You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The use of simulation in medical and health science education has emerged as a seminal pedagogical tool in the past several decades.1-3 The needs and application of simulation technology for training in dental and dental hygiene education have progressively paralleled the same utility of supporting and improving student learning.4-6 Incorporating simulation into preclinical curriculum acknowledges the Institute of Medicine’s attempt at improving patient safety and enhances student ability and confidence prior to encountering live patients.7,8 Simulation can be incorporated into various preclinical phases of dental and dental hygiene education but must be financially feasible and supported by the faculty of each institution.
Prior to providing oral healthcare to patients, undergraduate dental hygiene students must demonstrate proficiency in all areas of patient oral health assessment, treatment, and evaluation. Included in the oral health assessment are identification and recording of specific dental restorative conditions. Historically, students struggle with demonstrating these skills despite didactic and laboratory instruction in dental materials and theory.9 Preclinical laboratory sessions typically include students partnering with one another to practice identification and assessment skills; however, traditional undergraduate dental hygiene students are often young adults and may have limited dental restorations, reducing practical experience beyond 2-dimensional (2D) textbook and didactic instruction. Advances in dental material shade-matching and contouring abilities have introduced clinical similarities between various materials and tooth structures with seemingly undetectable margins.10,11 Although these attributes contribute to the success of esthetic dentistry, identification and charting of these materials have proved to be challenging for preclinical dental hygiene students.12,13 Although these concepts are reviewed didactically using photographs and written descriptions, students continue to have difficulty comprehending 2D models and have limited preclinical laboratory experiences. The ultimate goal of dental and dental hygiene education is to become proficient in skills set forth by the Commission on Dental Education. Deliberate practice is an educational approach to become proficient in these skills by using repetition, assessment of performance, and feedback resulting in improved skill performance by the student.
Other health science disciplines continue to demonstrate success in the use and effectiveness of simulation as an adjunct to clinical and didactic learning. Simulation closes the gap between preclinical knowledge building and actual hands-on patient care. In the 1960s, the cardiology patient simulator was developed. Still in use today, this simulator is able to reproduce 30 different cardiac conditions, allowing medical students to successfully improve training in cardiac and pulmonary clinical skills.14,15 Many programs in emergency medicine use simulation scenarios for rapid response teams to practice critical skills such as intubation and resuscitation. These activities improve team member roles during real-life traumas and hospital emergencies.16-18 Neurosurgery, vascular, and orthopedic surgery students also benefit from simulation technology to build and improve surgical skills.19,20
In the nursing education and practice setting, simulation programs have been developed to improve learning environments for nurses of varying levels of experience and expected scenarios, such as critical care, acute care, infant care, obstetrics, and gynecology.21-23 Hospitals are now incorporating simulation into their orientations. One hospital developed a simulation program concurrently with its cardiac surgery unit and developed scenarios that reflected typical care a cardiac patient may require.24,25 In obstetrics, simulation training is common. New and seasoned practicing nurses as well as other health professionals have opportunities to participate in common neonatal diagnoses such as sepsis and respiratory distress. The team approach to learning with simulation addresses the need to improve neonatal outcomes.26
Simulation in anesthesia education has been used since the 1980s. Given the nature of the practice environment, teachable moments are often overshadowed by the necessity for seasoned anesthesiologists to respond to critical patient needs instead of allowing for student instruction. Simulation in anesthesiology offers learners the opportunity to experience critical decision-making in a safe environment.27 In addition, the American Board of Anesthesiology now requires some form of simulation training to fulfill certification requirements.28
The two theoretical frameworks used in this study include Benner’s stages of clinical competence29 and Kirkpatrick’s training outcomes model.30,31 Students interacting with the simulated dental conditions in this investigation were provided with both a visual and tactile sense of experiential learning.32 “Learning by doing, observing, and participating” provides experiential learning in the form of apprenticeship rather than isolated didactic classroom instruction.32 Benner’s theory reflects upon these vital experiences related to both philosophical behaviorism and constructivism, and is based on the Dreyfus model of skill acquisition.32-35 This theory also recommends cohesive adoption of experiential learning into a larger didactic training process, including a well-designed curriculum and evaluation protocol.33 Benner’s theoretical framework is ubiquitous among educational research in nursing and has direction for interprofessional applications.36-38
The aim of this study was to investigate the use of customized simulated mouth models in improving identification and recording of dental restorations in first-year dental hygiene students when compared to the use of traditional didactic instruction and 2D images.
Methods and Materials
The School of Dental Hygiene at Old Dominion University enrolls 48 students into its entry-level baccalaureate degree program each year. The program requires 2 years of prerequisite and general education courses preceding 2 years of dental sciences, dental hygiene theory and practice, community oral health, research methodology, and teaching strategies. Participants of this study were dental hygiene students who had completed 2 years of prerequisite courses and were recognized as first-year dental hygiene students. Students completed one semester of a dental materials course and had knowledge of Black’s classification. The School of Dental Hygiene supported this research study by providing participants and the facility for conducting the clinical trial. Prior to the start of this investigation, the protocol was reviewed and approved by the institutional review board ensuring the protection of human subjects.
Using an A-dec 42L Stationary Simulator (A-dec Inc), 11 stock interchangeable Frasaco A-PZ DA (Frasaco USA) periodontal simulated mouth models were customized to reflect restorative findings of a typical patient receiving care in the dental hygiene clinic. Each model was uniquely modified by a faculty dentist who “restored” them to randomly include 10 chartable items: two sealants, three posterior multisurface amalgams, three posterior multisurface composites, and two anterior multisurface composites. Two-dimensional images were obtained by photographing dentition of three patients from the clinic facility with 10 chartable items similar to the modified simulated mouth models.
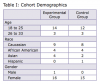
A convenience sample of dental hygiene students from the first-year baccalaureate degree program was chosen for this study. At the time of the study, 48 students were enrolled in the program as first-year dental hygiene students and were eligible for participation in the investigation (Table 1). Following recruitment, 34 students committed to enrollment in the study. The number of sample participants was based on the total available students starting their first-year dental hygiene cohort experience, having all been equally exposed to one semester of dental and dental hygiene science studies. It was important to study this sample population because all participants were identified as having the same formal prerequisite education and only one cohort semester of education in the dental hygiene program. The sample was randomly divided into two groups: the Didactic Group (control) and the Simulator Group (experimental). Four students reported having 2 years or less of dental assisting experience prior to entering the program. Two of these students were randomly assigned to each group.
Random assignment rendered 17 students in the Simulator Group (experimental) and 15 students in the Didactic Group (control). Two students from the control group did not complete all sessions and were disqualified from the study. Students in the Simulator Group used a randomly selected custom-simulated mouth model for three sessions of 15 minutes each to practice identification and documentation of dental conditions. Both groups had previous identical didactic and laboratory lessons on dental charting. Students in the Didactic Group viewed randomly selected 2D images for three sessions of 15 minutes each to also practice identification and documentation of dental conditions. Students from both groups recorded findings using standard dental charting criteria. Students in SC scheduled individual 15-minute timed sessions with a supervising faculty in a private room with one simulator. Students in the Didactic Group SC scheduled individual 15-minute timed sessions with a supervising faculty in a quiet room. Sessions were scheduled over a 3-week timeframe. Students charted findings at every session. Students were not able to ask questions or collaborate with other students. Both groups received feedback immediately after the 15-minute time ended. One dental hygiene faculty member graded all dental charts anonymously and did not see the student’s name or any identifying information to maintain intrarater reliability. Because there were 10 chartable items in each scenario, each item was worth 10 points for a total of 100 possible points earned per session.
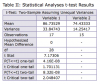
A two-sample, independent t-test analysis of data was conducted to compare graded dental recordings of dental hygiene students using simulated mouth models and dental hygiene students using 2D photographs.
Results
Using Microsoft Excel 2010, a t-test for independent samples assuming unequal variance was calculated. The variances were unequal based on the f-test, which resulted in a P value of .055. The t-test gave a P value of < .0001. Figure 1 illustrates mean Simulator Group (experimental) and Didactic Group (control) scores. Table 2 demonstrates a statistically significant difference in the graded dental chart scores for Simulator Group (mean = 86.73, variance = 33.84) and control (mean = 74.43, variance = 14.25). Considering this study was restricted to a small, unique population group, generalizability of the results may be limited to first-year dental hygiene students. Overall, students who identified restorations on the simulator yielded a mean 87% success rate, while those students who identified restorations using 2D photographs yielded a mean 74% success rate.
Discussion
Findings of this study reflect the collective evidence of beneficial outcomes published in current dental and healthcare simulation education literature.39-43 Comparatively, the beneficial outcomes in this and other current studies consistently demonstrate the effectiveness and major benefits of using simulation. These benefits include increasing skill acquisition before patient exposure and the ability to repeatedly practice identification skills in a safe environment. Specific diagnostic and assessment skills are especially important in dental hygiene education to ensure safe delivery of care as the evolving profession uses highly realistic restorative and prosthetic materials and conservative caries detection methods, and roles for dental hygienists continue to expand nationally.42,44 The results of this study showed diagnostic and assessment skills can be increased by using simulation, which should be adopted as a proficient learning tool to help dental hygiene students increase their success rate of providing effective, safe care for preparedness in expanding roles such as nurses used to prepare students for midwifery roles.44 Studies in nursing simulation also provide evidence similar to this study in demonstrating how low-cost, low-to-medium level fidelity simulation allows students an opportunity to increase success when learning new skills.39,44 Methods and outcomes in this study further mirrored nursing simulation studies that implemented best practices and standards for simulation use in education and research.43,45
The use of modeling and simulation has shown to be an effective method to transfer knowledge from instructor to student when compared to traditional teaching methods in dentistry.46-48 Simulators provide integration of psychomotor skill training with problem-based learning, such as didactic instruction. In this study, dental hygiene students were able to identify and correctly chart each preventive and restorative dental material based on visual, tactile, and auditory senses. This leads to improved performance when compared to isolated classroom-delivered learning. In addition, this allowed for students to become confident and proficient in critical skills necessary for successful assessment of oral conditions when evaluating live patients and in vivo scenarios.
Limitations of the study included a small sample size. Additionally, due to budget constraints, extensive restorations (such as cast porcelain and metal crowns) were not used in the simulation. Educators within the disciplines of both dental and dental hygiene curriculum may be able to use the findings of this study to improve assessment skills of students. The supporting data, which proves the effectiveness of the simulated technology, demonstrates the need for educators to consider and adopt realistic, safe, efficient, inexpensive, and effective teaching methodologies. Simulation of the oral cavity enhanced the pedagogical transfer of didactic clinical assessment and evaluation skills into a realistic scenario. Each interchangeable modified simulated mouth model served as a tool to enhance dental hygiene students’ ability to accurately identify specific dental materials and conditions. This modeling and simulation exercise will be implemented into the junior year dental hygiene preclinical laboratory course to assist students in accurately identifying dental restorations prior to actual patient care.
Conclusion
Using this type of simulation tool in conjunction with traditional teaching strategies of didactic education may allow students to physically assess, identify, and chart certain restorations presented in the clinical setting. Although using simulated mouth models is not a new concept in dental and dental hygiene education, this study reaffirms the importance and success of this type of educational tool. In this study, modified simulated mouth models improved identification and recording of dental conditions by dental hygiene students when compared to students who used 2D images. Future research should include larger sample sizes, more complex restorations, and an evaluation of the effects of experiential learning with modeling and simulation using outcomes assessment in dental hygiene education.
Disclosure
This research study was made possible through the financial support of Old Dominion University’s Center for Learning Technologies, Faculty Innovator Grant.
About the Authors
Margaret Lemaster, RDH, MS, is an Assistant Professor, Gene W. Hirschfeld School of Dental Hygiene, Old Dominion University. Joyce M. Flores, RDH, MS, is an Assistant Professor, Gene W. Hirschfeld School of Dental Hygiene, Old Dominion University. Margaret S. Blacketer, MPH, is a Senior Business Information Developer, Medicare Medical Economics, WellPoint, Inc., Norfolk, Va.
References
1. Hoffman H, Irwin A, Ligon R, et al. Virtual reality-multimedia synthesis: next-generation learning environments for medical education. J Biocommun. 1995;22(3):2-7.
2. Issenberg SB, McGaghie WC, Hart IR, et al. Simulation technology for health care professional skills training and assessment. JAMA. 1999;282(9):861-866.
3. Steadman RH, Coates WC, Huang YM, et al. Simulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skills. Crit Care Med. 2006;34(1):151-157.
4. Raemer D, Anderson M, Cheng A, et al. Research regarding debriefing as part of the learning process. Simul Healthc. 2011;6 Suppl:S52-S57.
5. Phillips J, Berge ZL. Second life for dental education. J Dent Educ. 2009;73(11):1260-1264.
6. Fanti V, Marzeddu R, Massazza G, Randaccio P. A simulation tool to support teaching and learning the operation of X-ray imaging systems. Med Eng Phys. 2005;27(7):555-559.
7. Advancing oral health in America. Choice: Current Reviews for Academic Libraries. 2012;50(1):117-118.
8. Maurette P. To err is human: building a safer health system. Ann Fr Anesth. 2002;21(6):453-454.
9. Gordon N. Learning experiences of oral hygiene students in the clinical environment. Int J Dent Hyg. 2013;11(4):267-272.
10. Della Bona A, Barrett AA, Rosa V, Pinzetta C. Visual and instrumental agreement in dental shade selection: Three distinct observer populations and shade matching protocols. Dent Mater. 2009;25(2):276-281.
11. Paravina RD, Westland S, Imai FH, et al. Evaluation of blending effect of composites related to restoration size. Dent Mater. 2006;22(4):299-307.
12. Ahn J, Lee Y. Difference in the translucency of all-ceramics by the illuminant. Dent Mater. 2008;24(11):1539-1544.
13. Lee YK, Yu B, Lee SH, et al. Shade compatibility of esthetic restorative materials—A review. Dent Mater. 2010;26(12):1119-1126.
14. Isssenberg S, Greber A. Bedside cardiology skills training for the osteopathic internist using simulation technology. J Amer Osteopath Assoc. 2003;103(12):603-607.
15. Okuda Y. The use of simulation in the education of emergency care providers for cardiac emergencies. Int J of Emerg Med. 2008;1(2):73-77.
16. DeVita MA, Schaefer J, Lutz J, et al. Improving medical emergency team (MET) performance using a novel curriculum and a computerized human patient simulator. Qual Saf Health Care. 2005;14(5):326-331.
17. Sadosty AT, Bellolio MF, Laack TA, et al. Simulation-based emergency medicine resident self-assessment. J Emerg Med. 2011;41(6):679-685.
18. Weller J, Dowell A, Kljakovic M, Robinson B. Simulation training for medical emergencies in general practice. Med Educ. 2005;39(11):1154.
19. Aoun SG, McClendon J Jr, Ganju A, et al. The Association for Surgical Education’s roadmap for research on surgical simulation. World Neurosurg. 2012;78(1-2):4-5.
20. Boyle E, O’Keeffe DA, Naughton PA, et al. The importance of expert feedback during endovascular simulator training. J Vasc Surg. 2011;54(1):240-248.
21. Rauen CA. Simulation as a teaching strategy for nursing education and orientation in cardiac surgery. Crit Care Nurse. 2004;24(3):46-51.
22. Atesok K, Mabrey JD, Jazrawi LM, Egol KA. Surgical simulation in orthopaedic skills training. J Am Acad Orthop Surg. 2012;20(7):410-422.
23. Nagle BM, McHale JM, Alexander GA, French BM. Incorporating scenario-based simulation into a hospital nursing education program. J Contin Educ Nurs. 2009;40(1):18-25.
24. Harder B. Use of simulation in teaching and learning in health sciences: a systematic review. J Nurs Educ. 2010;49(1):23-28.
25. Pilcher J, Goodall H, Jensen C, et al. Special focus on simulation: educational strategies in the NICU: simulation-based learning: it’s not just for NRP. Neonatal Netw. 2012;31(5):281-287.
26. Smith ML. Simulation and education in gynecologic surgery. Obstet Gynecol Clin North Am. 2011;38(4):733-740.
27. Morgan PJ, Cleave-Hogg D. A worldwide survey of the use of simulation in anesthesia. Can J of Anesth. 2002;49(7):659-662.
28. Maintenance of Certification in Anesthesiology. American Board of Anesthesiology [Internet]. 2014 [cited 2016 February 10]. Available from: http://www.theaba.org/MOCA/About-MOCA-2-0.
29. Benner P. Using the Dreyfus model of skill acquisition to describe and interpret skill acquisition and clinical judgment in nursing practice and education. Bulletin of Science Technology Society. 2004;24(3):188-199.
30. Falletta S. Evaluating training programs: the four levels. Am J Eval. 1998;19(2):259-261.
31. Beywl W. Evaluating training programs. The four levels. Z Eval. 2009;8(1):127-130.
32. Cox D. Experiential Learning - Experience as the Source of Learning and Development - Kolb, DA. J Coll Student Dev. 1984;25(5):481-482.
33. Benner P. Educating nurses: a call for radical transformation-how far have we come? J Nurs Educ. 2012;51(4):183-184.
34. Nelsen E, Grinder R. Experiential Learning - Experience as the Source of Learning and Development - Kolb, DA. Contemp Psychol. 1985;30(8):622-623.
35. Sugarman L. Experiential Learning - Experience as the Source of Learning and Development - Kolb, DA. J Occup Behav. 1987;8(4):359-360.
36. Crider MC, McNiesh SG. Integrating a professional apprenticeship model with psychiatric clinical simulation. J Psych Nurs Mental Hlth Svcs. 2011;49(5):42-49.
37. Jefford E, Fahy K, Sundin D. A review of the literature: midwifery decision-making and birth. Women Birth. 2010;23(4):127-134.
38. Shur Coyle J. Development of a model home health nurse internship program for new graduates: key lessons learned. J Cont Ed Nurs. 2011;42(5):201-214.
39. Brydges R, Manzone J, Shanks D, et al. Self-regulated learning in simulation-based training: a systematic review and meta-analysis. Med Educ. 2015;49(4):368-378.
40. de Boer I, Wesselink P, Vervoorn J. Evaluation of the appreciation of virtual teeth with and without pathology. Euro J Dent Ed. 2015;19(2):87-94.
41. Goulart JM, Dusza S, Pillsbury A, et al. Recognition of melanoma: a dermatologic clinical competency in medical student education. J Amer Acad Derm. 2012;67(4):606-611.
42. Perry S, Burrow M. A review of the use of simulation in dental education. Simul Healthc. 2015;10(1):31-37.
43. Shin S, Park JH, Kim JH. Effectiveness of patient simulation in nursing education: meta-analysis. Nurse Educ Today. 2015;35(1):176-182.
44. Brady S, Bogossian F, Gibbons K. The effectiveness of varied levels of simulation fidelity on integrated performance of technical skills in midwifery students—a randomised intervention trial. Nurse Educ Today. 2015;35(3):524-529.
45. Rutherford-Hemming T, Lioce L, Durham CF. Implementing the standards of best practice for simulation. Nurse Educ. 2015;40(2):96-100.
46. Bradley M, Black P, Noble S, et al. Application of teledentistry in oral medicine in a community dental service, N. Ireland. Br Dent J. 2010;209(8):399-404.
47. Clancy J, Lindquist T, Palik J. A comparison of student performance in a simulation clinic and a traditional laboratory environment: three-year results. J Dent Educ. 2002;66(12):1331-1337.
48. Buchanan J. Use of simulation technology in dental education. J Dent Educ. 2001;65(11):1225-1231.