You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The failure of the nation’s infrastructures to satisfy the oral health needs of isolated, underprivileged, or impaired populations is well-documented.1-7 In response to these needs, many state dental boards have organized volunteer systems and ratified practice act provisions that encourage dentists and dental hygienists to provide services to disadvantaged and underserved populations within their communities.6-17 Some licensing boards have relaxed or suspended direct supervision requirements allowing oral health professionals unencumbered access to needy populations.11-14 In other regions, state officials offer reduced- or no-cost volunteer licenses to dentists and dental hygienists willing to provide charitable care to underserved populations in qualified locations.8,11-13,16 A few states also provide liability insurance and legal protection for dental professionals when they volunteer.17
In select states, providing pro bono care or freely presenting oral health education to indigent or critical need populations through nonprofit agencies and organizations are options for satisfying the continuing education requirements necessary for oral health professionals to demonstrate continued professional competence.9,13,14,16,18,19 Under these circumstances, dentists and dental hygienists can apply their professional expertise while benefiting those in need. Cultural competence is enhanced when services are provided to diverse populations in nontraditional settings. In this sense, volunteering in a professional capacity closely parallels the outcomes of academic service learning.20
Of the states requiring continuing education as a condition to maintain a license to practice dental hygiene, 13 presently recognize specified volunteer activities as a suitable alternative to educational course work.9,10 Arizona, Delaware, Florida, Georgia, Idaho, Illinois, Minnesota, Nevada, Ohio, Oklahoma, Oregon, South Dakota, and West Virginia all afford dental hygienists the option of performing a specified number of volunteer hours per licensing cycle to satisfy between 1 and 10 hours of the requisite number of continuing education hours.9 To alleviate deficiencies in the existing healthcare system, it is important for state professional licensing boards to understand exactly how and to what extent authority can be used to successfully engage dental hygienists in community service activities. Despite extensive exploration of this subject area, the phenomenon of volunteerism has been understudied in populations comprised specifically of dental hygienists. There is limited understanding of the factors that contribute to the decision of dental hygienists to volunteer professional services to the disadvantaged and underserved. A solitary investigation designed to evaluate this population’s views of mandatory requirements for community service was conducted by Bhayat et al among South African oral hygienists.21 They concluded stringent mandates can engender negative attitudes toward humanitarian service, and ultimately be counterproductive to their intended purpose.21 Similar outcomes were reached by comparable investigations that were conducted among populations other than dental hygienists.21-26 Researchers have found community service mandates can engender negative attitudes toward humanitarian service and ultimately be counterproductive to the intended purpose.21-26 Legislation designed to effectively promote volunteerism must ensure “volunteers” have the individual freedom to decide when, where, and how long the service will continue.21-25
According to the Self-Determination Theory (SDT) of human motivation and behavior, the ideal environment for responsible behaviors, such as volunteering, to take root and flourish are those that ensure autonomy while allowing for the interaction of both intrinsic and extrinsic influences.26,27 In addition to addressing both intrinsic and extrinsic motivations, the constructs of SDT account for the role external forces and social contexts play in facilitating desirable and responsible behaviors such as volunteering.26-31
The basic premise of SDT is that human beings are naturally prone to intrinsic or autonomous motivation and self-regulation, which are the sources of personal creativity, accountability, well-being, and lasting change.30-32 Depending upon one’s unique response to various environmental factors, an individual’s motivational orientation may be controlled to various degrees by external forces.27 Deci and Ryan consider people dominated by extrinsic rewards, punishments, or the expectations of others to have controlled motivational orientations.33 Others feel ineffective, even helpless or are simply content to maintain the status quo.30-33 In terms of SDT, such individuals are motivated and have an impersonal motivational orientation.33 The instrument designed by Deci and Ryan to measure these subscales of personal motivation is the General Causality Orientations Scale (GCOS).30-33
If dental hygienists are predominantly motivated by intrinsic forces to provide pro bono services, it is possible that an occupational licensing provision intended to ignite and fuel volunteer activity among this population may actually extinguish existing intrinsic or internal motivations for prosocial behaviors.27 Conversely, for dental hygienists who respond to external incentives or who are amotivated, a state-authorized benefit may kindle personal desires to provide volunteer service.27
Volunteering is a complex prosocial phenomenon that defies simple classification. For the purposes of this research, volunteerism was defined as: dental hygienists choosing to provide educational or therapeutic methods to prevent or treat oral diseases and promote oral health “in recognition of a need, with an attitude of social responsibility and without concern for monetary profit, going beyond one’s basic obligations.”34,35
The individuals identified as being most likely to volunteer are middle-aged, female college graduates who earn above-average levels of income.36-38 As the demographic profile of a volunteer is compared to the group characteristics of dental hygienists, it is clear these oral health professionals possess both the personal assets and resources that enable them to volunteer.39 In an early investigation of prosocial practices conducted among graduates of the University of Iowa’s dental hygiene program, Hunter found 57% of this population rendered some type of volunteer service annually.40 Marsh’s 2011 exploration of volunteerism among licensed New York dental hygienists determined 57.4% of dental hygienists volunteered in a professional capacity at least annually.35 Based upon data for the year 2010, only 26.3% of the general population in the United States volunteers.41 According to the 2007 American Dental Hygienists’ Association survey, 45.2% of dental hygienists report involvement in some type of volunteer activity related to the profession.39 Although the volunteer rate is considerably higher than that of the overall population, almost half of the dental hygienists in this country do not volunteer.39
The implications of permitting dental hygienists to satisfy re-licensure requirements by performing donated oral health services have not been investigated. While crediting or “rewarding” oral health professionals with continuing education hours for the performance of prosocial acts seems to be an ideal strategy to sustain and improve the rate of volunteerism, there is no empirical support for this arrangement. This research compared the donations of time and professional expertise, perceptions of volunteerism, and motivational orientations of dental hygienists when they volunteer professional services in both the presence and absence of a practice act statute intended to incentivize volunteerism.
Methods and Materials
Upon approval from the Idaho State Human Subjects Committee, a quasi-experimental, non-equivalent control group design was used to test the null hypotheses of no differences in the dependent variables of volunteer hours performed, individual perceptions of volunteerism, and dominant motivational orientations among dental hygienists. The target population was 3,717 registered dental hygienists from two neighboring geographical locations, with very similar environmental, economic, and demographic characteristics. The major distinguishing feature was a difference in state regulation of continuing education requirements and volunteer hours.
Forty-eight states require continuing education as a condition for professional license renewal.10 Utah is one of 35 that does not currently recognize volunteer activities as an indication of continued competence.9 Alternatively, Idaho accepts volunteer service as a form of continuing education.9 Registered dental hygienists endorsed by the states of Utah and Idaho were also selected as the cohorts for this research because in a state-by-state comparison of volunteer rates, these two regions were ranked proportionally first and second highest in the nation.41
With the support of both state dental hygiene professional associations, information procured from the state licensing boards, e-mails, text messages, and postcards were sent to actively licensed dental hygienists in Utah and Idaho. These communications invited them to participate, presented the purpose of the study, and outlined procedures for accessing and completing an online survey. The software SurveyMonkey was used to document participant consent and collect the information required to address the research questions.
The online survey was comprised of a combination of numerical, close-ended questions and semantic differential rating scales. The survey features were designed to assess the population’s descriptive characteristics, volunteer behaviors, and perceptions of volunteering.
The content and face validity of these aspects were substantiated by specific literature citations.23,36,42-51 The SDT General Causality Orientations Scale (GCOS) was used to assess the strength of three distinct motivational orientations among the study population.33 Twelve items presented hypothetical sketches and provided three possible reactions to each situation described. The three subscales for each measure corresponded to an Autonomy, Controlled, or an Impersonal Motivational Orientation. The stability and reliability of the research instrument was evaluated using test-retest reliability and a coefficient of 0.83 was achieved. At the conclusion of the 5-week survey period, the data collected was exported from SurveyMonkey, quantified, and statistically tested with a significance level of 0.05.
Results
Four hundred and twenty-eight (11.5%) dental hygienists actively licensed by the states of Utah and Idaho responded to the survey. Of the total number of survey respondents, 316 participants provided usable study data.
The majority of respondents were female between the ages of 21 to 40 years with dependents. Two thirds of the study participants were licensed to practice in Utah while one third was licensed in Idaho. The plurality of respondents worked part-time, had between 1 to 9 years of professional practice experience, and had attained a baccalaureate or graduate degree. Almost two thirds of the respondents were not members of the American Dental Hygienists’ Association. Nearly half (45.2%) of the dental hygienists surveyed were uncertain if time spent volunteering professional services was an option for satisfying some of the continuing education hours required for professional licensure renewal.
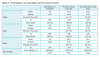
The inclinations of registered dental hygienists to volunteer in a professional capacity appear in Table 1. Although Utah dental hygienists seemed somewhat more willing to volunteer services to underserved populations when compared with Idaho dental hygienists, Mann-Whitney U analysis of this dimension revealed no statistically significant difference in the willingness of dental hygienists to volunteer.
Study participants were asked how many hours were typically spent providing pro bono oral health services each year. As evidenced in Table 1, dental hygienists in the state of Utah volunteered in a professional capacity a mean of 51.9 hours annually and in the state of Idaho 15.4 hours annually. Comparing the pro bono hours of professional dental hygiene service in the most recent 12-month period, the mean number for those licensed by the state of Utah was 20.4 hours. For those licensed by the state of Idaho the number was 17.8 hours. Mann-Whitney U tests were conducted on both measures of time spent volunteering in a professional capacity. The results revealed no statistically significant difference in the number of hours volunteered in a professional capacity when the practice occurred in a state where volunteer service is sanctioned by the dental licensing board as compared to when they practice in a state that does not permit some measure of volunteer service to satisfy re-licensure requirements.
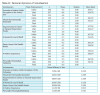
A summary of dental hygienists’ attitudes regarding the importance of volunteerism as well as the significance of certain personal, motivational, and situational antecedents of volunteer behaviors appear in Table 2. According to this table, dental hygienists in both states strongly affirmed the importance of volunteerism as a means of meeting unmet oral health needs or improving access to oral healthcare. Both Utah and Idaho dental hygienists categorically acknowledged the opportunity to serve within local communities was a personally meaningful, positive, intrinsically rewarding experience and promoted a positive public perception of the profession. Disagreement with extrinsically rewarding dental hygienists for prosocial efforts was a prevailing theme among all respondents. Utah dental hygienists indicated slightly stronger agreements for the statement: “Practice act requirements for the direct or general supervision of dental hygiene functions are a deterrent to dental hygienists volunteering in a professional capacity.” Mann-Whitney U analysis of the mean ranks of disagreement or agreement with statements relative to volunteerism revealed no statistically significant difference between dental hygienists licensed in the two states of interest.
The survey instrument asked dental hygienists to select the factor most likely to prevent volunteering professional services. Over 80% identified time constraints due to family, work, or school obligations as the main obstacle to involvement in volunteerism. The remaining respondents (18.9 %) indicated a lack of volunteer opportunities as the leading cause of non-participation in oral health service activities. Chi Square analysis of the nominal data collected revealed views of barriers to volunteerism were not significantly different between dental hygienists licensed by the states of Utah and Idaho.
Of the factors most likely to incite dental hygienists to participate in oral health service activities, 44.1% of respondents identified credit hours to satisfy state professional licensing requirements as the most motivating factor. State licensing endorsements were cross-tabulated with data identified motivating factors: a sense of personal satisfaction, opportunities for professional development, social networking opportunities, community approval or recognition, and credit hours to satisfy state professional licensing. Chi Square analysis of this nominal data revealed dental hygienists licensed by the states of Idaho and Utah did not have significantly different perceptions of the factors most likely to incite volunteer behaviors.
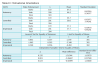
Study participants were asked to consider the reasons dental hygienists might volunteer in a professional capacity. As shown in Table 3, more dental hygienists in the state of Idaho as compared to the state of Utah felt the opportunities to learn something new and earn credit hours to satisfy licensing requirements were extremely important motives for providing pro bono services. Idaho dental hygienists also had higher rankings with regard to volunteerism being a societal obligation and a competency requirement, expectation, or option. Alternatively, more Utah dental hygienists viewed the opportunities to meet new people, enhance one’s resume, and find a meaningful use of discretionary time as extremely important reasons to volunteer. Mann-Whitney U analysis of the mean ranks of the importance of statements concerning the causes of volunteerism revealed there was no statistically significant difference between dental hygienists licensed in these two states.
The SDT GCOS was used to assess the strength of three distinct motivational orientations among the study population.33 Differences in the sample sizes for the comparisons occurred between the three subscales as not every study participant completed all survey items in this section.
Group statistics for the GCOS data set were calculated, and Table 4 provides the results of this statistical analysis. Although the measures of Autonomy, Controlled, and Impersonal Motivational Orientations were ordinal in nature, the overall scores of these subscales were the sum of 12, 7-point Likert scales. Therefore, the GCOS scores were treated as continuous variables, and a parametric independent samples t-test was used in the comparison of the mean GCOS scores of respondents.
Prior to conducting the independent samples t-test, to ensure the two variances on each subscale were equal, the data was subjected to Levene’s Test for Equality. In each instance, the resulting P value was greater than the critical value (0.05). Therefore, equal variances were assumed for all three GCOs subscales. The t statistic and degrees of freedom were also calculated for each subscale. Table 4 shows there was no statistically significant difference in the average GCOS scores for Autonomy and Impersonal subscale measures between dental hygienists endorsed by the states of interest. However, there was a statistically significant difference in the measure of Controlled Motivational Orientation. Dental hygienists licensed by the state of Utah scored higher on this dimension of motivation in comparison to dental hygienists licensed by the state of Idaho.
Discussion
The study participants presented a demographic profile very much like the descriptions of dental hygiene populations in the literature.21,35,39,40 Nonetheless, because this was a nonrandom sample survey, data cannot be generalized beyond the target population. In addition to sampling error, this study was impacted by the bias of nonresponse error. The 11.5% response rate was below average. The failure of participants to be actively licensed to practice dental hygiene in Idaho or Utah and to provide responses in each section of the survey further reduced the size of the study sample. Despite these inherent research biases, 316 subjects provided valuable data to enhance understandings of volunteerism.47-50 The results of this study were contrary to initial expectations of volunteer behaviors. Because dental hygienists licensed by the state of Idaho have the benefit of performing pro bono service in lieu of a portion of required continuing education hours, it was assumed they would perform a comparatively higher number of service hours. However, the dental hygienists of Utah volunteered more often, and many respondents from Idaho were unaware of volunteerism as a continuing education opportunity.
Nearly half (45.2%) of both the Utah and Idaho dental hygienists surveyed were uncertain if time spent volunteering professional services was an option for satisfying some of the continuing education hours required to renew the license to practice. This outcome suggests when dental hygienists are unaware or do not have a clear understanding of the details of state practice acts, amendments intended to encourage volunteerism may have little-to-no bearing on the actual number of volunteer hours performed.
Further explanation of the pattern of a nonsignificant difference is that practitioners licensed by the state of Idaho simply might not perceive the substitution of volunteer hours for continuing education hours to be a meaningful or personally beneficial incentive. Some comparative research has shown altruistic inclinations to volunteer or internal feelings of civic responsibility can be suppressed in the presence of extrinsic incentives or the external regulation of prosocial behaviors.21,23,25,43,51-53
The lack of no significant differences in dental hygienists’ perceptions of volunteerism were also unexpected. Both Utah and Idaho dental hygienists rated the opportunity to earn credit hours to satisfy professional licensing requirements as an important reason to volunteer. Nevertheless, there was consensus that pro bono hours performed as a requirement, expectation, or option to prove competency was neither an unimportant nor an important reason for volunteering.
Utah and Idaho dental hygienists strongly agreed volunteering was “a reward in and of itself” as well as a positive, personally meaningful, and satisfying experience. The majority disagreed with dental hygienists being extrinsically rewarded or compensated in any way for volunteer efforts. Yet, when asked which factor would most likely encourage volunteerism, 44.1% of Utah and Idaho dental hygienists selected “credit hours to satisfy state licensing requirements.” Only 29.6% chose the response option: “a sense of personal satisfaction.”
While these inconsistencies could be attributed to biases in the research, they support the literary findings. Although individuals may report altruistic feelings or intrinsic factors are the impetus for prosocial intentions and behaviors, a willingness to volunteer may also be influenced by egoistical feelings activated by extrinsic forces.26,42,51,52,54 SDT suggests a synergy between intrinsic and extrinsic factors must be encouraged if effective responsible human behavior is to be successfully stimulated.30 According to the results of this study, while dental hygienists strongly identified with intrinsic factors as the motivations of prosocial behaviors and disapproved of rewarding or compensating dental hygienists for acts of volunteerism, respondents demonstrated support of external incentives.
The results of the GCOS portion of the survey instrument revealed the dominant Motivational Orientation among dental hygienists in both Utah and Idaho was Autonomy. This result suggests dental hygienists in the two states of interest respond to “aspects of the environment that simulate intrinsic motivation, tend to display greater self-initiation, seek activities that are interesting and challenging and take greater responsibility for his or her own behavior.”33 Therefore, simply increasing awareness of oral health needs and how practitioners can meet the needs may be enough to encourage volunteerism in this population.
The only statistically significant difference between the two groups examined were scores on the GCOS subscale of Controlled Motivational Orientation. Dental hygienists licensed by the state of Utah scored higher on this dimension of motivation when compared with dental hygienists licensed in Idaho. This result may reflect differences in supervision requirements between the two states. In this exploration of volunteerism, more than 60% of the survey respondents agreed or strongly agreed that practice act requirements for the direct or general supervision of professional functions were a deterrent to dental hygienists volunteering in a professional capacity. In addition to requirements for ongoing education and training, another dental practice act provision of particular consequence to the volunteering practices of dental hygienists are state directives related to practice supervision.55,56 Utah is a state where dental hygienists practice under general supervision requirements.57 Oral hygiene services are permitted only when patients have been examined and treatment is prescribed by a licensed dentist.57 When encumbered by direct or general supervision requirements, dental hygienists must rely on the good will of dentists to support efforts to provide pro bono care. Direct and general supervision requirements may also create restrictions as to when, how, and where dental hygienists provide community service.6,11-16
Alternatively, practice acts stipulating direct access are much more conducive to dental hygienists volunteering professional services.55,56 Presently, over half of the states in the nation, including the state of Idaho, permit dental hygienists direct access to some degree.55,56,58 Direct access provisions allow dental hygienists to “initiate treatment based on his or her assessment of patient’s needs without the specific authorization of a dentist, treat the patient without the presence of a dentist, and...maintain a provider-patient relationship.”56
According to SDT, general supervision constraints would frustrate a dental hygienist’s need for autonomy.28,32 Such practice provisions orient dental hygienists to external control of behaviors, which could intrude on intrinsic motivations to provide community service.21,23,25,43,51-53 Because such practice provisions discourage rather than encourage self-determination, dental hygienists subject to this influence may feel there are fewer opportunities to volunteer. Ultimately practitioners may become less involved in volunteering in a professional capacity. Conversely, direct-access regulations are social factors with the potential to increase dental hygienists’ intrinsic motivations for volunteerism.
Conclusion
The lack of significant difference in the number of volunteer hours between licensed hygienists in Utah and Idaho should not be construed to mean legislation related to the substitution of pro bono hours for continuing education hours fails to affect the volunteer practices of dental hygienists. Additional research is required to make realistic determinations as to the effectiveness of such legislation. This investigation contributes to the body of knowledge regarding volunteerism in society and accentuates the need for additional explorations of the extent to which practice act regulations encourage or discourage dental hygienists’ altruistic decisions and actions.
Legislators and members of professional licensing boards should consider dominant motivational orientations of dental hygienists as they compose and ratify policies intended to mobilize this population to provide charitable oral health assessments, care, and education. To address the current oral healthcare crisis in this country, dental hygienists are in need of evidence-based practice statutes and regulations that keep pace with the objective of universal access to comprehensive oral care.
About the Authors
Sandra D. Wilkie, RDH, MS, is a dental hygienist at Roseman University of Health Sciences, College of Dental Medicine. JoAnn R. Gurenlian, RDH, MS, PhD, is a professor and graduate program director in the Department of Dental Hygiene at Idaho State University. Jacqueline J. Freudenthal, RDH, MHE, is an associate professor, Department of Dental Hygiene, Idaho State University.
Acknowledgments
We gratefully acknowledge the Idaho and Utah Dental Hygienists’ Associations, Idaho State University graduate students, staff, and faculty members, who provided invaluable support and assistance with this research. In particular, we recognize the vital contributions of statistician Dr. Teri S. Peterson and graduate faculty representative, Dr. Chris Sanford. We also express our sincere appreciation to the registered dental hygienists who participated in this research.
References
1. Health, United States, 2011. Hyattsville, MD: National Center for Health Statistics; 2010.
2. The meaning of oral health. In: Oral Health in America: A Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health, 2000.
3. National Call to Action to Promote Oral Health. Rockville, MD: US Department of Health and Human Services, Public Health Service, National Institute of Dental and Craniofacial Research, National Institutes of Health, 2003.
4. 2020 Topics & objectives. Oral health. Overview. US Department of Health and Human Services. 2012.
5. Oral health. Preventing cavities, gum disease, tooth loss, and oral cancers at a glance 2011. Chronic Disease Prevention and Health Promotion. Centers for Disease Control and Prevention; 2011.
6. Access to Care. Office of Student Affairs. American Dental Association [Internet]. 2010 [cited 2012 November 2]. http://www.ada.org/section/educationAndCareers/pdfs/access_to_care_infopak-2010.pdf.
7. Dental hygiene. Focus on advancing the profession. American Dental Hygienists’ Association [Internet]. 2005 [cited 2012 November 2]. http://www.adha.org/downloads/ADHA_Focus_Report.pdf.
8. Gehshan S, Snyder A. Why public policy matters in improving access to dental care. Dent Clin North Am. 2009;53(3):573-589.
9. States Requiring Continuing Education for License Renewal. American Dental Hygienists’ Association [Internet]. 2009 [cited 2013 October 24]. http://www.adha.org/resources-docs/7512_CE_Requirements_by_State.pdf.
10. Facts About the Dental Hygiene Workforce in the United States. American Dental Hygienists’ Association [Internet]. 2012 [cited 2013 October 24]. http://www.adha.org/resources-docs/75118_Facts_About_the_Dental_Hygiene_ Workforce.pdf
11. American Dental Hygienists’ Association. Stateline. Access. 2012;26(5):10.
12. American Dental Hygienists’ Association. Stateline. Access. 2012;26(4):10-15.
13. American Dental Hygienists’ Association. Stateline. Access. 2005;19(8):37-38.
14. American Dental Hygienists’ Association. Stateline. Access. 2008;22(6):14-15.
15. American Dental Hygienists’ Association. Stateline. Access. 2003;17(3):40.
16. American Dental Hygienists’ Association. Stateline. Access. 2009;23(6):27.
17. Geletko KW, Beitsch LM, Lundberg M, Brooks RG. Reducing the impact of the health care access crisis through volunteerism: a means, not an end. Am J Public Health. 2009;99(7):1166-1169.
18. Law and rules. Ohio State Dental Board [Internet]. 2011 [cited 2013 January 9] http://www.dental.ohio.gov/pdfs/2011dpa.pdf.
19. Other continuing education guidelines. Clinical volunteer services. Continuing education. South Dakota State Board of Dentistry [Internet]. 2010 [cited 2013 January 9] https://www.sdboardofdentistry.com/licensure/continuingEducation.asp.
20. Lautar CJ, Miller FY. Service-learning and dental hygiene: a literature review. J Dent Hyg. 2007;81(3):1-10.
21. Bhayat A, Yengopal V, Rudolph MJ, et al. Attitudes of South African oral hygienists towards compulsory community service. Int J Dent Hyg. 2008;6:8-12.
22. Metz E, Youniss J. A demonstration that school-based required service does not deter but heightens volunteerism. Pol Sci Politics. 2003;36:281-286.
23. Planty M, Bozik R, Regnier B. Helping because you have to or helping because you want to? Sustaining participation in service work from adolescence through young adulthood. Youth Soc. 2006;38(2):177-202.
24. Sobus MS. Mandating community service: psychological implications of requiring prosocial behavior. Law Psych Rev. 1995;153:1-19.
25. Stukas AA, Snyder M, Clary EG. The effects of “mandatory volunteerism” on intentions to volunteer. Psych Sci. 1999;10(59):59-64.
26. Shye S. The motivation to volunteer. A systemic quality of life theory. Soc Indic Res. 2010;98(2):183-200.
27. Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68-78.
28. Deci EL, Ryan RM. Intrinsic motivation and self-determination in human behavior. New York, NY: Plenum Press; 1985.
29. Deci EL, Ryan RM. Motivation, personality, and development within embedded social contexts: an overview of self-determination theory. In: Ryan RM, ed. The Oxford Handbook of Human Motivation. Oxford, United Kingdom: Oxford University Press; 2014:85-107.
30. Deci EL, Ryan RM. Self-determination theory: a macrotheory of human motivation, development, and health. Can Psych. 2008;49(3):182-185.
31. Deci EL, Flaste R. Why We Do What We Do: The Dynamics of Personal Autonomy. New York, NY: GP Putnam’s Sons; 1995.
32. Deci EL, Ryan RM. The general causality orientations scale: self-determination in personality. J Res Pers. 1985;19:109-134.
33. University of Rochester. Self-determination theory. An approach to human motivation and personality. Questionnaires. The General Causality Orientations Scale. GCOS [Internet]. 2012 [cited 2012 November 2]. Available from: http://selfdeterminationtheory.org/questionnaires/10-questionnaires/46.
34. Ellis SJ, Noyes KH. By the people, a history of Americans as volunteers. San Francisco, CA: Jossey-Bass Publishers; 1990:4.
35. Marsh LA. Dental hygienist attitudes toward willing- ness to volunteer care for the underserved population (Doctoral dissertation). Available from: ProQuest dissertations and theses database. 2011. (UMI No. 3451011).
36. Bussell H, Forbes D. Understanding the volunteer market: the what, where, who and why of volunteering. Int J Nonprof Voluntary Sec Market. 2002;7(3):244-57.
37. Brown E. The scope of volunteer activity and public service. Law Contemp Probl. 1999;62(4):17-42.
38. Volunteering in the United States-2011. U.S. Department of Labor Bureau of Labor Statistics. 2012.
39. Survey of dental hygienists in the United States. Executive summary. American Dental Hygienists’ Association [Internet]. 2007 [cited 2012 November 2]. Available from: https://www.adha.org/resources-docs/7117_ADHA_Environmental_Scan.pdf.
40. Hunter EL. Volunteerism of dental hygienists. Dent Hyg. 1978;52:535-540.
41. Volunteering in America. Corporation for National Community Service [Internet]. 2012 [cited 2012 November 2]. Available from: http://www.volunteeringinamerica.gov/rankings.cfm
42. Finkelstein MA. Intrinsic vs. extrinsic motivational orientations and the volunteer process. Pers Individ Dif. 2009;46:653-658.
43. Goette L, Stutzer A, Frey, BM. Prosocial motivation and blood donations: A survey of the empirical literature. Transfus Med Hemother. 2010;37(3):149-154.
44. Lacetera N, Macis M, Slonim R. Will there be blood? Incentives and substitution effects in prosocial behavior. Economics Working Paper Series. 2010;1-49.
45. Sundeen RA, Raskoff S, Garcia MC. Differences in perceived barriers to volunteering to formal organizations: lack of time versus lack of interest. Non-profit Manag Leadersh. 2007;17(3):279-300.
46. Brown E. The scope of volunteer activity and public service. Law Contemp Probl. 1999;62(4):17-42.
47. Esmond J, Dunlop P. Developing the volunteer motivation inventory to assess the underlying motivational drives of volunteers in Western Australia. CLAN WA Inc. [Internet]. 2004 [cited 2012 November 2]. Available from: http://biggestdifference.com/mor- evolunteers/resources/MotivationFinalReport.pdf.
48. Clary EG, Snyder M. The motivations to volunteer: theoretical and practical considerations. Curr Dir Psychol Sci. 1999;8(5):156-159.
49. Mowen JC, Sujan H. Volunteer Behavior: A hierarchal model approach for investigating its trait and functional motive antecedents. J Consum Psychol. 2005;15(2):170-182.
50. Hall MH. Measurement issues in surveys of giving and volunteering and strategies applied in the design of Canada’s national survey of giving, volunteering, and participating. NVSQ. 2001;30(3):515- 526.
51. Ariely D, Bracha A, Meier S. Doing good or doing well? Image motivation and monetary incentives in behaving prosocially. Am Econ Rev. 2009;99(1):1-17.
52. Frey BS, Oberholzer-Gee F. The cost of price incentives: an empirical analysis of motivation crowding-out. Am Econ Rev. 1997;87(4):746-755.
53. Frey BS, Goette L. Does pay motivate volunteers? Institute for Empirical Research in Economics, University of Zurich, Working Paper Series ISSN 1424-0459 [Internet]. 1999 [cited 2012 November 2]. Available from: http://fex-dev2.ethz.ch/eserv/eth:25512/eth-25512-01.pdf.
54. Mannino C, Snyder M, Omoto A. Why do people get involved? Motivations for volunteerism and other forms of action. In: Dunning D, ed. Social Motivation. New York, NY: Taylor & Francis Publishing; 2011:127-146.
55. Dental hygiene practice act overview: Permitted functions and supervision levels by state. American Dental Hygienists’ Association [Internet]. 2013 [cited 2013 October 24] Available from: http://www.adha.org/resourcesdocs/7511_Permitted_Services_Supervision_Levels_by_State.pdf.
56. Direct access states. American Dental Hygienists’ Association [Internet]. 2013 [cited 2013 October 24]. Available from: http://www.adha.org/resourcedocs/7513_Direct_Access_to_Care_from_DH.pdf.
57. American Dentists and dental hygienist practice act. Division of Occupational and Professional Licensing. Utah.gov [Internet]. 2012 [cited 2013 January 4]. Available from: https://secure.utah.gov/datarequest/professionals/requestExemption.html.
58. Administrative rules. Statues and administrative rules. Idaho State Board of Dentistry [Internet]. [cited 2013 January 4]. Available from: http://isbd.idaho.gov/rules.htm.