Practice guidelines. Albany, NY: New York State Department of Health; 2006.
13. National Maternal and Child Oral Health Resource Center. Access to oral health care during the perinatal period: A Policy Brief. Washington, DC: National Maternal and Child Oral Health Resource Center [Internet]; 2008. http://mchoralhealth.org/PDFs/PerinatalBrief.pdf. Accessed April 28, 2016.
14. National Maternal and Child Oral Health Resource Center. Oral health care during pregnancy: A national consensus statement. Washington, DC: National Maternal and Child Oral Health Resource Center [Internet]; 2012. http://mchoralhealth.org/PDFs/OralHealthPregnancyConsensus.pdf. Accessed April 28, 2016.
15. A summary of the 2013 Michigan perinatal oral health conference. Lansing, MI: Michigan Department of Community Health; 2013.
16. Michalowicz BS, DiAngelis AJ, Novak MJ, et al. Examining the safety of dental treatment in pregnant women. J Am Dent Assoc. 2008;139(6):685-695.
17. Wooten KT, Lee J, Jared H, et al. Nurse practitioners’ and certified nurse midwives’ knowledge, opinions, and practice behaviors regarding periodontal disease and adverse pregnancy outcomes. J Dent Hyg. 2011;85(2):122-131.
18. Al Habashneh R, Guthmiller JM, Levy S, et al. Factors related to utilization of dental services during pregnancy. J Clin Periodontol. 2005;32(7):815-821.
19. George A, Shamim S, Johnson M, et al. How do dental and prenatal care practitioners perceive dental care during pregnancy? Current evidence and implications. Birth. 2012;39(3):238-247.
20. Al-Habashneh R, Aljundi S, Alwaeli H. Survey of medical doctors’ attitudes and knowledge of the association between oral health and pregnancy outcomes. Int J Dent Hyg. 2008;6(3):214-220.
21. Kloetzel MK, Huebner CE, Milgrom P, et al. Oral Health in pregnancy: educational needs of dental professionals and office staff. J Public Health Dent. 2012;72(4):279-286.
22. Da Costa EP, Lee JY, Rozier RG, Zeldin L. Dental care for pregnant women: an assessment of North Carolina general dentists. J Am Dent Assoc. 2010;141(8):986-994.
23. Boyd LD, Hartman-Cunningham ML. Survey of diabetes knowledge and practices of dental hygienists. J Dent Hyg. 2008;82(5):43.