You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
INTRODUCTION
Oral Health Practitioners and Tobacco Interventions: A Perfect Match
Approximately 20% of the US population uses tobacco.1 Each day, nearly 4,000 US youth smoke their first cigarette.2,3 From 2000 to 2004 cigarette smoking was estimated to be responsible for $193 billion in annual health-related economic losses including nearly $96 billion in medical costs and $97 billion in lost productivity.4 Approximately 70% of all smokers desire to quit.5
Healthcare providers have a vital role to play in helping users of both smoking and smokeless (spit) tobacco quit; tobacco interventions delivered by clinicians, including dental professionals, can increase abstinence rates.6-8 As such, the US Public Health Service (USPHS) Clinical Practice Guideline, Treating Tobacco Use and Dependence, recommends that all clinicians provide tobacco interventions.7 As a primary healthcare provider, dental professionals are often able to establish and maintain trusting patient relationships which helps create a safe environment for discussing the topic of tobacco use. Nevertheless, although dental office tobacco prevention and treatment efforts can increase tobacco abstinence, they are underutilized.9,10 Both students and practicing dental hygienists have cited both a lack of confidence and intervention skills training as reasons for not providing tobacco interventions.11,12
Tobacco dependence education should be integral to healthcare professionals’ education and clinical training. However, a survey of dental hygiene educators found faculty were only moderately confident in teaching tobacco dependence education, and their curricula lacked instruction on brief motivational interviewing, pharmacotherapy, or establishing a tobacco control program in the dental practice.13 Likewise, barriers to integrating tobacco dependence education in predoctoral curricula included a lack of integration between didactic content and clinical practice, and a failure to provide supportive intervention skills.14 Other studies found that the reported lack of faculty time, student interest, current materials, and a perceived lack of faculty expertise were reasons for not fully integrating tobacco cessation strategies into patient care.15,16
The American Dental Association (ADA) recognizes the dental hygienist as an appropriate team member to provide tobacco cessation interventions. The ADA lists tobacco cessation counseling under Section II 3.3.2, Provision of Clinical Dental Hygiene Services and is also in the American Dental Hygienists Association (ADHA) Standards of Clinical Practice documents.17,18 The ADHA has also contributed to the promotion of dental hygienists as tobacco cessation experts. Following a Robert Wood Johnson Foundation sponsored summit and a grant award in November 2003, the ADHA has continued its dedication to oral and systemic health by the concerted efforts of registered dental hygienists focusing on tobacco dependence treatment. The ADHA explains that it is “proud to make such a positive impact on the oral and overall health of the public by encouraging dental hygienists to help smokers quit.”19 The grant assisted the ADHA to offer a nationwide campaign designed to promote a smoking cessation intervention and additional educational materials to Association members. Its goal was to increase the percentage of dental hygienists that screen clients for tobacco use.19 Further, the grant allowed for the development of an educational program (Ask. Advise. Refer.), designation of points of contact in each state for technical assistance and expertise who would also serve as the Smoking Cessation Initiative Liaison and creation of a dedicated website (www.askadviserefer.org). The ADHA reports that the objectives are to “further establish dental hygienists as advocates of cessation intervention and to place dental hygiene on the frontline of smoking cessation intervention.”19
National Tobacco Control Program
In 1999, the Center for Disease Control (CDC) and Prevention Office on Smoking and Health created the National Tobacco Control Program to encourage a coordinated, national effort to reduce tobacco-related morbidity and mortality. The program provides funding and technical support to state and territorial health departments. National Tobacco Control Program funding aims to achieve the objectives outlined in the CDC’s Best Practices for Comprehensive Tobacco Control Programs 2007, an evidence-based guide to help states plan and establish effective tobacco control programs.20
Indiana Tobacco Prevention and Cessation Commission
The vision of the Indiana Executive Board of the Tobacco Use Prevention and Cessation Commission Trust Fund was to significantly improve the health of all Indiana residents by reducing the negative health and economic impact of tobacco use. The Tobacco Use Prevention and Cessation mission is “to prevent and reduce the use of all tobacco products in Indiana and to protect citizens from exposure to tobacco smoke.”21 On July 1, 2011, the Tobacco Use Prevention and Cessation became part of the Indiana State Department of Health. While its mission is unchanged, one overarching goal is to mobilize stronger partner coalitions that reflect the Tobacco Use Prevention and Cessation targeted population groups and support its program objectives. The Board allocates resources from the Trust Fund to accomplish this goal.21
Indiana University School of Dentistry Tobacco Cessation & Biobehavioral Group
Established in 2006 from a university-sponsored grant, the Tobacco Cessation & Biobehavioral Group’s mission has three components: research, education, and cessation. The research component involves biomedical, behavioral, and educational research. The education and cessation components focus on graduating students and researchers with extensive education about smoking and spit tobacco and the health effects, training health professionals to provide tobacco-using patients with evidence-based information and treatment, and offering tobacco cessation counseling.22
However, dental practitioners with limited time and resources can assist tobacco-using patients who are interested in quitting by referring them to a tobacco quitline.23 Quitline referrals and subsequent in-depth counseling from quitline personnel is an effective strategy for increasing cessation rates.24 Quitline referral by dental practitioners is a feasible strategy for assisting patients to quit tobacco in all its forms if efficient links between the dental practice and the quitline can be established.23 Patients receiving telephone counseling quit tobacco use at higher rates, but only a small percentage of those proactively referred actually receive counseling.23 Nonetheless, training practitioners to provide brief tobacco interventions may result in a behavior change among practitioners, enabling them to be more effective in helping their patients quit tobacco.25
With this in mind, Tobacco Cessation & Biobehavioral Group members of the Indiana University School of Dentistry (IUSD) developed and delivered a 7-hour continuing education program for Indiana oral health practitioners to improve their knowledge, confidence, and skills in providing tobacco cessation interventions to their patients. The program was funded by multiple grants (2008 to 2010) from the Tobacco Prevention and Cessation Commission of the Indiana State Department of Health and was implemented in collaboration with the Indiana Dental Hygiene Association and Tobacco Prevention and Cessation community partners.
It was anticipated that after participating in the continuing education program, attendees would increase their knowledge on tobacco dependence and treatment and would actively apply their learning to clinical practice. This project aimed to assess the effectiveness of the tobacco education program at enhancing attendees’ knowledge of tobacco’s addictive nature and associated health effects, pharmacotherapeutic and behavioral tobacco interventions, local and statewide tobacco cessation referral resources, and the components and protocols for establishing a team-based approach for tobacco interventions in the dental office, as well as obtain information on the extent to which program participants’ integrated course concepts and strategies into practice.
METHODS AND MATERIALS
Program Development
The Indiana Dental Hygiene Association representatives and Tobacco Cessation & Biobehavioral Group study investigators selected 11 Indiana sites for the continuing education program based on the highest tobacco use rates by county as reported by Indiana Tobacco Prevention and Cessation. Continuing education program brochures that included registration information were mailed to all licensed dental and dental hygiene professionals in zip codes within a 50-mile radius of each selected continuing education site. The program provided 7 hours of continuing education credit towards Indiana licensure and was offered free of charge.
Program content was based on the Mayo Clinic’s Nicotine Dependence Treatment Program and the USPHS Clinical Practice Guideline, Treating Tobacco Use and Dependence.7 Program topics included: Nicotine Dependence 101, Oral Health and Tobacco (from molecular to clinically evident effects of tobacco on oral tissues), Pharmacotherapy and Cessation Aids, Behavioral Interventions, A Team-Based Office Model for Implementing a Tobacco Cessation Program, and Indiana Tobacco Prevention and Cessation Community Partners and Resources. Interventional strategies emphasized the 5 A’s protocol (Ask patients about tobacco use, Advise them to quit, Assess willingness to quit, Assist in the quit attempt, and Arrange for follow-up), and the Ask-Advise-Refer protocol. The program’s learning objectives included:
• Describe and recognize the oral and systemic effects of tobacco use
• Evaluate available efficacy and safety data on new and emerging tobacco cessation therapies
• Apply an individualized tobacco cessation quit-plan that maximizes the likelihood of treatment success
• Identify planning, maintenance, therapy, resources and referral sources, and follow-up to prevent relapse and promote long-term cessation success
• Identify tobacco cessation referral resources, and meet with county Tobacco Prevention and Cessation representatives of the Indiana State Department of Health
Measures
An initial post-continuing education survey and 3-month follow-up survey were developed to capture the attendees’ self-reported knowledge and tobacco intervention activities at two points in time. To establish content validity, each survey was piloted with a small group of IUSD faculty, and surveys were modified based on their feedback. The 18-item initial post-continuing education survey contained items regarding demographics, content knowledge acquisition, and respondents’ intention to apply concepts to patient care. The survey contained multiple-choice items with dichotomous (yes/no) or scaled response choices (strongly agree, agree, undecided, disagree, strongly disagree). There was also one open-ended item (if you do NOT plan to refer patients to the Indiana quitline, please tell us why). Five of the survey items were directed solely to dentist attendees. These were:
1. Do you plan to provide, or continue to provide, patients with tobacco cessation literature in your dental practice?
2. If you plan to provide (or plan to continue to provide) tobacco cessation resources, how will you provide those resources?
3. For what reasons might you NOT plan to provide tobacco cessation resources in your practice or be UNSURE about providing such literature?
4. Do you plan for your practice to refer patients who are interested in community cessation resources and/or the Indiana Quitline?
5. If you do NOT plan to refer patients, please tell us why.
The 3-month follow-up survey contained 14 items concerning demographics, participants’ self-reported implementation of intervention strategies discussed during the continuing education program and perceived barriers to implementation. The follow-up survey gathered information about attendees’ progress in implementing a team-based tobacco cessation program into the dental setting. Item formats were similar to the initial survey; however, there were four open-ended items and one question directed solely to dentists (I am prescribing pharmacological agents for tobacco cessation to my patients who want to quit using tobacco). Approval for this research project was obtained by the Indiana University Purdue University Indianapolis Institutional Review Board.
Procedures
During the continuing education program, the study was explained to attendees and they were offered the opportunity to participate by agreeing to provide their contact information, and complete the initial and 3-month follow-up surveys. At the conclusion of each program, participants were asked to complete the initial post-continuing education survey. At 3 months following each program, the follow-up survey was mailed or delivered electronically to those who had previously consented to participate and had completed the initial survey. A contact information form, attached to the initial survey, was used to mail 3-month follow-up surveys and survey completion reminders to non-responders. A maximum of three contact attempts were made to complete the 3-month surveys (the initial contact and two subsequent mailings were sent to non-responders). The survey was confidential; however, to track completion, both the contact information form and the surveys were coded with the same numerical identifier. Survey data were reviewed, coded, entered into an electronic database, and analyzed as de-identified aggregate data using descriptive statistics including frequencies and percentages. Open-ended responses were categorized into themes for analysis.
RESULTS
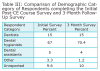
A total of 626 individuals attended the 11 continuing education programs. Of the attendees who completed the initial survey (n = 565), approximately 70% were dental hygienists, 25% were dentists and other allied health professionals, and the remainder did not identify their profession (Table 1). Mean response rate for all individuals in the initial survey was 91%.
The results of the scaled items from the initial survey are shown in Table 2. The majority of the attendees’ responded “Strongly Agree” or “Agree” to the statements concerning their understanding of course concepts and intention to integrate course content in their practice. Knowledge gained and/or confidence in applying that knowledge was highest in the following topics: tobacco’s oral effects, nicotine addiction, effects of pharmacotherapy, communication strategies, and tobacco cessation resources. Some survey items generated less certainty among respondents; principally, confidence in their knowledge about dosing and adverse effects of cessation pharmacotherapy, and intention to take an active role in the implementation of a team-based tobacco intervention plan in their practice.
Dentists were asked to complete the final five items. Of 119 dentist respondents, 28% (33) indicated that they currently provide tobacco cessation literature in their practice and planned to continue doing so, while 60% (71) stated that they planned to provide such literature, and 13% (15) stated they were unsure if they would provide tobacco cessation literature in their office. Of those dentists who currently provide or planned to provide literature in their office (n = 104), tobacco cessation resources are/would be presented as: reception area literature display (86), treatment area literature display (86), reception area video (7), treatment area video (18), and office website with links (17). Of materials to be distributed directly to patients, dentists indicated that they are/would be distributed by multiple individuals, including the dental hygienist (87), dentist (69), assistant (59), and other personnel (17).
When asked why they might not plan to provide or are unsure about providing tobacco cessation resources/literature in their practice, dentists (n = 126) indicated the following reasons: lack of time to discuss resources (23), lack of time to distribute resources (20), patient acceptance of resources (15), concerns about cost of resources (13), space for resources (10), locating/obtaining appropriate resources (8) and lack of referral agencies in my area (8). Other reasons indicated for not planning to provide tobacco cessation resources included: retired/unemployed/not practicing status, working in a research environment, and my (employer’s) permission is required.
Of the 126 respondents who answered the survey item “Do you plan for your practice to refer patients who are interested in community cessation resources and /or the Indiana Quitline,” 90% (113) indicated that they currently were or planning to refer patients, 8% (10) were unsure if they would make such referrals, and 3% (4) indicated that did not intend to refer patients to the Quitline and local Tobacco Prevention and Cessation resources.
Three-Month Post-Continuing Education Follow-up Survey
Although the response rate varied by location, the completed follow-up surveys were returned by 250 individuals, resulting in a mean response rate of 40% (Table 1). The professions of the 3-month survey respondents were proportionally similar to those completing the initial survey (Table 3).
In response to the statement, “I am personally using the communication strategies learned in the course when talking to patients about tobacco use,” participants (n = 233) responded as follows: strongly agree (12.4%, 29), agree (66.5%, 155), undecided (15%, 35), disagree (4.7%, 11), and strongly disagree (1.2%, 3).
Table 4 details the respondents’ referral of patients to the local Tobacco Prevention and Cessation community partners and the Indiana tobacco quitline for counseling as well as their reasons for not making such referrals. Practitioners appeared to favor referrals to the Indiana quitline over local Tobacco Prevention and Cessation counselors.
Participants’ responses to items regarding the extent to which they had implemented the tobacco interventional strategies discussed in the course are described in Table 5. Additionally, participants were asked to provide examples of how they accomplished implementation of the tobacco intervention with patients in their office. Seventy-five write-in responses were provided; the following are a sample of these comments:
• “Inquire about patient’s previous cessation times. Inform patients of dental and medical health problems associated with smoking. Give patient info and contact options.”
• “Ask patient if they desired to not smoke. If yes, then describe the quit line and other options available. Depending on their response, gave the patient the appropriate materials.”
• “For every patient I ask about tobacco use (what kind, how long they have used, if they have considered quitting), I advise them to quit and refer to the quit line or physician.”
Participants were also asked to provide an example of one challenge they have encountered in integrating a tobacco cessation intervention into their office routine. Of the 89 responses received, the most common themes were: lack of patient interest/compliance, time, and difficulty getting staff involved. Thirty-three responses were received for the final item, “If you have not implemented a tobacco cessation intervention plan or do not intend to, why not?” The most common reasons given were: lack of interest/approval from the dentist in the practice, lack of time to discuss or implement a plan, and that the respondent was not currently in active practice/employed.
DISCUSSION
As tobacco use is a well-known risk factor for a myriad of oral and maxillofacial conditions, addressing patient tobacco use is a part of preventive dental practice and advising patients to quit is a professional responsibility of the dental team. In general, tobacco users expect and are comfortable receiving such advice.24,25 Campbell et al found that most patients believed that dental offices should provide tobacco interventions, and support for such was equal between tobacco users and non-users.26 Further, a recent systematic review concluded that brief tobacco use cessation counseling conducted by oral health professionals was found to be effective at 12 months or longer.27 However, dental professionals have been largely inactive in direct counseling of patients to quit tobacco.28 Major constraints cited against the implementation of tobacco counseling in oral healthcare settings include suboptimal attitudes, insufficient training, and lack of reimbursement.29-32
The continuing education program described here sought to enhance Indiana oral healthcare providers’ understanding of tobacco dependence and treatment and encourage them to provide tobacco cessation interventions. The program reached over 600 practitioners, primarily dental hygienists whose role focuses on patient education and disease prevention. In the short-term, the program appeared to be effective at increasing attendees’ knowledge, especially on tobacco’s oral health effects, nicotine addiction, and how tobacco cessation medications work.
Participants indicated that the program was effective in teaching communication strategies to employ with tobacco users; this should have improved attendees’ confidence in approaching patients about quitting tobacco. Immediately after the program, nearly 98% of participants planned to use these communication techniques in practice. However, 3 months later, enthusiasm for applying these communication strategies seemed to decrease: 78% reported applying these skills, 15% were undecided, and 6% were not employing them in patient interactions.
Immediately post-program, nearly 90% of dentists indicated that they provided or planned to provide patient tobacco cessation resource materials, primarily in treatment or reception rooms. Although materials were distributed by multiple personnel, the dental hygienist and dentist were primary. Findings were similar at follow-up. The principal barriers to providing patient resources were a lack of time to discuss and distribute materials to patients, lack of patient acceptance, the cost of materials, and difficulty locating and obtaining resources. This finding was problematic because the continuing education program provided numerous free resources (educational posters, pamphlets, quitline information, etc.) to attendees and links to the Indiana State Department of Health Tobacco Prevention and Cessation Commission website where a plethora of patient referral and education materials could be obtained at no charge.
Immediately post-program, participants reported enhanced awareness of tobacco cessation referral resources, and the majority (90%) planned to refer patients to county Tobacco Prevention and Cessation counselors or the Indiana quitline. At follow-up, only 60% and 40% reported making referrals to the quitline and Tobacco Prevention and Cessation counselors, respectively. The Ask-Advise-Refer approach with quitline referral was the most popular interventional strategy, probably due to its efficiency. Unfortunately, the more proactive “FAX to Quit” strategy (faxing patient information to the quitline and allowing a quitline counselor to begin patient counseling within 48 hours) was reportedly used by very few practitioners. The reasons for not referring to Tobacco Prevention and Cessation counselors included use of the quitline instead, patient lack of interest in counseling, and misplacing Tobacco Prevention and Cessation counselor contact information. Although the continuing education program provided clinicians the opportunity to meet their county Tobacco Prevention and Cessation partner and obtain their contact and service information, some clinicians may have found that patients preferred the quitline’s convenience or anonymity over in-person counseling.
Although the CE program appeared to increase participants’ knowledge of cessation pharmacotherapy, immediately after the program at least 10% of the participants did not feel confident in their knowledge of the dosing or adverse effects of the medications discussed. This suggests the program did not adequately address this issue, and may explain, in part, why at 3 months very few dentists reported recommending/prescribing tobacco cessation medications to their patients.
Despite emphasis during the course, even immediately after the continuing education program, nearly 25% of attendees did not plan to take an active role in implementing a tobacco cessation program in their office. At 3 months, relatively few participants reported adopting specific formal office protocols and practices for providing tobacco interventions with patients.
Teaching oral healthcare professionals about tobacco use and dependence, and how to implement tobacco cessation interventions, does not necessarily ensure that they will change their practice behaviors and begin to utilize the learned concepts and skills with their patients. This continuing education program emphasized the “team approach” to tobacco cessation interventions that outlined suggested roles and responsibilities for each member of the dental team, including the dentist, dental hygienist, assistant, and non-clinical staff. First suggested in Christen’s how-to model, most cessation programs conducted in dental offices stress the pivotal role of the team care approach that involves all dental practice members.33 Among the keys to success, working as team where all staff are involved and invested in the program, and identifying an office champion (coordinator) who has overall responsibility for the program can make a positive impact in enhancing patients’ quit attempts.26,34 As the dental hygienist typically has more patient contact time than the dentist, and has the most training and expertise as an oral health educator, it is recommended that the dental hygienist serve as the coordinator of the office tobacco cessation program. Given that healthcare is moving toward an interprofessional model of care delivery, dental hygienists may have more opportunities to work in a variety of settings as part of a healthcare team. Their expertise in educating patients and their families on the connection between oral and systemic health and the impact of tobacco use on oral health, and motivating patients in adopting healthy behaviors allows them to provide a unique and vital contribution to the healthcare team.
This study had several limitations, most notably the self-report nature of the survey and a decrease in response rate from the initial survey to the 3-month follow-up survey. However, demographically, initial and follow-up participants had similar characteristics. Another limitation was an inability to systematically track participant referrals to the quitline or Tobacco Prevention and Cessation counselors and, ultimately, obtain information on patient quit rates other than anecdotal, self-report information. Further, survey results revealed some potential areas for improvement in the continuing education program itself. The pharmacotherapy section of the course may need to be revised for better participant comprehension, and include an open discussion of perceived barriers to the use of pharmacotherapy strategies. Although the continuing education program contained interactive components and question and answer periods, more role-playing and active learning techniques could be employed to further enhance skill development.
As Berwick noted, it is helpful to understand not only whether interventions work but in what context.35 Amemori compared the effect of an educational intervention on increases in provision of patient tobacco interventions by Finnish dentists and dental hygienists’ across three study groups: control group, those who received tobacco dependence education and cessation training, and a group that received tobacco dependence education/cessation training with monetary compensation for cessation counseling that was provided.36 Findings revealed that the educational session was effective in increasing providers’ self-efficacy and skills in counseling.36 Compared to dentists, dental hygienists were more active in counseling and their counseling performance showed greater increases in cessation numbers in both intervention groups. However, similar to the present study, the educational intervention’s positive effects on clinician tobacco cessation activities faded rapidly two months post-continuing education course. Remarkably, compared to tobacco dependence education/cessation training alone, the incentive of receiving payment for counseling did not result in increased practitioner tobacco intervention activities. Future studies should focus on identifying what factors, beyond knowledge acquisition, enhance oral healthcare providers’ motivations and willingness to engage in tobacco cessation interventions.
CONCLUSION
Providing oral health professionals with education in tobacco use and cessation strategies, as well as patient education materials and tobacco cessation referral information and resources (eg state-funded tobacco quitline) may encourage them to provide brief tobacco interventions as a routine part of practice. Providing this service to their patients illustrates how oral health professionals can function as an interdisciplinary team. Dentistry should function as part of an interprofessional healthcare team with the goals of integrated health promotion and holistic care for every individual. Continuing education opportunities regarding tobacco dependence and treatment, including the ability to connect with local tobacco cessation resources, should be made available. Oral healthcare practitioners with appropriate training can contribute to finding a solution to the problem of tobacco use and dependence.
About the Authors
Lorinda Coan LDH, MS, is an assistant professor of dental hygiene at the University of Southern Indiana. L. Jack Windsor, PhD, is an associate professor in the Department of Oral Biology at the Indiana University School of Dentistry. Laura M. Romito, DDS, MS, is an associate professor and director of the Nicotine Dependence Program at the Indiana University School of Dentistry, and is also an associate professor, Department of Oral Biology, at the Indiana University School of Dentistry.
Acknowledgments
The authors acknowledge the support of the Indiana Tobacco Prevention and Cessation Commission and all local TPC community partners who participated in the CE program. We thank our collaborators and colleagues at the Indiana Dental Hygienists’ Association, as well as staff and faculty colleagues of the Indiana University School of Dentistry Tobacco Cessation and Biobehavioral Group, particularly Dr. Arden Christen, whose support and participation were vital to this project.
References
1. Centers for Disease Control and Prevention (CDC). Current Cigarette Smoking Among Adults—United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61(44):889-894.
2. Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings. Substance Abuse and Mental Health Services Administration [Internet]. 2011 [cited 2013 November 5] Available from: http://www.samhsa.gov/data/NSDUH/2k10Results/Web/HTML/2k10Results.htm#Ch4.
3. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Office on Smoking and Health. 2012.
4. Centers for Disease Control and Prevention. Smoking-Attributable Mortality, Years of Potential Life Lost, and Productivity Losses—United States, 2000–2004. MMWR Morb Mortal Wkly Rep. 2008;57(45):1226-1228.
5. Centers for Disease Control and Prevention. Quitting Smoking Among Adults—United States, 2001–2010. MMWR Morb Mortal Wkly Rep. 2011;60(44):1513-1519.
6. Fiore MC, Bailey WC, Cohen SJ, et al. Treating tobacco use and dependence: 2008 guideline. U.S. Department of Health and Human Services, Public Health Service. 2000.
7. Tobacco Use and Dependence Guideline Panel. Treating Tobacco Use and Dependence: 2008 Update. U.S. Department of Health and Human Services. 2008.
8. Carr AB, Ebbert J. Interventions for tobacco cessation in the dental setting. Cochrane Database Syst Rev. 2012;6:CD005084.
9. Needleman IG, Binnie VI, Ainamo A, et al. Improving the effectiveness of tobacco use cessation (TUC). Int Dent J. 2010;60(1):50-59.
10. Studts JL, Burris JL, Kearns DK, et al. Evidence-based tobacco cessation treatment by dental hygienists. J Dent Hyg. 2011;85(1):13-21.
11. Brame JL, Martin R, Tavoc T, et al. A randomized controlled trial of the effect of standardized patient scenarios on dental hygiene students’ confidence in providing tobacco dependence counseling. J Dent Hyg. 2012;86(4):282-291.
12. McCartan B, McCreary C, Healy C. Attitudes of Irish Dental, Dental Hygiene, and Dental Nursing Students and Newly Qualified Practitioners to Tobacco Use Cessation: A National Survey. Eur J Dent Educ. 2008;12(1):17-22.
13. Davis JM, Stockdale MS, Cropper MS. The need for tobacco education: studies of collegiate dental hygiene patients and faculty. J Dent Educ. 2005;69(12):1340-1352.
14. Spangler JG, George G, Foley LK, Crandall SJ. Tobacco intervention training: current efforts and gaps in U.S. medical schools. JAMA. 2002;288(9):1102-1109.
15. Barker GJ, Williams KB. Tobacco use cessation activities in U.S. dental and dental hygiene student clinics. J Dent Educ. 1999;63:828-833.
16. Weintraub TA, Saitz R, Samet JH. Education of preventive medicine residents: alcohol, tobacco, and other drug abuse. Am J Prev Med. 2003;24(1):101-105.
17. American Dental Association Commission on Dental Education. Accreditation standards for dental hygiene education programs. American Dental Association [Internet]. 2006. [Cited 2006 June]. Available from: http://www.ada.org/~/media/coda/files/dh.ashx.
18. American Dental Education Association. Exhibit 5: ADEA policy statements. J Dent Educ. 2004;68(7):729-744.
19. Dental hygienists supported in national effort to help smokers quit: third year grant awarded from Robert Wood Johnson Foundation. American Dental Hygienists’ Association [Internet]. 2005 [cited 2012 June]. Available from: http://www.adha.org/media/releases/archives/2005/12012005_rwj.htm.
20. Best Practices for Comprehensive Tobacco Control Programs—2007. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. 2007.
21. Tobacco Use Prevention and Cessation Commission. Indiana State Department of Health [Internet]. 2012 [cited 2012 June 19]. Available from: http://www.in.gov/isdh/tpc/index.htm.
22. Information page. Indiana University Tobacco Cessation Biobehavioral Group [Internet]. 2012 [cited 2012 June 19]. Available from: http://tcbg.iusd.iupui.edu.
23. Ebbert JO, Carr AB, Patten CA, et al. Tobacco use quitline enrollment through dental practices. A pilot study. J Am Dent Assoc. 2007;138:595-601.
24. Gordon JS, Andrews A, Crews K, et al. The 5 A’s vs 3A’s plus proactive quitline referral in private practice dental offices: preliminary results. Tob Control. 2007;16:285-288.
25. Gordon JS, Andrews JA, Crews KM, et al. Do faxed quitline referrals add value to dental office-based tobacco-use cessation interventions? J Am Dent Assoc. 2010;141(8):1000-1007.
26. Campbell HS, Sletten M, Petty T. Patient perceptions of tobacco cessation services in dental offices. J Am Dent Assoc. 1999;130:220-226.
27. Carr AB, Ebbert JO. Interventions for tobacco cessation in the dental setting. A systematic review. Community Dent Health. 2007;24:70-74.
28. Gordon JS, Lichtenstein E, Severson HH, Andrews JA. Tobacco cessation in dental settings: research findings and future directions. Drug Alcohol Rev. 2006;25:27-37.
29. Rosseel JP, Jacobs JE, Hilberink SR, et al. What determines the provision of smoking cessation advice and counseling by dental care teams? Br Dent J. 2009;206:E13.
30. Trotter L, Worcester P. Training for dentists in smoking cessation intervention. Aust Dent J. 2003;48:183-189.
31. Helgason AR, Lund KE, Adolfsson J, Axelsson S. Tobacco prevention in Swedish dental care. Community Dent Oral Epidemiol. 2003;31:378-385.
32. Amemori M, Korhonen T, Kinnunen T, et al. Enhancing implementation of tobacco use prevention and cessation counseling guideline among dental providers: a cluster randomized controlled trial. Implemen Sci. 2011;6:13.
33. Christen AG, Mc Donald JL, Klein JA, et al. How-to-do-it quit smoking strategies for the dental office team: an eight-step program. J Am Dent Assoc. 1990;120:20S-27S.
34. Smith SE, Warnakulasuriya KAAS, Feyerabend C, et al. A smoking cessation programme conducted through dental practices in the UK. Br Dent J. 1998;185:299-303.
35. Berwick DM. The science of improvement. JAMA. 2008;299:1182-1184.
36. Amemori M, Virtanen J, Korhonen T, et al. Impact of educational intervention on implementation of tobacco counselling among oral health professionals: a cluster-randomized community trial. Community Dent Oral Epidemiol. 2013;41:120-129.