You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Introduction
Thirteen percent of the US population is considered older, or over the age of 65, with increases expected to reach 20% by 2030, or 92 million Americans.1,2 Data from the most recent 2010 census revealed that the older population is increasing 15% more than the overall US population.3 Currently, about 4% of older Americans reside in long-term care facilities (LTCFs); in 2007 alone, there were 15,827 LTCFs providing 24-hour care by nurses and other staff members to oversee and monitor healthcare needs.4 It is estimated that 63% of the total number of patients residing in LTCFs are older, and by 2040, 20% of older Americans will require long-term care.5-7
Several limitations exist within LTCFs related to oral hygiene, since many long-term older patients (LTOPs) are medically compromised and are unable to provide oral hygiene self-care.8 Older adults retain 26 or more teeth throughout their lifetime, typically losing six teeth or less; only one fourth of the older population is fully edentulous.6,7 Literature confirms that the high incidence of certain systemic conditions in the LTOPs may be linked with poor oral hygiene, which include: diabetes, cardiovascular diseases, nursing home aspiration pneumonia, and physical/mental disorders.9-12 As LTOPs increase, oral healthcare for this disparaged population must become a priority with registered dental hygienists (RDHs) playing a larger role in the acquisition of care. There is a great need for LTCFs to employ RDHs to provide preventive and therapeutic oral care to these patients with the intent of reducing both oral health disease and systemic health conditions. The purpose of this manuscript is to identify systemic health conditions, oral health conditions, and barriers to oral care within LTOPs and to offer recommendations for increased access to care within LTCFs through utilization of RDHs.
Systemic Health Concerns
Type I and Type II diabetes affects approximately 25% of LTOPs, and researchers predict the greatest increase will occur in the 75 and older age group over the next 40 years.13,14 Concern for the LTOP with diabetes exists due to age-related complications that affect treatment and comorbidities such as polypharmacy, renal insufficiency, increased fall risk, visual impairment, and cognitive impairment.14 Unique guidelines have been established for treating LTOPs with diabetes based on life expectancy, cognition, and medication regimens for dental professionals.13 Medications are a difficult treatment option as they cannot always be prescribed to the LTOP due to compromised metabolism and risk of multiple drug interactions.13 A recent report stated that diabetics were 28% more likely to become fully or partially edentulous; 1 in every 5 cases of edentulism is linked to diabetes.15 Poor glycemic control in those with diabetes also places LTOPs at risk due to the well-established direct relationship between blood glucose levels and periodontal disease.15 Investigators have reported that inflammation resulting from periodontal disease exacerbates chronic systemic inflammation to influence the initiation and progression of diabetes, typically Type II diabetes.9,11 Increased inflammation, or more severe uncontrolled periodontal disease, is correlated with insulin resistance and more complications.9,11 In addition, diabetes places the LTOP at a higher risk for oral Candida infections due to the high blood sugar levels promoting the growth of the Candida albicans.9 Longitudinal studies on patients with diabetes and periodontal disease show those with better controlled glycemic indices had less severe inflammatory responses with their periodontal disease; thus, the diseases reflect one another.9
Cardiovascular disease (CVD), including hypertension, heart failure, coronary heart disease, arrhythmias, peripheral vascular disease, and valvular heart disease, affects 38.2% of older adults.16,17 CVD has been reported to be the number one cause of death in the older population.15 Forty percent of deaths from CVD occur between the ages of 75 and 85, while 48% occur over age 85.17 A study by Persson et al evaluated periodontal status by measuring bone loss on the radiograph, vertical defects, and furcations localized to the molars; radiographic evidence of periodontitis was found in 48.5% of the subjects, and carotid calcification was detected in 18.6%.18 Age was determined a primary risk factor for CVD due to increased carotid calcifications detected from panoramic radiographs.18,19 A systemic review by Lam et al reported that patients presenting with periodontal disease were 1.14 to 2.2 times more likely to develop CVD.10 Researchers are not in agreement that a correlation between periodontal disease and CVD is associated with systemic inflammation expressed in serum markers: interleukin-6, white blood cell counts, and fibrinogen.10 LTOPs that have endothelial dysfunction and carotid intima media thickness are also at increased risk for CVD and periodontal disease. This is because chronic microorganisms such as Chlamydophila pneumonia are said to cause atherosclerosis, and the DNA of oral bacteria can be amplified directly from atherosclerotic plaques.10,11 Providing care to the LTOP with CVD can be challenging since medications are often not realistic due to polypharmacy, and surgery is often contraindicated.17 When medications are used to treat CVD, they often have a damaging effect on the oral cavity including: xerostomia, gingival hyperplasia, and ulcerations.10 Due to the correlation between CVD, age, and periodontal disease, it is imperative that LTOPs receive routine preventive and therapeutic oral health services to include evaluation of the gingival pocket depths and alveolar bone loss.18
Nursing home aspiration pneumonia (NHAP) is common in the LTOP with existing breathing difficulties, and is defined as pneumonia developing after the collection of colonized oropharyngeal organisms in the lower right lung lobe of the LTOP.12-22 Streptococcus aureus and Pseudomonas aeruginosa are the main microbes contributing to NHAP.20,21,23-25 One of the highest mortality rates for the LTOP is associated with NHAP due to excess gram negative aerobic rods and Staphylococcus aureus collecting in the oral cavity.11,12 LTOPs breathe them into their lungs and contract the disease.11,12 Evidence shows risk factors that make the LTOP more prone to NHAP as poor functional status, presence of a nasogastric tube (NG), dysphagia, occurrence of an unusual event, chronic lung disease, presence of a tracheostomy, increasing age, and male gender.12 When diagnosed, the disease is often in an advanced stage, with few treatment options available.20,21,25 NHAP should not be mistaken for other types of pneumonias also commonly found among the geriatric. Aspiration pneumonitis is an acute lung injury after inhalation of regurgitated gastric contents, typically while unconscious.12 In addition, nosocomial pneumonia occurs more than 48 hours after hospital admission, but was not present at admission to the hospital.12 Hospital-acquired pneumonia first appears 3 days after a patient is admitted to the hospital.12 Finally, ventilator-associated pneumonia is defined as pneumonia that occurs after 48 to 72 hours of endotracheal intubation due to dysphagia.12 While NHAP can be treated with antibiotics, the optimum antibiotic regimen for NHAP is unknown.12 Since oral biofilm can collect and enter the lungs by gliding down the track of the NG tube, the LTOP on a NG tube is at a higher risk for developing NHAP.12 Typically, 35% of LTOPs in a LTCF will require a NG tube; often a NG tube is necessary due to dysphagia, or difficulty swallowing.12
Sarin et al examined 613 LTOPs, with an average age of 84, to determine direct links between NHAP and nine common risk factors.21 The risk factors were inadequate oral care, difficulty swallowing, lack of influenza vaccination, depression, feeding position of less than 90° from horizontal, active smoking, recipient of sedative medication, recipient of gastric-acid reducing medication, and use of angiotensin-converting enzyme inhibitors.21 Results indicated that only two risk factors associated with developing NHAP were identified: difficulty swallowing and inadequate oral care.21 A similar study investigated how preventative oral hygiene treatment could reduce the chance of developing NHAP in the LTGP.20 In a meta-analysis conducted by Sjogren and colleagues, published literature related to oral hygiene, NHAP, and the LTOP was reviewed.20 Fifteen articles were calculated to include an absolute risk reduction, numbers needed to treat, and positively correlated professional oral hygiene care with reduced cases of NHAP in the LTGP.20 Results demonstrated that after participants were provided with routine oral care, absolute risk reduction increased from 6.6% to 11.7%, and numbers needed to treat increased from 8.6 to 15.3 individuals.20
Adachi et al evaluated the effect of professional oral care delivery on respiratory disease of LTOPs in edentulous and dentate populations to determine if professional oral hygiene therapy administered by RDHs reduced NHAP.25 The experimental group consisted of 48 LTOPs who received daily brushing from an RDH using a toothbrush and fluoridated toothpaste, while the control group of 40 LTOPs received daily brushing with water and foam swabs by a certified nursing assistant (CNA) for a 6-month period.25 Results concluded those patients receiving daily oral healthcare from a CNA using a foam swab had higher incidences of Staphylococcus species, Pseudomonas aeruginosa and Candida albicans than the experimental patients who were provided oral care by RDHs.25 The chance of developing NHAP was lower in the experimental group (P < .05).25 Systematic reviews and experimental studies all conclude that professional daily oral hygiene and a reduced bacterial count in the LTOP will ultimately decrease the chance of NHAP.12,20-23
Oral Health Concerns
Oral hygiene is imperative in LTCFs, because natural teeth are more susceptible to dental caries, periodontal disease, demineralization, and gingival recession due to age, diet, genetic factors, brushing habits, and lifestyle factors over time.8,13-18,26-32 More than half of older adult patients have enamel and root surface caries, placing them at the highest risk due to gingival recession, heavy consumption of fermentable carbohydrates, poor oral hygiene, and decreased fluoride exposure.32,33 More recurrent caries is evident along the coronal surfaces from marginal breakdown or other failing restorative materials; fermentable carbohydrates can also collect around crowns, bridges, and implants, leading to carious lesions.34
Investigators have reported that periodontal disease occurs at a rapid pace for the LTOPs, often worsening with age.2,34-37 Twenty-three percent of the total older population has severe periodontal disease, with symptoms of inflamed, painful gingival tissue, recession and mobility.38 Periodontal disease in the LTOP is a result of several factors including: chronic diseases and disabilities, race, gender, medications, income, and access to oral care prior to admittance.38,39
LTOPs with removable prosthetics are at an increased risk of oral diseases and lesions, including oral candidiasis and denture stomatitis resulting from Candida albicans.37,40,41 A cross-sectional study, with an average age of 85, aimed to investigate fungal infections on 233 denture-wearing LTOPs.41 Swabs were performed on the participants’ buccal mucosa to determine the micro floral status.41 Results demonstrated that oral candidiasis and higher oral yeast counts are commonly seen in the LTOP and are attributed to lack of daily denture cleaning.41
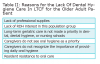
The LTOP is more susceptible to salivary changes and oral lesions because of a decrease in salivary gland function.32,42 Reports suggest that 15% to 30% of LTOPs experience xerostomia, most likely due to an average of eight daily prescribed medications (Table 1).32,42 Research points to increased xerostomia leading to higher caries rates in the LTOP.32 Xerostomia also gives way to dysphagia due to an adequate amount of salivary flow needed to help push the food towards the trachea.43
Between 15% to 60% of LTOPs may present with a nutritional deficiency due to medication side effects or an overall reduction in appetite.44,45 Loose dentures or decayed, broken, and missing teeth can cause difficulty consuming nutritious food.44,45 Several studies reported LTOPs with broken, missing, and severely decayed teeth had a chief complaint of inability to masticate; the studies also found LTOPs to have poor-fitting dentures.45 In addition, 6 million older patients are at risk for dysphagia.43 Dysphagia occurs often with increasing age due to the natural deterioration of the muscle mass and connective tissue elasticity, resulting in loss of strength and range of motion.43 As a result, many LTOPs have dysphagia and often become malnourished due to the limited choices of food to provide nutrients.43
Physical disabilities from falls, deterioration of the body with age, arthritis, stroke, spinal cord injuries, and blindness all affect oral hygiene capabilities.23,30,31 Common cognitive disabilities in the LTOP such as dementia, stroke, and Alzheimer’s disease make preventive oral care even more difficult.23,30,31 Descriptive studies where RDHs examined oral hygiene and oral health status confirms LTOPs with both mental and physical disabilities were often unable to care for the oral cavity without assistance.23,30,31,40 Furthermore, it has been established that those LTOPs in severe stages of physical and mental disabilities had the worst oral hygiene; as the systemic disease progressed their oral health deteriorated.23,30,31,40
Barriers to Oral Care
The Omnibus Budget Reconciliation Act of 1987 (OBRA) addressed many concerns regarding care in LTCFs by establishing new standards better focused towards the LTOP’s quality of life. OBRA was also praised for establishing Minimum Data Sets (MDS) to be completed on all LTCFs requiring Medicare and Medicaid reimbursement.15,23 LTCFs are reimbursed by Medicaid and because Medicaid is an entitlement program, LTCFs must provide the specialized oral care to anyone eligible according to the Federal government.47 LTCFs must provide routine dental services and emergency dental services to the extent which they are covered under the state, according to Medicaid.47 Dental bills that are not fully paid with Medicare may also be covered under an incurred medical expense, so that the LTCF can be reimbursed.48 In as many as 15 states, Medicaid will directly reimburse RDHs providing care to the LTOP.49
Nurses are required to complete sections K and L of the MDS that pertain directly to oral health.42 These sections are supposed to trigger intervention, care planning, and improvements in oral health.42 Still, there are numerous concerns about the quality of oral care received, since payroll for nurses tends to account for the biggest overhead and funds are limited.7 Limitations and restraints are also seen as few oral hygiene or health concerns are identified; the MDS simply records what services were completed and cannot effectively enforce suitable care to every patient.42 It has been shown that nurses can be dishonest about daily routines that have been carried out with the patient, including oral care.24 Furthermore, MDS scores are taken into account for an LTCFs overall evaluation, and poor marks could jeopardize the facility’s funding agencies and regulation records.24 Because oral hygiene marks on the MDS score are not considered vital to the scoring process, an incomplete record of care often occurs.24
Multiple interviews with nursing staff have given the most insight as to why care of the oral cavity is not given more emphasis in LTCFs (Table 2).27,28,42,50 Many nurses found that oral hygiene was minimally covered in their education; only 1% to 3% of the nursing workforce is trained in older adult oral care.27,28,42,50 The small amount of time spent learning about oral care for the LTOP made it seem less interesting and unimportant, with less than 30 minutes devoted to older adult care in nursing curricula, and even less time is spent in the CNA curricula.51 Also, nursing staff reported oral care as a challenge for fear of being bitten or forcing care upon the patient, especially those with mental impairments.26-28 Some CNAs found caring for the oral cavity to be filthy, unnecessary, and unimportant, particularly when cleaning dentures or partials.5,28 CNAs that deemed oral hygiene an important part of the daily routine received little support from other healthcare staff at the LTCF.5,24,28 LTCFs are becoming overcrowded—adding oral hygiene care in conjunction with other needs can be difficult and overwhelming for the nursing staff.7,23,24,29,52 When providing an adequate number of staff and allowing a moderate amount of time to complete the oral care routine, nurses not only found oral hygiene easier to perform, but also felt more responsible for providing these services to their patients.27,53-55 Interprofessional collaboration between RDHs and nurses of all skill levels needs to be established. Forming a better relationship between health disciplines would allow the RDH to provide the LTCF nursing staff more assistance when it comes to treating the oral cavity of the LTOP. There are several gaps in the importance and recognition of proper care and the relationships between oral health and systemic health that an RDH could address.56
Inadequate funding can also greatly impact oral care for the LTOP. Nursing staff have reported they often cannot care for their patient’s oral cavity due to inadequate supplies.27,28,42 More often than not, the nursing staff is provided water instead of a fluoridated toothpaste, and foam swabs instead of a toothbrush, although it has been shown that LTOPs do not receive enough fluoride uptake and that foam swabs cannot effectively remove plaque.57 An investigational study identified 41 LTOPs who had reductions in gingival bleeding and plaque scores over 3 weeks after receiving oral hygiene aids, while the nursing staff received oral health education from an RDH.28 The education for the nursing staff consisted of hands-on training in toothbrushing techniques when using an electric toothbrush and chlorhexidine gluconate 1% gel.28
LTOPs have the right to refuse professional oral hygiene care (Table 3).24,27,28,58 Questionnaires to nurses working in LTCFs revealed that often nurses felt confused and frustrated on proper protocol. The nurses had to make a choice: allow the LTOP to refuse necessary treatment or force dental care upon a resistant LTOP.58 Research has argued that LTOPs may be reluctant to seek out dental care due to financial restraints as many do not have dental insurance and have limited personal funds.2,36,59,60 Other research describes some LTOPs not recognizing the severity of their self-care deficit and refusing to have help provided to them for the oral cavity.56 As many as 83% of LTOPs have health concerns such as sensory problems and intubation tubes, which limit their ability to keep their oral cavity healthy.56
RDHs face multiple barriers when it comes to providing increased access to care for the LTOP. Few states are improving the need to provide better access to care for the LTOP. Only 45% of US states and territories have legislative policies working to provide increased access to the LTOP.61 Currently, governing legislation allows a RDH to practice in an LTCF without direct supervision from a dentist in some states; however, what services are provided and requirements of the RDH vary (Table 4).62 However, RDHs receive limited specialized education toward working with the LTOP.63-66 Dental hygiene curricula vary by school programs, and often, students report not receiving enough education in treating the LTOP.63,64 Most instructive lessons and clinical education for dental hygiene students are focused on caring for the relatively healthy, mobile older adult patient; very few courses offer support focused on the LTOP.65 None of the over 500 residencies established by the American Dental Education Association (ADEA) specialized in older adult training.2 The Commission on Dental Accreditation (CODA) requires dental hygiene students to work with the older adult population and community-based programs; however, it is not mandated that they work in LTCFs.66 Adapting school curriculum is challenging due to limited program funding that must be shared among multiple subject matters and topics; however, faculty within dental hygiene schools need to demonstrate increased interest in regard to oral care for the LTOP.66
Recently, the advanced dental hygiene practitioner was established in some states, allowing RDHs to provide access to care, because this model includes a broader range of duties that can be performed.67 Furthermore, research shows that RDHs are more likely to volunteer based on their level of education, job satisfaction, membership in their professional organization, and sensitivity to underserved patients.63 Until more direct access becomes available nationwide, many RDHs who are willing to work with the LTOP cannot do so, despite the huge need.
Discussion
With the first of the baby-boomers turning age 65 recently, literature has begun to focus on what changes will be needed to accommodate this very large segment of the American population.1-3 Several academic journals all recognize that LTOPs are at an increased risk from the lack of dental care provided when admitted into a LTCF.8,13-18,27-32 Systemic health conditions commonly found in LTOPs include natural deterioration, slowing of the human body, and various medications all cause an increased need for oral care in LTOPs (Table 1).32,42 Unfortunately, the LTOP themselves often do not recognize the importance of routine oral care and may refuse treatment for various reasons (Table 3).24,27,28,58 Despite healthcare providers attending to the LTOPs needs in a LTCF, literature has shown a void in collaboration between providers that could help reduce the lack of routine oral care.56,67 Attention needs to be brought to this matter in hopes that LTCFs could receive adequate funding to purchase oral hygiene aids, increase staffing, and educate the staff, LTOPs, and family members on the importance of routine oral care (Table 2).27,28,42,50 RDHs could potentially save lives by providing routine oral prophylaxis to the LTOP; thus, reducing heavy levels of bacteria in the oral cavity. Based on what has been conferred about the lack of dental hygiene care and its relationship to the LTOP, the authors believe that the RDH could provide increased access to care for LTOPs in LTCFs by doing the following:
1. Provide professional oral care to screen for carious lesions, fungal infections, oral lesions, periodontal disease, and assess salivary function.8,13-18,27-32
2. Perform preventive measures to decrease the incidence of carious lesions in the LTOP, through fluoride applications (varnish) and dental sealants.
3. Perform non-surgical periodontal therapy. Treat an unresponsive periodontal pocket with the administration of localized antimicrobials.
4. Provide education on topics such as nutritional counseling and side effects to commonly prescribed medications to the LTOP. A LTOP can have their nutritional status evaluated with a Mini Nutritional Assessment (MNA), a subjective assessment of health and nutrition from a questionnaire pertaining to diet.22
5. Assess, incorporate, and distribute oral hygiene aids better suited for LTOPs with limitations from physical disabilities to reduce high bacterial flora counts.
6. Provide oral care specialized educational courses for long-term older adult care providers.
7. Stay current with literature on best practice for older adults and oral health to keep LTCFs current through oral health education to staff involved in direct patient care.
8. Potentially decrease incidence of systemic health conditions by reducing overall bacterial floral counts intraorally.12,20-23
9. Advocate for interprofessional collaboration between RDHs, nursing staff, LTCF administrations, and dentists (Table 2).27,28,42,50,52
10. Expose necessary radiographs to provide dental hygiene diagnoses of oral diseases that cannot be detected clinically.
11. Assess the LTOP’s overall health, and refer to a necessary DDS or DMD when oral health may need further treatment beyond the scope of dental hygiene practice.
12. Advocate for specialized educational lectures and off-site clinical experiences in LTCFs within dental hygiene curriculum.65
13. Research US dental hygiene schools to determine what specialized education is currently being conducted for LTOPs.
14. Advocate through state legislation to allow more states, over the current 33, to provide direct access to care through integration of RDHs (Table 4).62
Conclusion
As LTOPs increase and inadequate oral care is recognized, opportunities for RDHs to become employed in the public health sector will increase.3 Because retained teeth positively correlates with overall health, RDHs are needed within LTCFs. Adequate oral care for LTOPs and education to administration and nursing staff on the expected positive outcomes of dental hygiene interventions is critical.8,13-18,26-32 Systemic health concerns commonly seen in the LTOP, with retained dentitions, are often correlated with poor oral care. RDHs can become better prepared to work with the LTOP by taking continuing education courses specializing in geriatric dentistry, public health, and institutional facilities. Also, RDHs are encouraged to stay current on legislative movements to find out when more access to care is granted in the state in which they practice. In the near future, government legislation may allow RDHs to work independently in LTCFs nationwide. Employing RDHs within LTCFs would not only provide access to oral care for LTOPs, but would offer support to LTCF staff, who are currently unable to fully meet oral health needs in this growing population.
About the Authors
Tracee S. Dahm, BSDH, MS, is a clinical practicing dental hygienist at LWSS Family Dentistry and an adjunct faculty member at the Gene W. Hirschfeld School of Dental Hygiene, Old Dominion University. Ann Bruhn, BSDH, MS, is an assistant professor at the Gene W. Hirschfeld School of Dental Hygiene, Old Dominion University. Margaret LeMaster, BSDH, MS, is an assistant professor and junior clinic coordinator at the Gene W. Hirschfeld School of Dental Hygiene, Old Dominion University.
References
1. U.S. Census Bureau. 2012 national population projections. [Internet]. Washington (DC): U.S. Census Bureau; 2014 December [cited 2015 July 10]. Available from: http://www.census.gov/population/projections/data/national/2012.html.
2. Dounis G, Ditmyer MM, McClain MA, et al. Preparing the dental workforce for oral disease prevention in an aging population. J Dent Educ. 2010;74:1086-1094.
3. U.S. Census Bureau. The older population: 2010-2010 census briefs. [Internet]. Washington (DC): U.S. Census Bureau; 2011 November [cited 2015 July 10]. 19 p. Available from: http://www.census.gov/prod/cen2010/briefs/c2010br-09.pdf.
4. Wiener JM, Freiman MP, Brown D. Nursing home care quality: twenty years after the omnibus budget reconciliation act of 1987 [Internet]. Menlo Park (CA): The Kaiser Family Foundation; 2007 December [cited 2015 July 10]. 53 p. Available from: https://kaiserfamilyfoundation.files.wordpress.com/2013/01/7717.pdf.
5. Reznick S, Matear DW. Perceptions of caregivers regarding the importance of dental care for institutionalised seniors: a pilot study. J R Soc Promot Health. 2002;122(3):170-174.
6. Chronic disease prevention and health promotion-oral health: Preventing cavities, gum disease, tooth loss, and oral cancers at a glance. Centers for Disease Control and Prevention [Internet]. 2011. [cited on 2012 March 12]. Available at: http://www.cdc.gov/chronicdisease/resources/publications/AAG/doh.htm.
7. Lost 6 or more teeth report. Centers for Disease Control and Prevention [Internet]. [cited on 2012 March 10]. Available at: http://apps.nccd.cdc.gov/nohss/ListV.asp?qkey=7&DataSet=2.
8. Sumi Y, Ozawa N, Miura H, et al. Oral care helps to maintain nutritional status in frail older people. Arch Gerontol Geriatr. 2010;51(2):125-128.
9. Gharat AR. Periodontitis and diabetes—a complex relationship. Int J Diab Dev Ctries. 2011;31(3):128-132.
10. Lam OL, Zhang W, Samaranayake LP, et al. A systematic review of the effectiveness of oral health promotion activities among patients with cardiovascular disease. Int J Cardiol. 2011;151(3):261-267.
11. Scannapieco FA. The oral microbiome: its role in health and in oral and systemic infections. Clinical Microbiology Newsletter. 2013;35(20):163-169.
12. Raghavendran K, Mylotte JM, Scannapieco FA. Nursing home-associated pneumonia, hospital-acquired pneumonia and ventilator-associated pneumonia: the contribution of dental biofilms and periodontal inflammation. Periodontol 2000. 2007;44:164-177.
13. Johnson EL, Brosseau JD, Soule M, Kolberg J. Treatment of diabetes in long-term care facilities: a primary care approach. Clin Diabetes. 2008;26(4):152-156.
14. Fravel MA, McDanel DL, Ross MB, et al. Special considerations for treatment of type 2 diabetes mellitus in the elderly. Am J Health Syst Pharm. 2008;68(6):500-509.
15. Patel MH, Kumar JV, Moss ME. Diabetes and tooth loss: an analysis of data from the National Health and Nutrition Examination Survey, 2003-2004. J Am Dent Assoc. 2013;144(5):478-485.
16. Heart Disease and Stroke Statistics 2008 Update. American Heart Association [Internet]. [cited 2012 February 12]. Available at: http://www.silverbook.org/browse.php?id=37.
17. Rose LF, Mealey B, Minsk L, Cohen DW. Oral care for patients with cardiovascular disease and stroke. J Am Dent Assoc. 2002;133(Suppl):37S-34S.
18. Persson RE, Hollender LG, Powell VL, et al. Assessment of periodontal conditions and systemic disease in older subjects II. J Clin Periodontol. 2002;29(9):803-810.
19. Mupparapu M, Kim IH. Calcified carotid artery atheroma and stroke: a systematic review. J Am Dent Assoc. 2007;138(4):483-492.
20. Sjogren P, Nilsson E, Forsell M, et al. A systemic review of the preventive effect of oral hygiene on pneumonia and respiratory tract infection in elderly people in hospitals and nursing homes: effect estimates and methodological quality of randomized controlled trials. J Am Geriatr Soc. 2008;56(11):2124-2130.
21. Sarin J, Balasubramaniam R, Corcoran A, et al. Reducing the risk of aspiration pneumonia among elderly patients in long-term care facilities through oral health interventions. J Am Med Dir Assoc. 2007;9(2):128-135.
22. Ishikawa A, Yoneyama T, Hirota K, et al. Professional oral health care reduces the number of oropharyngeal bacteria. J Dent Res. 2008;87(6):594-598.
23. Lampert NM, Tepper LM. Prevention of oral disease for long-term care and homebound elderly. N Y State Dent J. 2010;76(5):42-45.
24. Ettinger RL, O’Toole C, Warren J, et al. Nursing directors’ perceptions of the dental components of the Minimum Data Set (MDS) in nursing homes. Spec Care Dentist. 2000;20(1):23-27.
25. Adachi M, Ishihara K, Abe S, Okuda K. Professional oral health care by dental hygienists reduced respiratory infections in elderly persons requiring nursing care. Int J Dent Hyg. 2007;5(2):69-74.
26. Matear DW, Barbaro J. Caregiver perspectives in oral healthcare in an institutionalised elderly population without access to dental services: a pilot study. J R Soc Promot Health. 2006;126(1):28-32.
27. Wardh I, Hallberg LRM, Berggren U, et al. Oral health education for nursing personnel; experiences among specially trained oral care aides: one-year follow-up interviews with oral care aids at a nursing facility. Scand J Caring Sci. 2003;17(3):250-256.
28. Kullberg E, Sjogren P, Forsell M, et al. Dental hygiene education for nursing staff in a nursing home for older people. J Adv Nurs. 2010;66(6):1273-1279.
29. Family Caregiver Alliance National Center on Caregiving. Selected long-term care statistics [Internet]. San Francisco (CA): Family Caregiver Alliance; 2015 January 31 [cited 2015 July 12]. Available from: http://www.caregiver.org.
30. Lohrentz TD. The Americans with disabilities act [Internet]. Bethesda (MD): Depression and Bipolar Support Alliance; 2003 November [cited 2012 February 6]. 2 p. Available from: http://dbsanca.org/docs/ADA_Title_1_Employment.1782709.pdf.
31. Ettinger R. Oral health and the aging population. J Am Dent Assoc. 2007;138(Suppl):5S-6S.
32. Brukiene V, Aleksejūnienė J, Gairionyte A. Salivary factors and dental plaque levels in relation to the general health of elderly residents in a long-term care facility: a pilot study. Spec Care Dentist. 2011;31(1):27-32.
33. Gupta B, Marya CM, Juneja V, Dahiya V. Root caries: an aging problem. Internet J Dent Sci. 2007;5(1).
34. Chalmers JM, Ettinger RL. Public health issues in geriatric dentistry in the United States. Dent Clin N Am. 2008;52(2):423-466.
35. Araujo ACS, Gusmao ES, Batista JEM, Cimões R. Impact of periodontal disease on quality of life. Quintessence Int. 2010;41(6):111-118.
36. Carmona R. Ageism in healthcare: are our nation’s seniors receiving proper oral health care? Remarks before the special committee on aging United States Senate [Internet]. Washington (DC): United States Department of Health and Human Services; 2007 January 8 [cited 2011 December 31]. Available from: www.surgeongeneral.gov/news/testimony/ageism09222003.htm.
37. Mealey BL, Ocampo GL. Diabetes mellitus and periodontal disease. Periodontol 2000. 2007;44:127-153.
38. Bensing K. Oral care in elderly patients [Internet]. King of Prussia (PA): Advance Healthcare Network for Nurse Practitioners and Physicians Assistants; 2013 January 18 [cited 2013 October 13]. Available from: http://nurse-practitioners-and-physician-as-sistants.advanceweb.com/Features/Articles/Oral-Care-in-Elderly-Patients.aspx.
39. National Institute of Dental and Craniofacial Research. Oral health in America: a report of the Surgeon General (Executive Summary) [Internet]. Bethesda (MD): National Institute of Dental and Craniofacial Research; 2014 March 7 [cited 2011 November 1]. Available from: http://www.nidcr.nih.gov/datastatistics/surgeongeneral/report/executivesummary.htm
40. Jablonski RA, Swecker T, Munro C, et al. Measuring the oral health of nursing home elders. Clin Nurs Res. 2009;18(3):200-217.
41. Budtz-Jorgensen E, Mojon P, Banon-Clement JM, Baehni P. Oral candidiasis in long-term hospital care: comparison of edentulous and dentate subjects. Oral Dis. 1996;2(4):285-290.
42. Coleman P. Opportunities for nursing-dental collaboration: addressing oral health needs among elderly. Nurs Outlook. 2005;53(1):33-39.
43. Sura L, Madhavan A, Carnaby G, Crary MA. Dysphagia in the elderly: management and nutritional considerations. Clin Interv Aging. 2012;7:287-298.
44. Kanehisa Y, Yoshida M, Taji T, et al. Body weight and serum albumin change after prosthodontic treatment among long-term elderly in a long-term care geriatric hospital. Community Dent Oral Epidemiol. 2009;37(6):534-538.
45. Gil-Montoya JA, Subirá C, Ramón JM, Gonzalez-Moles MA. Oral health-related quality of life and nutritional status. J Public Health Dent. 2008;68(2):88-93.
46. Centers for Medicaid and Medicare Services. MDS 3.0 for nursing homes and swing bed providers [Internet]. Baltimore (MD): Centers for Medicaid and Medicare Services. 2015 March 6 [cited 2015 July 13]. Available from: http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/NHQIMDS30.html.
47. American Dental Association. Medicaid and Medicare [Internet]. Chicago (IL): American Dental Association. 1995-2014. [cited 2014 April 8]. Available from: http://www.ada.org/368.aspx.
48. American Dental Association. Paying for dental care: a how-to guide (incurred medical expenses) [Internet]. Chicago (IL): American Dental Association. [cited 2014 April 8]. Available from: http://www.ada.org/en/member-center/member-benefits/practice-resources/paying-for-dental-care-a-how-to-guide-incurred-med.
49. American Dental Hygienists’ Association. States which directly reimburse dental hygienists for services under the Medicaid program [Internet]. Chicago (IL): American Dental Hygienists’ Association. 2010 June [cited 2014 April 7]. 3 p. Available from: https://www.adha.org/resources-docs/7519_Direct_Reimbursement_Medicaid_by_State.pdf.
50. Howard RM, Sullivan DC. Survey of oral hygiene knowledge and practice among Mississippi nursing home staff. J Miss Acad Sci. 2011;56-57.
51. National Institute on Aging, U.S. Census Bureau. Dramatic changes in U.S. aging highlighted in new census, NIH report [Internet]. Bethesda (MD): National Institutes of Health; 2006 March 9 [cited 2015 July 13]. Available from: http://www.nih.gov/news/pr/mar2006/nia-09.htm.
52. Kaasalainen S, Ploeg J, McAiney C, et al. Role of the nurse practitioner in providing palliative care in long-term care homes. Int J Palliat Nurs. 2013;19(10):477-485.
53. Koh LC. Student attitudes and educational support in caring for older people: a review of literature. Nurse Educ Pract. 2012;12(1):16-20.
54. Michaud PL, de Grandmont P, Feine JS, Emami E. Measuring patient-based outcomes: is treatment satisfaction associated with oral health related quality of life? J Dent. 2012;40(8):624-631.
55. Wyatt CC. A 5-year follow-up of older adults residing in a long-term care facilities: utilization of a comprehensive dental programme. Gerodontology. 2009;26(4):282-290.
56. Coleman P. Collaboration of nursing and dentistry [Internet]. Milwaukee (WI): Geriatric Oral Health. 2015. [cited 2015 July 13]. Available from: http://www.geriatricoralhealth.org/topics/topic07/default.aspx.
57. Medicare. U.S. department of health and human services [Internet]. [cited 2012 February 3]. Available at: http://www.medicare.gov/longtermcare/static/home.asp.
58. Wårdh I, Hallberg LR, Berggren U, et al. Oral health care—a low priority in nursing. In-depth interviews with nursing staff. Scand J Caring Sci. 2000;14(2):137-142.
59. Health & Drug Plans [Internet]. [cited 2011 October 25]. Available at: http://www.medicare.gov/default.aspx.
60. Berenson RA, Horvath J. Confronting the barriers to chronic care management in Medicare. Health Aff (Millwood). 2003; Suppl Web Exclusives: W3-37-53.
61. Synopses of State Public Health Dental Programs. Summary Report for Association of State and Territorial Dental Directors [Internet]. 2011-2012 [cited 2013 October 13]. Available from: www.astdd.org/docs/state-synopsis-report-summary.pdf
62. American Dental Hygienists’ Association. Direct access states [Internet]. Chicago (IL): American Dental Hygienist Association. 2014 June [cited 2015 July 13]. 14 p. Available from: www.adha.org/resources-docs/7513_Direct_Access_to_Care_from_DH.pdf
63. Marsh LA. Dental hygienist attitudes toward providing care for the underserved population. J Dent Hyg. 2012;86(4):315-322.
64. Best H. Educational systems and the continuum of care for the older adult. J Dent Educ. 2010;74(1):7-12.
65. Dolan TA. Access to dental care for older Americans. N Y State Dent J. 2010;76(5):34-37.
66. Commission on Dental Accreditation. American Dental Association. [Internet]. 2013. [cited 2014 April 7]. Available at: http://www.ada.org/sections/educationAndCareers/pdfs/dh.pdf
67. Fried J. Interprofessional collaboration: if not now, when? J Dent Hyg. 2013;87(Suppl 1):41-43.