You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The close relationship between diet and oral health is well-established, with a wealth of information demonstrating the impact that diet has on dental diseases, in particular dental caries and erosion.1-3 Dental caries occurs when bacteria in the oral cavity metabolize fermentable carbohydrates and organic acids are produced, causing demineralization of hard tooth structure.1 This process depends on the presence of fermentable carbohydrates, thus being directly associated with diet. While dental caries incidence in Australia has decreased significantly over the last 30 years, this trend seems to have reached a plateau, and the caries incidence in many population subgroups remains unacceptably high.4 Early childhood caries (ECC) is particularly concerning as it is characterized by severe, rampant caries in the teeth of young children and is closely associated with infant feeding practices.5 Dental erosion is the loss of hard tooth structure due to acid destruction, the most common cause being dietary acids.1 Dental erosion appears to be a growing issue, and it has been hypothesized that this rise in prevalence is due to an increased consumption of acidic drinks.6 As well as contributing to the development of oral health problems, diet also has a direct effect on general health. Poor diet has been shown to contribute to systemic health problems such as obesity, diabetes, and cardiovascular disease.7 With an increasing body of evidence linking oral health to general health, the issue of diet and oral health is a major concern for dental professionals and should become a major focus in the treatment of patients.8
Watt et al suggest that dietary advice is likely to be more effective if a team approach is adopted.9 Dental hygienists traditionally have a preventive role on the dental team and may be ideally suited to providing dietary advice. While dentists often face time constraints, dental hygienists commonly see patients for longer appointments on a somewhat regular basis, which puts them in an ideal position to assess patients’ dietary habits and to provide appropriate advice.10 A recent study examining the attitudes of dental hygienists in North Carolina established that 95% of respondents believed that dental hygienists should play a role in helping patients make dietary changes.11 Interestingly, a study investigating the self-reported dietary counseling practices of Oregon dental hygienists observed that only 53% of dental hygienists provided any dietary advice to patients.10 These results were reiterated by a more recent survey of Maryland dental hygienists which established that nutritional counseling was only provided by 65% of respondents in the prevention of ECC.12 These results are concerning, considering the crucial role that diet plays in the development of ECC.13 It appears that while the majority of dental hygienists agree that they should have a role in providing dietary education it is implemented infrequently in practice.
Despite the belief that they should be providing dietary advice, the infrequent provision of dietary advice by dental hygienists leads to the speculation that barriers exist to dietary advice provision. Research demonstrates that there is a correlation between the perceived extent of training and dental hygienists’ confidence in providing dietary advice.10,11 Therefore, it would be valuable to review the content and application of dental hygiene curricula to ensure that dental hygienists are adequately trained and experienced in dietary counseling. Barriers to the provision of dietary advice identified by dental hygienists include minimal observed financial gain, dietary advice not fitting into routine patient scheduling, and lack of financial reimbursements from health insurance companies.10 In addition to practice barriers, patient factors may also limit the frequency with which dietary advice is provided. Sarmadi et al reported that girls received dietary advice slightly more frequently than boys; however, this relationship was not significant.14 Minimal research has examined whether provision of dietary advice by dental hygienists is influenced by different patient factors such as age and gender.
A recent Cochrane Review, which investigated the effectiveness of one-to-one dietary interventions, found that a significant change in dietary behavior was observed in participants in four of the five studies reviewed.15 However, due to the limited research available, strong evidence is lacking. While the Cochrane Review provides a useful overview of the effectiveness of dietary interventions, the question of frequency of dietary advice provision by dental hygienists seems to be a somewhat overlooked issue.
Dental hygiene students are a useful group to research as they are a group that is closely supervised by clinical faculty and are required to follow strict guidelines about the treatment they provide. It can be assumed that dental hygiene students’ treatment follows the current body of research and, therefore, that students frequently incorporate dietary advice into their practices. In Australia, where this study was conducted, the Australian Dental Council requires newly graduated dental hygienists to be able to “identify the impact of environmental and lifestyle factors and the determinants of health on oral health and implement strategies to positively influence these interactions” as per the Professional Attributes and Competencies.16 Thus, the aim of this study was to assess the frequency of dietary advice provision by dental hygiene students and to investigate factors influencing the frequency that dietary advice is provided.
Methods and Materials
Study Design
This study used a retrospective cross-sectional design to examine the frequency that dietary advice was provided by students in their third year of a Bachelor of Oral Health at the University of Newcastle. In addition, the study also examined whether different patient factors were associated with the frequency of dietary advice provision. Ethics approval was obtained from the University of Newcastle Ethics Committee in 2013.
Setting
Individuals wishing to register as a dental hygienist in Australia must complete a 3-year Bachelor of Oral Health degree or 2-year Advance Diploma. The Oral Health program at the University of Newcastle is based at the Ourimbah campus on the New South Wales (NSW) Central Coast and involves an integration of oral health sciences and clinical placements, with a focus on population health.
Participants
Participants included in the study were all third-year Bachelor of Oral Health students who were currently enrolled at the Ourimbah campus of the University of Newcastle, as well as all patients seen by this cohort at the university clinic in 2012. No exclusion criteria were applied to the selection of students or patients to reduce selection bias.
Within the curriculum, all participants had completed sessions on diet and nutrition and its impact on oral health, and were encouraged during clinical sessions to explore the role of diet and oral disease with their patients. All data was de-identified by a third party, with patient names, times, and identifiable details removed from the extracted data before analysis. As the data was de-identified, no information about any of the participants or patients was accessible and, therefore, no participants were identifiable in the results. Students were not advantaged or disadvantaged by the study, as they were not identifiable in the data and were not directly involved in the study.
Data Collection
The study used de-identified data retrieved from Dental4Windows, an electronic dental program used in the university dental clinic. Dental4Windows is a popular dental program that allows dental practitioners to enter clinical notes and item numbers and make appointment bookings for patients. This study was interested in examining the age and gender of patients and the treatment they received on each visit to the clinic.
The dependent variable was the frequency of the use of the item number 131 (representing dietary advice, where at least 15 minutes of dietary advice is provided). This was measured by assessing how frequently the item number was entered into Dental4Windows by third-year dental hygiene students over the study period. Dental item numbers are used in Australia as a uniform system of recording services provided by dental practitioners and are used by private health insurance companies, as well as Medicare, to allow efficient processing of dental claims.
The independent variables measured included other services provided at that appointment (in the form of item numbers), as well as the age and gender of patients. The reason for recording these variables is to get an understanding of which, if any, patient factors influenced whether different patients receive dietary advice and how frequently.
Data Analysis
Data analysis was completed using the statistics program STATA® version 12 (Statcorp, www.statcorpmedical.com). Frequencies were displayed as percentages. More complex analysis of data was completed using regression analysis. Regression analysis was used to describe the relationship between dietary advice and variables including age, gender, and other treatment provided; logistic regression allows the dependent variable to be defined and correlating predictions to be made.17
Results
Patient Demographics
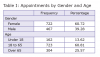
Data was extracted from Dental4Windows in August 2013. The data comprised information about all patients seen by third-year oral health students during 2012. The extracted data consisted of de-identified patient information, including year of birth, gender, and treatment provided, in the form of item numbers. Third-year oral health students saw a total of 1,189 patients over the 12-month study period. Of these, 722 patients were female and 467 were male. Table 1 describes the gender distribution of patients seen over the 12-month study period. The ages of the patients seen were categorized into three age ranges: younger than 18 years old, 18 to 65 years old, and older than 65 years old (Table 1). The largest proportion of patients seen during the 12 months was adults aged 18 to 65 (n = 723, 60.81%). Approximately one quarter of the patients who attended the university clinic were older than 65 years of age (n = 304, 25.57%). Patients seen least frequently were children or adolescents under the age of 18 (n = 162, 13.62%).
Treatments Provided to Patients
The treatment provided most often by dental hygiene students was oral hygiene instruction (n = 754, 63.41%), with the least frequent treatment provided being saliva testing (n = 11, 0.93%). Dietary advice was provided to 77 patients, only 6.48% of all patient appointments. Comparably, oral hygiene instruction was provided to almost 10 times as many patients (n = 754, 63.41%). The frequency of each of the treatments provided by third-year oral health students over the 12 months is listed in Table 2.
Statistical Correlations
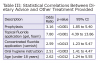
Logistic regression analysis was used to determine if statistically significant correlations existed between dietary advice and other treatment provided at the same appointment. There was a statistically significant link between dietary advice and oral hygiene instruction, with patients who received oral hygiene instruction being 2.5 times as likely to also receive dietary advice at that appointment (OR: 2.51, 95% CI 1.41 to 4.47, P < .003). Patients who received prophylaxis were also more likely to receive dietary advice than those who did not (OR: 3.16, 95% CI 1.85 to 5.40, P < .001). Topical fluoride application (gel) significantly increased the likelihood for a patient to receive dietary advice. Patients who received topical fluoride were 7.8 times as likely to receive dietary advice (OR: 7.80, 95% CI 4.39 to 13.86, P < .001). A correlation was also found between concentrated fluoride application (varnish) and dietary advice (OR: 2.59, 95% CI 1.23 to 5.47, P < .013); however, this correlation was not as strong. Alternatively, no statistically significant correlations were found between dietary advice and debridement or periodontal charting. Table 3 reports statistical correlations between dietary advice and other treatment provided.
Logistic regression analysis was also carried out to examine possible correlations between dietary advice and age or gender of patients. The data demonstrated patients under the age of 18 were more likely to receive dietary advice than adult patients. Patients less than 18 years old were more than 2.5 times as likely to receive dietary advice. No statistically significant correlations were discovered between dietary advice and gender.
Discussion
This study examined the frequency with which dietary advice was provided by dental hygiene students to patients seen over a 12-month period. The results demonstrated that dietary advice is provided infrequently by dental hygiene students. These results are consistent with the findings of McKinney et al, indicating that dietary advice may be overlooked by a wide range of dental professionals.18
The findings from the present study have demonstrated dietary advice was only provided to 6.48% of patients. These results are quite concerning and may indicate a need to review dental hygiene curricula. Comparably, 52% of dental hygienists in Oregon reported providing dietary advice in their practices; however, over half of those surveyed provide dietary advice to fewer than 10% of patients.10 The low proportion of patients receiving dietary advice could be attributed to barriers such as time constraints or limited training and/or practical experience in providing dietary advice.19 Given the results from the present study, it may be necessary for further research to be carried out to examine barriers to providing dietary advice. Future research may also be required to examine the content and application of dietary advice training for dental students.
A statistically significant correlation was observed between dietary advice and age, with children less than 18 years of age being 2.5 times as likely as older patients to receive dietary advice. These findings may be attributed to current policies and guidelines on appropriate feeding practices for children, indicating a view that children are in greater need of dietary advice than adults.20
A number of close associations were discovered between dietary advice and other treatment provided to patients. Patients who received oral hygiene instruction were 2.5 times as likely to also receive dietary advice, indicating that oral hygiene instruction is often provided in conjunction with dietary advice. The authors hypothesize that dental hygiene students may provide both dietary advice and oral hygiene instruction to patients they identify as high-caries-risk patients. Similarly, correlations were observed between topical and concentrated fluoride application (varnish) and dietary advice provision, again indicating a possibility that patients identified as being at a greater risk of developing caries are deemed to require dietary advice. Interestingly, provision of prophylaxis was also positively associated with dietary advice, with patients who received prophylaxis more than 3 times as likely to receive dietary advice during the same appointment. It may be that prophylaxis is provided more frequently to children, explaining the association with dietary advice. No correlations were present between dietary advice and debridement or periodontal charting.
Given that hygiene students see patients for lengthy appointments and are supervised and supported by clinical faculty, it was surprising that they were not providing dietary advice more regularly. It is important for dental professionals to recognize the importance of dietary advice, not only for its role in oral health, but also for prevention of diet-related systemic diseases such as diabetes and heart disease. Dental hygienists typically see patients quite frequently for somewhat long appointments, arguably making them ideally suited to counsel patients about the link between diet and disease.
Most studies examining the frequency of dietary advice provision obtain data from self-reporting of dental practitioners.10,21 One disadvantage of using self-reporting is that dental practitioners are essentially required to estimate their dietary advice practices, potentially causing the results to be affected by over-reporting. Therefore, it is likely that studies relying on self-reporting do not accurately reflect the true dietary advice practices of dental professionals. This study used data taken directly from clinical records, thus, having the potential to be much more accurate.
Diet-related oral health problems such as dental erosion and dental caries pose a significant challenge to oral healthcare professionals. Dietary advice appears to be a valuable strategy in influencing eating and drinking habits, in turn, having the potential to prevent or manage dental caries and erosion.22 Dental hygienists may be ideally suited to providing dietary advice to patients as part of their preventive role and, therefore, present an interesting area for research. Dental hygiene students offer a valuable insight into the practices of dental practitioners, and educators should consider whether students receive adequate training in dietary advice. These results suggest dietary advice may be overlooked or possibly undervalued as a component of the preventive oral care regime. Further research may be useful to investigate barriers to dietary advice provision, as well as the perceived importance of dietary advice to dental practitioners.
It is important to recognize limitations to the present study. The conditions for entering the item number 131 specify that at least 15 minutes of dietary advice are to be provided. It is possible that students may have provided dietary advice, which lasted less than 15 minutes and was, therefore, not recorded in the clinical records. This would influence the results of the study, potentially leading to underreporting of dietary advice. In future studies, it may be valuable to produce a “dummy” item number for dietary advice provision of less than 15 minutes. Further, information on the caries risk for each patient was not available when extracting the data; it would have been interesting to determine if correlations exist between caries risk and the provision of dietary advice. As the study sample consisted of dental hygiene students at one university in Australia, the findings may have limited generalizability. However, the study has provided useful data to help us understand the practices of dental hygiene students in NSW, Australia. Further research is required to examine the dietary advice practices of a wide range of dental practitioners. As the study used a retrospective design, the data was reliant on accurate record keeping. However, as the clinical records were recorded at the time of the appointment and students are required to enter the item numbers corresponding with treatments provided, the records appear to be accurate and reliable.
Conclusion
In summary, the findings from the present study have demonstrated that dental hygiene students in NSW, Australia, provide dietary advice very infrequently to patients. These results are important, as diet is a key risk factor for many oral diseases, yet it appears that dietary advice is an overlooked component of the preventive oral healthcare practices of dental hygiene students. The research also demonstrates that there is a relationship between patient age and students deciding whether or not to provide dietary advice to patients. These results strongly suggest the need for a review of dental curricula to ensure that dietary advice is a major component of the preventive services offered by dental hygienists. Recommendations for further research include identifying barriers to dietary advice provision, perceptions of dental practitioners and students in regard to dietary advice, and further research examining the frequency of dietary advice provision by dental practitioners in a range of different settings and its association with caries risk.
References
1. Moynihan P, Petersen PE. Diet, nutrition and the prevention of dental diseases. Public Health Nutr. 2004;7(1A):201-226.
2. Tinanoff N, Palmer CA. Dietary determinants of dental caries and dietary recommendations for preschool children. J Public Health Dent. 2000;60(3):197-206.
3. Bartlett D. Etiology and prevention of acid erosion. Compend Contin Educ Dent. 2009;30(9):616-620.
4. Mejia GC, Amarasena N, Ha DH, et al. Child dental health survey Australia 2007: 30-year trends in child oral health. Australian Institute of Health and Welfare. [Internet]. 2012 [cited 2016 February 5]. Available from: http://www.aihw.gov.au/publication-detail/?id=10737421875.
5. Kawashita Y, Kitamura M, Saito T. Early childhood caries. Int J Dent. 2011;725320:7.
6. Nunn JH, Gordon PH, Morris AJ, Walker A. Dental erosion – changing prevalence? A review of British national childrens’ surveys. Int J Paediatr Dent. 2003;13(2):98-105.
7. Wahlqvist ML. Food & nutrition: food and health systems in Australia and New Zealand. 3rd ed. Crows Nest, NSW: Allen & Unwin; 2011.
8. Boyd LD, Giblin L, Chadbourne D. Bidirectional relationship between diabetes mellitus and periodontal disease: State of the evidence. Can J Dent Hyg. 2012;46(2):93-102.
9. Watt RG, McGlone P, Kay EJ. Prevention. Part 2: dietary advice in the dental surgery. Br Dent J. 2003;195(1):27-31.
10. Levy TA, Raab CA. A study of the dietary counseling practices among Oregon dental hygienists. J Dent Hyg. 1993;67(2):93-100.
11. Kading CL, Wilder RS, Vann WF, Curran AE. Factors affecting North Carolina dental hygienists’ confidence in providing obesity education and counseling. J Dent Hyg. 2010;84(2):94-102.
12. Manski MC, Parker ME. Early childhood caries: knowledge, attitudes, and practice behaviors of Maryland dental hygienists. J Dent Hyg. 2010;84(4):190-195.
13. Seow WK. Biological mechanisms of early child- hood caries. Community Dent Oral Epidemiol. 1998;26(1 suppl):8-27.
14. Sarmadi R, Gahnberg L, Gabre PIA. Clinicians’ preventive strategies for children and adolescents identified as at high risk of developing caries. Int J Paediatr Dent. 2011;21(3):167-174.
15. Harris R, Gamboa A, Dailey Y, Ashcroft A. One-to-one dietary interventions undertaken in a dental setting to change dietary behaviour. Cochrane Database Syst Rev. 2012;3:CD006540.
16. Professional attributes and competencies of the newly qualified dental hygienist. Australian Dental Council [Internet]. 2011 [cited 2014 June]. Available from: http://www.adc.org.au/index.php?id=14
17. Bowling A, Ebrahim S. Handbook of Health Research Methods: Investigation, Measurement and Analysis. Open University Press. 2007.
18. McKinney L, Karp NV, Karp WB. Dentist practices and attitudes toward nutrition counseling. J Mass Dent Soc. 1996;44(4):10-13.
19. Franki J, Hayes MJ, Taylor JA. The provision of dietary advice by dental practitioners: a review of the literature. Community Dental Health. 2014;31:9-14.
20. American Academy on Pediatric Dentistry Clinical Affairs Committee, American Academy on Pediatric Dentistry Council on Clinical Affairs. Policy on dietary recommendations for infants, children, and adolescents. Pediatr Dent. 2008-2009;30(7 Suppl):47-48.
21. Källestål C, Wang NJ, Petersen PE, Arnadottir IB. Caries-preventive methods used for children and adolescents in Denmark, Iceland, Norway and Sweden. Comm Dent Oral Epid. 1999;27:144-151.
22. Thompson RL, Summerbell CD, Hooper L, et al. Relative efficacy of differential methods of dietary advice: a systematic review. Am J Clin Nutr. 2003;77(4):1052-1057.