You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Fear and anxiety regarding dentistry continue to persist despite the modern advances in local anesthetic agents.1-19 The majority of individuals admit they are fearful to some extent but many avoid dental care altogether.13,19 Using coping skills, most of the general public that have fears and anxieties are able to carry on with normal daily life. An individual with a ‘‘specific phobia’’ is defined as having a fear and anxiety that is so great it inhibits them from normal daily function.20 These patients present the greatest challenge for the dentist.
When looking at fear and anxiety toward dentistry, the majority of the general public has a low level of fear, but they are able to receive dental treatment through various coping mechanisms. A small, but significant, portion of the public has fears so great that it impedes the ability to properly maintain oral healthcare.13,19 These are the patients with a high level of fear who probably do not seek dental care on a regular basis. Between these two groups are those with moderate levels of fear and anxiety. This group may be able to tolerate minor dental treatment but have a higher level of anxiety for more involved treatment. For example, they may tolerate hygiene appointments, but may not be willing to accept other, more invasive treatments, such as a crown preparation or a root canal treatment. Patients with a moderate to high level of fear and anxiety are more likely to miss, cancel, or avoid a dental appointment.2,7,10,13,19,21,22 The majority of these fearful patients can be easily and safely treated with oral sedatives (see Table). Adults, in general, have few objections to taking medications by mouth. The oral route is widely accepted, easy, convenient, painless, and inexpensive. The use of sedatives to produce anxiolysis (minimal sedation) in healthy adults is typically safe and effective provided the appropriate dose is prescribed and adequate time is given to allow the drug to reach its peak effect.23
As with all techniques, oral sedation has its limitations, however. Oral sedation can help the majority of patients with mild to moderate levels of fear and anxiety but may be ineffective in patients with higher levels of anxiety. The practitioner must remember that a certain portion of the fearful public will not be successfully managed using oral sedation because empiric dosing is not an exact science. For these patients, dosages must be titrated intravenously. Even with intravenous sedation, there are still those who will require deeper levels of sedation, deep sedation, or general anesthesia, if dental care is to be provided successfully.
Levels of sedation progress as a continuum and each level can be achieved regardless of the route of administration. Employing oral sedation does not guarantee that a patient will be in a state of anxiolysis, nor does it guarantee that the patient will not drift into deeper levels of sedation. For this reason, patients should be treated with the lowest effective dose of the sedative agent chosen to best suit their needs. When providing sedation, the airway is always of chief concern, regardless of the level provided. While it is unlikely that appropriate doses of the drugs commonly used for oral sedation produce significant respiratory depression, it is important not to get this confused with airway obstruction; obstruction and respiratory depression are not synonymous. For example, depressing the mandible during treatment may obstruct the patient’s airway. Until this occurs, a sedated patient may breathe normally but may not initiate enough ventilatory effort to overcome this obstruction, and hypoxemia can occur. This risk for obstruction is a consideration when using any central nervous system (CNS) depressant, regardless of its ability to actually depress medullary respiratory drive.
HISTORY OF ORAL SEDATIVES
By definition, a sedative drug decreases activity, moderates excitement, and calms the recipient.24 The evolution of sedative drugs started with the introduction of fermented beverages by the Sumerians circa 9000 BC.25 Aside from nitrous oxide and ether, the modern age of sedative medications began in the 19th century with bromides and chloral hydrate. While the bromides were excellent drugs in their day, they were not often manufactured into pharmaceutically elegant products, allowing the incorporation of impurities. This worsened the already negative side effect profile of bromides, which included frequent urination, sweating, visual disturbances, and electrolyte disturbances.26
Chloral hydrate (Noctec) was synthesized in 1832 by the German chemist, Justus von Liebig, and represented the first class of sedative agents to show longevity on the mainstream pharmacopeia. Chloral hydrate is a generalized CNS depressant that acts rapidly, and if given alone, is capable of inducing deep sleep in approximately 30 minutes. It was soon discovered that chloral hydrate worked more quickly in combination with alcohol and, when slipped into whiskey, it was the ‘‘knockout drops’’ of the underworld, also called a ‘‘Mickey Finn.’’
The most popular sleeping pills of the early 20th were the barbiturates, although the progenitor of the barbiturates was actually discovered in the mid-19th century. A Prussian chemist, Adolf von Baeyer, is credited with inventing and naming barbituric acid in the early 1860s. In 1903, a student of Baeyer’s, along with another German chemist, produced a new compound out of barbituric acid and a diethyl derivative. The new chemical, given the tradename Veronal (barbital), was an excellent sedative and sleep aid. Other researchers came up with more barbituric acid derivatives; the most widely used was phenobarbital. Many European and American pharmaceutical companies developed new barbiturates in the 1920s and 1930s. The Eli Lilly Company produced the widely used Amytal (amobarbital) and Seconal (secobarbital), and Abbott Laboratories invented Pentothal (thiopental) and Nembutal (pentobarbital).
Though the barbiturates are effective sleep aids, they are not without risks. Barbiturates support addictive behavior, can have a variety of unpleasant side effects, and their effectiveness is greatly increased when taken concurrently with other CNS depressants. In fact, barbiturate sleeping pills can quickly cause death when taken with alcohol due to their significant cardiovascular and respiratory depressant effects. It is this narrow margin of safety that prompted the development of safer sedative/hypnotic medications (eg, benzodiazepines) during the next few decades. Due to their unacceptable safety profile, the use of barbiturates for sedation can no longer be recommended in most clinical situations.
BENZODIAZEPINES
The benzodiazepines and their newer derivatives are the most widely used class of drugs for anxiolysis and sedation. This is for good reason. Their efficacy is equivalent to or greater than any of the other classes of sedatives and their safety profile is enviable.
Virtually all effects of the benzodiazepines result from their specific actions on the central nervous system. They promote the binding and influence of the major inhibitory neurotransmitter, gamma-aminobutyric acid (GABA) to the GABAA subtype of GABA receptors in the brain. GABAA receptors are actually multi-subunit complexes closely associated with gated chloride ion channels within the cell membrane of neurons. When GABA activates its receptor, the channel opens and allows a greater influx of chloride ions and a more negative resting membrane potential. This renders the neuron less responsive to excitatory stimuli.
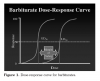
It is significant that benzodiazepines do not open the chloride channel. They bind to specific benzodiazepine (BZ) receptors on the GABAA complex, separate from the actual receptor for GABA. Activation of the BZ receptor enhances the chloride ion channel’s response to GABA, but no effect is produced if GABA is not present. A benzodiazepine agonist can only potentiate the body’s endogenous neurotransmitter. This concept is a likely explanation for the relative safety of benzodiazepines compared to chloral hydrate, barbiturates, or propofol. These other agents also have distinct receptors on the GABAA complex, but actually open the chloride channel independently of GABA. High doses of these agents may be lethal, but death following overdose of benzodiazepines alone is virtually unheard of. This wide margin of safety (high therapeutic index) for benzodiazepines is illustrated using dose-response curves (Figure 1 and Figure 2). Unlike barbiturates, illustrated in Figure 1, the effective-dose curve and the lethal-dose curve for the benzodiazepines are separated by a very large margin. Even the high doses required for our ‘‘hypo-responder’’ patients are unlikely to cross over to the lethal dose curve.
The safety and sedative efficacy of the numerous benzodiazepine formulations are virtually identical. Individual differences in the onset and duration of clinical effects are due to each drug’s unique pharmacokinetic profile. An understanding of these differences will enable the practitioner to select the right drug at the right dose for the right patient and for the right procedure.27
Diazepam (Valium)
Diazepam is often considered the prototypical benzodiazepine and the ‘‘grandfather’’ of the drug class; it has been available for more than 42 years and continues to be widely used. It is a highly lipophilic molecule resulting in fast onset of action (usually within 20 to 40 minutes), and peak plasma levels 1 to 2 hours after oral administration. It has 100% oral bioavailability and doses range from 2 mg to 10 mg for adults. The long elimination half-life of diazepam (20 to 80 hours) is due to a number of active metabolites (desmethyldiazepam and oxazepam) which may contribute to the daytime drowsiness and ‘‘hangover’’ that some may experience.28 Diazepam undergoes hepatic metabolism by oxidative reduction, and both the parent molecule and active metabolites are particularly influenced by aging, hepatic dysfunction, and drug–drug interactions.29 Given these shortcomings, the use of diazepam for oral sedation has been largely supplanted by better benzodiazepine alternatives.
Lorazepam (Ativan)
Lorazepam is considered an intermediate-acting benzodiazepine given its elimination half-life of approximately 10 to 20 hours. However, this system of classification is actually misleading. Despite a half-life shorter than diazepam, the actual sedative effect is generally longer because it has lower lipid solubility, which slows its redistribution from the brain.30 Lorazepam undergoes phase II hepatic metabolism via glucuronide conjugation to inactive metabolites that are rapidly excreted via the kidney, rather than phase I hepatic metabolism, which is affected by competition by the cytochrome P450 enzyme system and often results in active metabolites. Lorazepam is, therefore, less affected by variables such as advanced age, hepatic dysfunction, or drug–drug interactions. It has an oral bioavailability of 83% to 100% with peak plasma levels occurring 1 to 2 hours after administration. The onset of action after oral administration occurs within 60 minutes.31 The usual adult doses for dental sedation can range from as low as 0.5 mg to 4 mg depending on the patient and procedural criteria.32-34
Triazolam (Halcion)
Triazolam is widely used for the short-term treatment of insomnia. Its rapid onset, short duration of action, and lack of active metabolites makes it a near ideal antianxiety medication for dental patients.35 It is short-acting, with an onset of activity usually within 30 minutes, and with peak blood levels occurring after approximately 75 minutes. The oral bioavailability for triazolam is only 44% but it can be increased to 53% with sublingual administration.35-37
The usual adult dose for oral sedation can range from 0.125 mg to 0.5 mg.27,38 Triazolam has no active major metabolites. It is metabolized by oxidative reduction via the hepatic cytochrome P450 3A4 system and, like diazepam, it can be influenced by aging, hepatic dysfunction, and drug–drug interactions.39,40
Midazolam (Versed)
Midazolam is rapidly absorbed when administered orally either as a premixed syrup or by diluting the intravenous formulation in a pH-balanced, palatable, liquid vehicle (eg, apple juice). It has an oral bioavailability of 35% to 44% with an onset of action within 15 to 30 minutes, and peak plasma levels achieved within 20 to 50 minutes.41 Midazolam has largely replaced chloral hydrate as the medication of choice for pediatric sedation patients.35,43,44 Although, anecdotally, there have been reports of using the intravenous preparation of midazolam orally for short procedures on adults with doses at 0.25 mg/kg with a cumulative maximum of 20 mg being common, there have not been any published case series at this time to validate its effectiveness. Comparing pharmacodynamic effects, an oral dose of 0.25 mg of triazolam was found to be equivalent to oral midazolam in doses of 5 mg to 8 mg.45 Midazolam offers no advantage over triazolam for adult patients, unless they cannot swallow tablets. The actual niche for oral midazolam is for pediatric sedation and is not the focus of this article.
THE NONBENZODIAZEPINE GABA AGONISTS
Although the benzodiazepines have been touted as ideal sedative agents, the GABAA receptor complex has many subunits that make up the macromolecular structure.35 The GABAA receptor is composed of 5 subunits, with the α1, α2, α3, and α5 receptors thought to function as BZ receptor sites and mediate the clinical effects of benzodiazepines, including sedative, muscle relaxant, antiseizure, amnesic, and anxiolytic effects. However, the nonselective interaction between benzodiazepines and all of the GABA subunits may contribute to adverse drug effects, such as residual daytime sedation, cognitive impairment, rebound insomnia, and the risk of abuse. As research continues to clarify these receptor subunits, novel agonists will be developed that act more selectively.
The so-called ‘‘nonbenzodiazepine’’ hypnotics are the product of this goal, but marketing strategies are currently well ahead of actual scientific confirmation. These agents are chemically distinct from benzodiazepines. This allows them to be classified separately and be divorced from negative perceptions associated with benzodiazepines. However, they are BZ receptor agonists and their effects and clinical profiles are indistinguishable from benzodiazepines. Furthermore, their effects can be reversed using the benzodiazepine antagonist, flumazenil. They generally are claimed to have some selectivity for the α1 subunit (BZ1 receptor) described above which putatively reduces their potential for cognitive impairment and abuse.46 Whether these claims actually bear fruit remains to be seen.
Zolpidem (Ambien)
Unlike the benzodiazepines, zolpidem produces muscle relaxation and anticonvulsant effects only at doses much higher than the hypnotic dose.47 Zolpidem has a rapid onset of action, usually within 30 minutes, has a short elimination half-life and no active metabolites. This reduces the possibility of residual next-day effects from prolonged or excessive sedation. CNS depression with latent impairment of cognitive and motor function, commonly seen with barbiturates or long-acting benzodiazepines, is not common with zolpidem. Zolpidem is not contraindicated in pregnancy or in patients with narrow-angle glaucoma; both are advantages over the benzodiazepines. The usual adult dose is 10 mg, although 5-mg tablets are also available and may be recommended for elderly patients or patients on other CNS depressants.48 Flumazenil (Anexate, Romazicon) will antagonize the sedative actions of zolpidem.49 Zolpidem received Food and Drug Administration (FDA) approval in 1993 and a supplemental new drug application was filed by Biovail Pharmaceuticals in January 2002 for approval of an oral disintegrating dosage form of zolpidem. Sustained-release zolpidem (Ambien CR) was approved by the FDA on September 2, 2005, and although it has a specific role in the treatment of insomnia (‘‘controlled-release’’ to address sleep latency), this new formulation would have no role for in-office oral sedation.
Zopiclone (Imovane)
Zopiclone is another nonbenzodiazepine that produces its hypnotic effects via selective stimulation of the α1 subunit of the GABAA macromolecular complex.51 While this medication is not available in the United States, the active S-enantiomer of this molecule, eszopiclone (Lunesta), has been marketed as a hypnotic agent in its own right. Zopiclone also has a rapid onset of action, usually within 30 minutes, and a short halflife (3.5 to 5 hours) and no active metabolites. This makes its pharmacokinetic profile very similar to zolpidem. The average adult dose is 7.5 mg to 15 mg, and it is available as 5-mg and 7.5-mg tablets. Flumazenil will also antagonize the sedative actions of zopiclone.52
Eszopiclone (Lunesta)
Eszopiclone is one of the most recent additions to the nonbenzodiazepine class of sedative agents. As such there are very few data on its use in the dental realm. Its pharmacokinetic profile is similar to that of the parent compound, zopiclone, because eszopiclone is simply the S-enantiomer of the parent compound zopiclone. As such, flumazenil would also antagonize the sedative actions of eszopiclone.52 Eszopiclone was approved by the FDA in December 2004.53,54
Zaleplon (Sonata, Starnoc)
Zaleplon (Sonata, Starnoc) is a short-acting, nonbenzodiazepine sedative-hypnotic that also possesses anticonvulsant, anxiolytic, hypnotic, and myorelaxant properties. Zaleplon was FDA-approved in 1999 and has a faster onset of action and a shorter terminal elimination half-life than zolpidem. Zaleplon is available in 5-mg and 10-mg capsules and the usual dosing range is from 5 mg to 20 mg.55 In Japanese adults (and possibly other Asian populations), the maximum concentration in the blood (Cmax) as well as the total amount of drug absorbed from a single dose of zaleplon were increased 37% and 64%, respectively. This is likely due to differences in body weight or may represent differences in enzyme activities resulting from differences in diet, environment, or other factors. More conservative dosing of zaleplon in this patient population would be prudent. Flumazenil can also antagonize the sedative actions of zaleplon.56 Indiplon is from the same drug class as zaleplon and was being coproduced by Pfizer and Neurocrine Biosciences Inc to compete with Ambien and Lunesta.57 By early 2006, however, they had failed to win federal regulatory approval in the United States, yet literature citing this drug’s efficacy from other countries continues to populate the medical literature.58
Ramelteon (Rozerem)
Ramelteon is the first drug in the melatonin receptor agonist class of hypnotic therapies that has recently been FDA-approved for insomnia management and works by a completely different mechanism than all the medications discussed thus far.59 The melatonin MT1 and MT2 receptors are thought to be involved in the maintenance of circadian rhythm, which regulates the sleep-wake cycle.60 Ramelteon has high selectivity and affinity for melatonin MT1 and MT2 receptors which is believed to contribute to its sedation-promoting properties. Since its approval for the treatment of insomnia in 2005, ramelteon has been found to be very useful in treating patients having difficulty with sleep onset. The utility of this medication in the dental realm is slowly gaining interest, as this is the only sedative medication described thus far that is not a federally controlled substance. The unique and targeted mechanism of action of this drug also limits its side effect profile; it is not associated with an abuse potential or ‘‘hangover’’ effect often found with other sedatives. Ramelteon has no measurable affinity for the GABA receptor complex, dopamine, or opiate receptors. Ramelteon is available as 8-mg tablets and has an average onset of action of approximately 30 minutes and an elimination half-life of 2.6 to 5 hours.61 Ramelteon does not offer the benefit of anterograde amnesia found with benzodiazepines or other nonbenzodiazepine agents discussed thus far. Its action cannot be reversed by flumazenil.
THE ANTIHISTAMINES
While antihistamines are primarily used to manage allergic type reactions, they also cause sedation as a side effect. The strong calming and sleep-inducing effects of Atarax, Benadryl, and Phenergan in particular led to these medications being marketed as sedative-hypnotics in addition to some of their other effects in preventing nausea, vomiting, and the adverse sequelae of allergic reactions. The actual sedative efficacy of these agents is generally less than that with benzodiazepines.
Hydroxyzine (Atarax, Vistaril) is an antihistamine (H1-antagonist) sedative which has an onset of action within 15 to 30 minutes. The maximum effect is achieved after approximately 2 hours, and drug effect wanes after 3 to 4 hours. The incidence of side effects with hydroxyzine is low. Other than drowsiness, hydroxyzine has minimal effect on cardiovascular or respiratory function. Usual adult doses range from 50 mg to 100 mg.62
Diphenhydramine (Benadryl) is an H1-antagonist of the ethanolamine class. Other members of this group include carbinoxamine, clemastine, dimenhydrinate (a salt of diphenhydramine), doxylamine, phenyltoloxamine, and others. Ethanolamine H1-antagonists have significant antimuscarinic activity and produce marked sedation in most patients. Diphenhydramine is a popular antihistamine due to its relative safety after oral or parenteral administration. In addition to the usual allergic symptoms, the drug also treats irritant cough, although the airway drying effect may be counterproductive. Because of its anticholinergic properties, diphenhydramine is effective in the relief of nausea, vomiting, and vertigo associated with motion sickness.63
Diphenhydramine was originally approved by the FDA in 1946 as a prescription-only drug but was later changed to nonprescription, over-the-counter (OTC) status. Due to its ability to induce drowsiness, it is also promoted as an OTC hypnotic (Sominex). The onset of action following oral administration of diphenhydramine occurs in 15 to 30 minutes, with peak concentrations occurring in about 2 to 4 hours. Typical adult doses for sedation are 25 mg to 50 mg.64
Promethazine (Phenergan) has been available since 1951 and although it has long been used as a sedative agent, it is a phenothiazine as well as an antihistamine. It has considerable anticholinergic, sedative, antiemetic, and some local anesthetic properties. In November 2004 the FDA directed manufacturers of promethazine to include a Black Box warning contraindicating its use in children 2 years of age given the increased risk for fatal respiratory depression in these very young children. Typical adult doses for sedation are 25 mg to 50 mg.65
THERAPEUTIC CONSIDERATIONS
The most common use of oral sedation in adults is for the reduction of anxiety preceding and during the dental appointment. For some, the use of oral sedation the night before their appointment can ensure a more restful sleep leading to a more pleasant and relaxed patient for the dental appointment.66
Due to the varying recovery profiles of many different sedative agents available, the patient should be advised not to drive, make important decisions, or consume alcohol for a period of 24 hours after the appointment. This requires the patient to have an escort who must be a responsible adult. It would be ill-advised to allow a patient to leave the office unaccompanied.
On the day of the appointment, it would be prudent to administer the medication in the dental office where it is a controlled and monitored environment. Advantages of this protocol include the following:
1. The escort can be confirmed. Although a common scenario would be to have the patient take the sedative at home 1 hour prior to the start of the appointment, it may be beneficial to administer the medication at the dental office. Administering the medication in the office while supervised allows for the confirmation of the amount taken and can prevent the patient from self-medicating prior to arriving at the office and forgetting that an escort is needed, thereby driving unescorted to the dental office.
2. Written consent, if needed or required, can be obtained prior to administration of the sedative. Depending on the state or province, a practitioner may be required to obtain written informed consent that allows dental treatment while the patient is in an altered state of consciousness. If the patient were to take the oral sedative prior to arriving at the office, the informed consent must be acquired on a previous appointment.
3. Any change or confirmation of dental work that is or is not to be completed during the appointment can be confirmed prior to the administration of the sedative.
Selecting the Medication
It is important for the clinician to choose the sedative agent that will best suit the patient based on the patient’s age, weight, and medical history rather than solely based of the length of time required for the dental treatment. The choice of the drug also depends on the familiarity of the drug to the practitioner. The absolute contraindication of any medication is the lack of knowledge of the pharmacology of that drug.
Because all patients will react differently to medications, it would be prudent to start with a shorter appointment and with treatment that is not too invasive in order to gauge the appropriateness of the chosen sedative agent. The amount administered should always be the lowest effective dose. For the first appointment, the dentist should consider starting with the lowest dose that is known to be effective. Discussions with the patient the day after the initial sedation appointment will help to determine if the oral sedative used is appropriate in dose and type. What the physician deems as an adequate or inadequate dosage may actually differ from the patient’s own experience of the appointment.67 If the initial dose proves to be inadequate, the amount given can be increased during subsequent appointments. Although the weight of the patient can be useful in determining the initial dose, the level of fear and anxiety may be a more accurate determinant. At this time, however, there are few data that correlate the level of fear and the appropriate dose of an oral sedative.
The myriad of benzodiazepines and related agents have comparable efficacy and the one selected is most likely predicated on its pharmacokinetic properties. These will predict an onset and duration most appropriate for the treatment session. The following are a few examples.
For short dental procedures (1 hour), the use of zaleplon has been shown to be effective. A study by Ganzberg et al has shown good efficacy with the use of zaleplon (Starnoc, Sonata) in patients for third-molar extraction. This study demonstrated efficacy comparable to triazolam and a faster recovery from the sedation in the zaleplon arm of the study.68 For very short dental appointments, zaleplon 10 mg to 20 mg given 1 hour prior to the procedure may provide adequate sedation.
For dental procedures of moderate length (1 to 2 hours), triazolam (Halcion), a short-acting benzodiazepine, in the dose of 0.125 mg to 0.5 mg, can be given 1 hour before the procedure. Triazolam is a popular choice among clinicians due to its anxiolytic, hypnotic, and amnesic effects, which are desirable in dental patients. It has a relatively short half-life with little residual hangover effects the next day.
For longer appointments (2 to 4 hours), a longer-acting benzodiazepine such as lorazepam (Ativan) may be prescribed. Oral lorazepam in the dose of 1 mg to 4 mg may be given 1 to 2 hours prior to the dental procedure or 30 to 60 minutes prior for the sublingual preparation.
The antihistamines have also been used as sedatives for short to long dental procedures. Diphenhydramine (Benadryl) may be prescribed in the dose of 50 mg 1 hour prior to the dental procedure. Hydroxyzine (Atarax), with a longer half-life than diphenhydramine, can be given in the dose of 50 mg to 100 mg 1 hour before the appointment. Yet another antihistamine with a similar half-life as hydroxyzine is promethazine (Phenergan), and it is typically given in a dose of 25 mg to 50 mg 1 hour prior to the procedure. Be aware that patients may experience anticholinergic side effects such as dry mouth, and for patients with angle-closure glaucoma, these antihistamines should be avoided.69
Geriatric Patients
The patient’s age is important in the selection of an oral sedative drug and dosage. For geriatric patients, many physiological and psychological changes take place with age, such as decreased cerebral blood flow, cardiac output, renal and hepatic blood flow, and pulmonary function. Furthermore, these individuals tend to suffer from at least one chronic condition such as heart disease, hypertension, arthritis, osteoporosis, and noninsulin-dependent (type 2) diabetes mellitus, all requiring long-term control with drug therapy and, occasionally, surgery. In addition, there are also pharmacodynamic and pharmacokinetic differences in elderly patients.
Pharmacokinetically, oral absorption, hepatic metabolism, and renal clearance all decrease with age. Pharmacodynamically, oral sedatives and other CNS depressants tend to have a greater effect in the elderly. This, together with polypharmacy in this patient population, contributes to the lower dosages and shorter-acting medications that are typically required in order to avoid oversedation.70
A suggested short-acting benzodiazepine such as triazolam in a starting dosage of 0.125 mg to 0.25 mg given 1 hour before the dental appointment may be effective. For short appointments, another shorter acting (nonbenzodiazepine) alternative is zaleplon in a starting dose of 10 mg, or zolpidem regular release in a dose of 5 mg to 10 mg 1 hour prior to the appointment may be used. Alternatively, for longer appointments, a longer-acting benzodiazepine such as lorazepam may be prescribed. Oral lorazepam in the dose of 0.5 mg to 1 mg may be given 1 to 2 hours before or 30 to 60 minutes before the dental procedure for the sublingual preparation. Diazepam has a long half-life that is further extended in elderly patients; thus, its use in these individuals is not recommended.
The antihistamines are typically longer acting and have anticholinergic side effects that are less desirable in geriatric patients, those at risk for falls, and especially those with glaucoma or evidence of dementia.
MEDICALLY COMPROMISED PATIENTS
Patients with underlying medical conditions will often benefit from oral sedation to minimize preoperative anxiety. Medical consultation is often recommended to understand the severity and stability as well as the treatment and control of any existing conditions prior to the administration of oral sedative drugs.
Cardiovascular Disease
Anxiety and pain increase heart rate and blood pressure, leading to an increased oxygen demand of the myocardium. With coronary artery disease, this increased oxygen requirement may not be met, and episodes of angina and dysrhythmias can result. The use of sedation as well as excellent pain control both during and after the appointment are of increasing importance. These patients often benefit from oral sedation due to the decreased stress of the appointment especially during long or traumatic appointments. Excessive sedation can cause significant respiratory depression leading to hypoxia and subsequent myocardial ischemia. The use of supplemental oxygen should be considered even with mild sedation. Adequate pain control through profound local anesthesia as well as postoperative pain control with nonsteroidal anti-inflammatory drugs (NSAIDs) and opioids are important for patients with cardiovascular disease. All of these considerations are also applicable to patients with hypertension.
Renal and Hepatic Disease
The benzodiazepines are generally safer than other antianxiety agents and short-term administration is effective. Because of the potential for drug or metabolite accumulation, chronic use of these agents is discouraged. For single doses used in oral sedation, no dose adjustment of the benzodiazepines is required. Chloral hydrate, however, is renally cleared and its use should be avoided in these patients.71
Respiratory Disease
Minimal oral sedation in the usual doses is safe and beneficial for patients with asthma or chronic obstructive pulmonary disease (COPD). Stress can be a trigger for bronchospasm in patients with asthma as well as in patients with chronic bronchitis. The anticholinergic effects of the antihistamines may not only be desirable in these patients but may be of great benefit. The other oral sedatives such as the benzodiazepines can also be readily used.
Epilepsy
Minimal oral sedation may also be of benefit to this group of patients. The benzodiazepines have anticonvulsant activity and are often the drugs of choice for these patients. With unintentional oversedation, supplemental oxygen should be given to avoid hypoxia that can trigger a seizure. Some antiepileptic drugs (eg, phenytoin, carbamazepine, phenobarbital, valproic acid) are hepatic enzyme inducers that may increase the clearance of oral sedative drugs, thereby shortening their duration of action.
Diabetes Mellitus
Oral sedation can be used in patients with type 1 or type 2 diabetes mellitus. It is important to remind patients to maintain their caloric intake and their regular meals both before and after the appointment. If they sleep through a meal or do not eat their regular full meal due to the sedation, then the doses of their insulin or their oral hypoglycemic medication may need to be adjusted. Appointments for patients with diabetes should be kept short to prevent long periods of fasting. Keep in mind that signs and symptoms of hypoglycemia, such as altered mental state and fatigue, can be easily confused with an exaggerated response to CNS depressants.
Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) affects 2% to 4% of middle-aged adults.72 It is defined as apnea events lasting 10 seconds or longer that occur 5 times or more per hour during sleep.73 OSA can lead to hypoxemia, hypercarbia, polycythemia, systemic and pulmonary hypertension, and right ventricle failure. During rapid eye movement (REM) sleep, muscles that usually stent the airway open are relaxed. This results in significant narrowing of the airway. Patients with OSA are extremely sensitive to CNS depressants and are at risk for upper airway obstruction even with minimal doses of these drugs.74 Treatment of patients with OSA using oral sedatives should be approached with caution as a loss of the airway can readily occur in this patient population. The use of supplemental oxygen is encouraged.
CONCLUSION
This overview is intended as an introduction to minimal oral sedation (anxiolysis) in the dental office and is not meant to replace continuing education taught by those with advanced training in this area. Using oral sedation techniques will allow patients to visit the dentist in a stress-reduced state, where their fear and anxiety would otherwise impede their ability to seek and maintain proper oral healthcare. To date, this modality has been proven to be not only safe but very effective. Proper medication selection and patient management, however, are paramount to maintaining this safe practice.
ABOUT THE AUTHORS
Dr. Donaldson is the Director of Pharmacy Services at Kalispell Regional Medical Center, and a clinical assistant professor in the School of Dentistry, Oregon Health & Sciences University, Portland, Oregon. Dr. Gizzarelli is a pharmacist at Toronto General Hospital, University Health Network, Toronto, Ontario, Canada. Dr. Chanpong is a clinical assistant professor on the Faculty of Dentistry, University of British Columbia, Vancouver, British Columbia, Canada.
REFERENCES
1. Friedson E, Feldman JJ. The public look at dental care. J Am Dent Assoc. 1958;57(3):325-335.
2. Gatchel RJ, Ingersoll BD, Bowman L, et al. The prevalence of dental fear and avoidance: a recent survey study. J Am Dent Assoc. 1983;107(4):609-610.
3. Milgrom P, Fiset L, Melnick S, Weinstein P. The prevalence and practice management consequences of dental fear in a major US city. J Am Dent Assoc. 1988;116(6):641-647.
4. Gatchel RJ. The prevalence of dental fear and avoidance: expanded adult and recent adolescent surveys. J Am Dent Assoc. 1989;118(5):591-593.
5. Stouthard ME, Hoogstraten J. Prevalence of dental anxiety in The Netherlands. Community Dent Oral Epidemiol. 1990;18(3):139-142.
6. Teo CS, Foong W, Lui HH, et al. Prevalence of dental fear in young adult Singaporeans. Int Dent J. 1990;40(1):37-42.
7. Domoto P, Weinstein P, Kamo Y, et al. Dental fear of Japanese residents in the United States. Anesth Prog. 1991;38(3):90-95.
8. Hakeberg M, Berggren U, Carlsson SG. Prevalence of dental anxiety in an adult population in a major urban area in Sweden. Community Dent Oral Epidemiol. 1992;20(2):97-101.
9. Moore R, Birn H, Kirkegaard E, et al. Prevalence and characteristics of dental anxiety in Danish adults. Community Dent Oral Epidemiol. 1990;21(5):292-296.
10. Weinstein P, Shimono T, Domoto P, et al. Dental fear in Japan: Okayama Prefecture school study of adolescents and adults. Anesth Prog. 1993;39(6):215-220.
11. Ronis DL. Updating a measure of dental anxiety: reliability, validity, and norms. J Dent Hyg. 1994;68(5):228-233.
12. Hagglin C, Berggren U, Hakeberg M, Ahlqwist M. Dental anxiety among middle-aged and elderly women in Sweden. A study of oral state, utilisation of dental services and concomitant factors. Gerodontology. 1996;13(1):25-34.
13. Dionne RA, Gordon SM, McCullagh LM, Phero JC. Assessing the need for anesthesia and sedation in the general population. J Am Dent Assoc. 1998;129(2):167-173.
14. Doerr PA, Lang WP, Nyquist LV, Ronis DL. Factors associated with dental anxiety. J Am Dent Assoc. 1998;129(8):1111-1119.
15. Kaakko T, Milgrom P, Coldwell SE, et al. Dental fear among university students: implications for pharmacological research. Anesth Prog. 1998;45(2):62-67.
16. Ragnarsson E. Dental fear and anxiety in an adult Icelandic population. Acta Odontol Scand. 1998;56(2):100-104.
17. Jeske AH. Xylocaine: 50 years of clinical service to dentistry. Tex Dent J. 1998;115(5):9-13.
18. Thomson WM, Locker D, Poulton R. Incidence of dental anxiety in young adults in relation to dental treatment experience. Community Dent Oral Epidemiol. 2000;28(4):289-294.
19. Chanpong B, Haas DA, Locker D. Need and demand for sedation or general anesthesia in dentistry: a national survey of the Canadian population. Anesth Prog. Spring 2005;52(1):3-11.
20. Task Force on DSM-IV APA. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. 4th ed. Washington, DC: American Psychiatric Association; 2000.
21. Locker D, Liddell A, Burman D. Dental fear and anxiety in an older adult population. Community Dent Oral Epidemiol. 1991;19(2):120-124.
22. Taani DSMQ. Dental fear among a young adult Saudian population. Int Dent J. 2001;51:62-66.
23. Malamed SF. Sedation and safety: 36 years of perspective. Alpha Omegan. 2006;99(2):70-74.
24. Charney DS, Mihic SJ, Harris RA. Hypnotics and sedatives. In: Brunton LL, Lazo JS, Parker KL, eds. Goodman and Gilman’s the Pharmacological Basis of Therapeutics. 11th ed. Los Angeles, Calif: McGraw Hill; 2006:401.
25. Coppa A, Bondioli L, Cucina A, et al. Palaeontology: early Neolithic tradition of dentistry. Nature. 2006;440(7085):755-756.
26. Consensus Development Panel, Freedman D, chair. Drugs and insomnia: the use of medications to promote sleep. JAMA. 1984;251:2411.
27. Dionne R, Yagiela J, Donaldson M, et al. Balancing efficacy and safety in the use of oral sedation in dental outpatients. J Am Dent Assoc. 2006;137:502-513.
28. Valium [package insert]. Nutley, NJ: Roche Pharmaceuticals Inc; 2000.
29. Jacobi J, Fraser GL, Coursin DB, et al. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med. 2002;30(1):119-141.
30. Seppala K, Korttila K, Hakkinen S, Linnoila M. Residual effects and skills related to driving after a single oral administration of diazepam, medazepam or lorazepam. Br J Clin Pharmacol. 1976;3(5):831-841.
31. Ameer B, Greenblatt DJ. Lorazepam: a review of its clinical pharmacological properties and therapeutic uses. Drugs. 1981;21:162.
32. Goodchild JH, Donaldson M. Calculating and justifying total anxiolytic doses of medications for in-office use. Gen Dent. 2006;54:54-57.
33. Donaldson M, Goodchild JH. Maximum cumulative doses of sedation medication for in-office oral conscious sedation. Gen Dent. 2007;55(2):143-149.
34. O’Boyle CA, Barry H, Fox E, et al. Controlled comparison of a new sublingual lormetazepam formulation and i.v. diazepam in outpatient minor oral surgery. Br J Anaesth. 1988;60(4):419-425.
35. Dionne RA, Trapp LD. Oral and rectal sedation. In: Dionne RA, Phero JC, Becker DE, eds. Management of Pain and Anxiety in the Dental Office. St. Louis, Mo: WB Saunders; 2002:229.
36. Jackson DL, Milgrom P, Heacox GA, Kharasch ED. Pharmacokinetics and clinical effects of multidose sublingual triazolam in healthy volunteers. J Clin Psychopharmacol. 2006;26(1):4-8.
37. Scavone JM, Greenblatt DJ, Friedman H, Shader RI. Enhanced bioavailability of triazolam following sublingual versus oral administration. J Clin Pharmacol. 1986;26:208-210.
38. Berthold CW, Dionne RA, Corey SE. Comparison of sublingually and orally administered triazolam for premedication before surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:119-124.
39. Feck AS, Goodchild JH. Rehabilitation of a fearful dental patient with oral sedation: utilizing the incremental oral administration technique. Gen Dent. 2005;53(1):22-26.
40. American Hospital Formulary Service Drug Information. 2005. Bethesda, MD: American Hospital Formulary Service Drug Information; 2005:2252-2260.
41. Greenblatt DJ, Harmatz JS, von Moltke LL, et al. Age and gender effects on the pharmacokinetics and pharmacodynamics of triazolam, a cytochrome P450 3A substrate. Clin Pharmacol Ther. 2004;76(3):467-479.
42. Allonen H, Ziegler G, Klotz U. Midazolam kinetics. Clin Pharmacol Ther. 1981;30:653.
43. Kupietzky A, Houpt MI. Midazolam: a review of its use for conscious sedation of children. Pediatr Dent. 1993;15:237.
44. Malinovsky JM, Populaire C, Cozian A. Premedication with midazolam in children. Effect of intranasal, rectal and oral routes on plasma midazolam concentrations. Anaesthesia. 1995;50:351.
45. Sostmann HJ, Sostmann H, Crevoisier C, et al. Dose equivalence of midazolam and triazolam: a psychometric study based on flicker sensitivity, reaction time and digit symbol substitution test. Eur J Clin Pharmacol. 1989;36:181-187.
46. Charney DS, Mihic SJ, Harris RA. Hypnotics and sedatives. In: Brunton LL, Lazo JS, Parker KL, eds. Goodman and Gilman’s the Pharmacological Basis of Therapeutics. 11th ed. Los Angeles, Calif: McGraw Hill; 2006:401-413.
47. Holm KJ, Goa KL. Zolpidem: an update of its pharmacology, therapeutic efficacy and tolerability in the treatment of insomnia. Drugs. 2000;59:865.
48. Ambien [package insert]. Bridgewater, NJ: Sanofi-Aventis; 2006.
49. Langtry HD, Benfield P. Zolpidem: a review of its pharmacodynamics and pharmacokinetic properties and therapeutic potential. Drugs. 1990;40:291.
50. Ambien CR for insomnia. Medical Letter. 2005;47:97.
51. Drover DR. Comparative pharmacokinetics and pharmacodynamics of short-acting hypnosedatives: zaleplon, zolpidem and zopiclone. Clin Pharmacokinet. 2004;43(4):227-238.
52. Cienki JJ, Burkhart KK, Donovan JW. Zopiclone overdose responsive to flumazenil. Clin Toxicol. 2005;43(5):385-386.
53. Krystal AD, Walsh JK, Laska E. Sustained efficacy of eszopiclone over 6 months of nightly treatment: results of a randomized, double-blind, placebo-controlled study in adults with chronic insomnia. Sleep. 2003;26:793.
54. Najib J. Eszopiclone, a nonbenzodiazepine sedativehypnotic agent for the treatment of transient and chronic insomnia. Clin Ther. 2006;28(4):491-516.
55. Sonata [package insert]. Bristol, Tenn: King Pharmaceuticals; 2006.
56. Drover DR. Comparative pharmacokinetics and pharmacodynamics of short-acting hypnosedatives: zaleplon, zolpidem and zopiclone. Clin Pharmacokinet. 2004;43(4):227-238.
57. Petroski RE, Pomeroy JE, Das R, et al. Indiplon is a high-affinity positive allosteric modulator with selectivity for alpha1 subunit-containing GABAA receptors. J Pharmacol Exp Ther. 2006;317(1):369-377.
58. Neurocrine Announces Submission of New Drug Application for Indiplon Capsules. Available at: http://www.neurocrine.com/html/clin_insomnia.html. Accessed January 9, 2007.
59. Kato K, Hirai K, Nishiyama K, et al. Neurochemical properties of ramelteon (TAK-375), a selective MT1/MT2 receptor agonist. Neuropharmacology. 2005;48(2):301-310.
60. Turek FW, Gillette MU. Melatonin, sleep, and circadian rhythms: rationale for development of specific melatonin agonists. Sleep Med. 2004;5(6):523-532.
61. Rozerem [package insert]. Lincolnshire, Ill Takeda Pharmaceuticals Inc; 2005.
62. Skidgel RA, Erdos EG. Histamine, bradykinin, and their antagonists. In: Brunton LL, Lazo JS, Parker KL, eds. Goodman and Gilman’s the Pharmacologic Basis of Therapeutics. 11th ed. New York, NY: McGraw-Hill; 2006:629-651.
63. Rickels K, Morris RJ, Newman H, et al. Diphenhydramine in insomniac family practice patients: a double-blind study. J Clin Pharmacol. 1983;23:234-242.
64. Physicians’ Desk Reference. 61st ed. Montvale, NJ: Thompson Co; 2006:1868.
65. Bender BG, Berning S, Dudden R, et al. Sedation and performance impairment of diphenhydramine and second-generation antihistamines: a meta-analysis. J Allergy Clin Immunol. 2003;111:770-776.
66. Malamed SF. Sedation: A Guide to Patient Management. 4th ed. St. Louis, Mo: Mosby; 2002:105.
67. Dionne RA, Yagiela JA, Moore PA, et al. Comparing efficacy and safety of four intravenous sedation regimens in dental outpatients. J Am Dent Assoc. 2001;132(6):740-751.
68. Ganzberg SI, Dietrich T, Valerin M, Beck FM. Zaleplon (Sonata) oral sedation for outpatient third molar extraction surgery. Anesth Progr. 2005;52(4):28-31.
69. McEvoy GK, ed. American Hospital Formulary Service Drug Information. Bethesda, Md: American Society of Health-System Pharmacists; 2007.
70. Stoelting RK, Dierdorf SF. Diseases associated with aging. In: Anesthesia and Co-Existing Disease. 4th ed. Philadelphia, PA: Churchill Livingstone; 2002:740.
71. Aronoff GR, Berns JS, Brier ME, et al. Drug Prescribing in Renal Failure. 4th ed. Philadelphia, Pa: American College of Physicians; 1999.
72. Strollo PJ, Rogers RM. Obstructive sleep apnea. N Engl J Med. 1996;334:99-104.
73. Stoelting RK, Dierdorf SF. Nutritional diseases and inborn errors of metabolism. In: Anesthesia and Co-Existing Disease. 4th ed. Philadelphia, Pa: Churchill Livingstone; 2002:444.
74. Stoelting RK, Dierdorf SF. Nutritional diseases and inborn errors of metabolism. In: Anesthesia and Co-Existing Disease. 4th edition. Philadelphia, Pa: Churchill Livingstone; 2002:445.